1. Introduction
Low birth weight (LBW) either as a result of intrauterine growth restriction or prematurity is a major cause of perinatal mortality and adult cardiovascular and cognitive morbidity [1,2]. The burden of LBW is much greater in Low and Middle Income Countries (LMICs). Worldwide, about 20 million children are born with low birth weight, about 95 % in developing countries. [3] There are multiple maternal factors including: antenatal nutritional status, weight gain and caloric intake during pregnancy, socioeconomic status, parity and chronic illnesses of mother [4-6]. The role of micronutrient supplementation has been extensively assessed by a number of high quality trials which have (largely) shown positive albeit small effects birth weight [7,8].
The effect from protein energy supplementation in undernourished women in LMICs is more controversial. High protein intake during pregnancy has shown negative effect in some studies [9] and even isocaloric protein diet has no proven benefit to mother or infant[10]. However, recent systematic review and meta-analysis of 7 trials ( 2,367 women) showed a that balanced proteinenergysupplementation significantly improved birth weight (d = 0.20, 95% confidence interval, 0.03-0.38, P = 0.02). There was, however, no effect on birth length or birth head circumference [11].
Pakistan is a developing country with high burden of malnutrition in women of child bearing age and infants. Surveillance work in Sind suggests a maternal mortality rate of 320/ 100, 000 live births well above the WHO national estimate for Pakistan of 260/ 100,000[12]. One of the reasons for this high mortality rate is likely to be the prevalence of malnutrition among women which is largely attributed to poverty and social practices. A variable perinatal mortality rate (PMR) for Pakistan is reported in a local study from 63-92/1000 births which is again far higher than in many developed countries where the PMR is typically between 4 and 6/1,000 [13]. This high PMR has multiple reasons and low birth weight is a leading cause. An old study has shown mean birth weight in Pakistan to be 2910 gms[14] but this data is for hospital born babies and it is expected to be much lower for babies born in Peri urban slums.
We aimed to assess the effectiveness of high calorie dense food in the form of biscuits over a regular diet augmented by flour and oil in under nourished pregnant women (BMI ≤19.9) offered from 14 completed weeks of gestation until delivery.We hypothesized that offering energy dense biscuits rich in calories and micronutrients would enhance maternal and fetal weight gain in our setting and also result in adherence to multiple micronutrient (MMN) supplementation which is difficult to achieve in the form of tablets.
2. Methods
2.1 Trial Location and Population
The trial was conducted at two poor peri urban settings of Karachi, Ali Akbar Shah (AG) and Bhains Colony (BH) in Bin Qasim Town, with total populationof 64,834 people. There is a well-established demographic surveillance system (DSS) in these areas which collects information on vital statistics on a quarterly basis. The baseline Neonatal mortality rate (NMR) is 38 per 1,000 live births at Ali Akbar Shah while at Bhains Colony it is 35 per 1000 live births. There are AKU run primary health care centers in each of these sites which provide free of cost health services and immunization to children aged less than 5 years and pregnant women. The date of the last menstrual period (LMP) was used to calculate gestational and all undernourished pregnant femalesbased on low body mass index (BMI) (defined as BMI < 19.9 kg/ m2) identified before 14 weeks of gestation through the surveillance system were offered enrollment. The demographic surveillance team visit every block of catchment area every three monthly to detect early pregnancy. Women with chronic illness (cardiovascular disease, diabetes, renal disease, and hypertension), those with history of multiple abortions (three or more abortions), females identified as having twin/triplet pregnancies proved by ultrasound scans done earlier or those already enrolled in any other study were excluded.
3. Design and Intervention
3.1 Open label randomized controlled trial with 2 arms
Intervention Arm: Dietary supplementation with high energy biscuits containing multiple vitamins and calcium in the recommended allowance (RDA) for pregnant women (table 1).
Control arm: Supplementation with Wheat flour and oil.
For this project English Biscuit manufacturers (EBM, Karachi, Sindh), a local manufacturing company, agreed to provide specially formulated biscuits with micronutrients for pregnant women.
The composition of energy rich biscuits and comparison with recommended daily allowance (RDA) is shown in Table 1. While each gram of wheat flour has 339 Kcal, carbohydrates 72.5 gm, Fat 1.8 gm, Protein 13.7 gm, B1 0.4 mg, B2: 0.21 mg, B3 6.36, B5 1 mg, B6 0.34 mg, Folic acid 44 ug, Calcium 34 mg, Iron 3.8 mg and Zinc 2.93 mg.(https://ndb.nal.usda.gov/ndb/foods/show/6543?manu=&fgcd=). Women in the control arm received food rations comprising of wheat flour and oil.
The biscuits and rations were distributed to the females on a fortnightly basis at their homes and compliance was checked and recorded in a specially designed questionnaire by home visits on alternate days. Each 90 gram packet of biscuits contained five biscuits with total 450 calories. Women were asked to consume one packet daily. To avoid sharing of biscuits we provided additional regular biscuits of the sort available in local markets to the children of participants.
3.2 Outcomes
The primary outcome of our study was neonatal birth weight before 48 hours of life. Secondary outcomes were maternal hemoglobin and Ferritin levels measured at enrollment and at the third visit in last trimester (33-35) weeks.
3.3 Sample size and Randomization
The sample size was estimated using birth weight as the primary outcome variable. Based on estimation that mean birth weight in the intervention arm would be 2500 g +300 g we required 224 deliveries in each armand, allowing for attrition of 20 % we estimated that we needed 280 women in each limb.
Our funding allowed 150 women in each limb was we adopted a proof of concept approach in order to inform future studies in the region.
The randomization sequence was generated prior to enrolment. Randomization was undertaken in blocks of 4 using participant identification numbers to maintain equal number of participants in each arm. The allocation sequence was generated by the clinical trials unit of the Aga Khan University. After screening and explaining the objectives of study in local language, a written consent was sought by all participants. We took thumb impressions of participants who were illiterate. After enrolment, the medical officer allocated sequential identification numbers. In accordance with the trial design, the intervention arm received high energy biscuits and the control arm received supplementation with wheat flour (5 kg) and oil (1 liter) every fortnight.
4. Follow-up and Outcome Assessments
Follow up was undertaken as shown in Figure 1. Data was collected using pre-designed and pretested questionnaire by research associates with a separate chart for each visit. We used Tanita HD# 314 digital scale for measurements of weight and Shor boards for measuring height of mothers and length of newborns. Neonatal fronto-occipital circumference (FOC) and mid-upper arm circumference (MUAC) were measured by using measuring tape to the nearest mm. All anthropometric measurements were taken three times at each visit and then an average of the three measurements was taken. In case of discrepancy in measurements the physician at primary health unit rechecked for ascertainment of valid numbers. Samples were also drawn for Ferritin & hemoglobin on third visit between 33- 35 weeks of gestation. This date was calculated on the basis of last menstrual period (LMP). Participants were visited by Community health workers on alternate days to record compliance by a dietary recall and the collection of empty wrappers.Follow up of the newborn was undertaken within 48 hours of delivery. Length, weight, FOC and MUAC were recorded. Ascertaining and attributing causes of death were performed using verbal autopsy in accordance with the verbal autopsy standards [15].
4.1 Analysis
The data was analyzed using Statistical Package for Social Sciences (SPSS version 16.0). Continuous variables of normal distribution were presented as mean and standard deviation (mean ± SD) and numbers with percentages n (%). The level of significance between groups was assessed by Student’s t-test. The paired t-test was also performed for mean differences in biochemical measurements from enrolment to last follow up for each group. Chi- square test was used to compare categorical variables for significant difference in group percentages. A p-value of less than 0.05 was considered to be significant.
Categorical variables were assessed by unconditional logistic regression and odd ratios (ORs) derived. The factors with significant association in univariate analysis were further analyzed by a multivariable logistic regression.
4.2 Ethics
Women were enrolled in the study after taking written informed consent. Enrolled women could withdraw from the study at any point without affecting their access to and use of routine health services. Confidentiality of information was strictly followed. The ethical review committee of the Aga Khan University approved the study. The study is registered as an International Standard Randomized Controlled Trial, number NCT 02294240.
4.3 Results
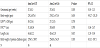
We randomly enrolled 300 women from September 2014 till March 2016. Primary Outcome data was available for 233 women, 117 in Intervention arm and 116 in Control arm (Table 1). 67 women dropped out due to multiple reasons. Their baseline characteristics were analyzed with women who completed study and no significant difference was found except that there were more primigravida (44.8%) in the drop out group. Overall baseline maternal and household characteristics were similar in both groups. The participants were mostly young malnourished females with mean age of 23 years ±4.6, mean BMI of 18.33±1.4 and predominantly multiparous (43.3%) (Table 2). The overall compliance for biscuits was 75.3%.
The birth weight and anthropometric parameters of neonates were not significantly different The mean birth weight in intervention arm was 2768 + 473 g and in control arm was 2742 + 473 g and the difference of 26 g (95 % CI -95.27 - 151.33) is non-significant ( p=0.65). The Fronto-occipital circumference (FOC) in intervention arm is 31.1±8.04 cm and in control arm is 30.8±8.9 cm, the difference is 0.3 cm, p value=0.780 CI (-1.86 - 2.47). The length in intervention arm is 44.4±12.2 cm and in control arm is 43.6±12.8 cm, the difference is 0.8 cm, p value=0.615 CI (-2.33 - 3.94). (Table 3).
Ferritin was not normally distributed so Whitney U test was applied and there was statistically significant difference noted in endline ferritin between intervention and control arms 34.76±62.39 vs 20.92±31.90 p value 0.05 and also in Hemoglobin levels -0.54±2.43 Vs 0.92±2.32 P value<0.0001 between the two arms (Table 4). The rate of fetal loss in the forms of abortions and still birth were higher in control arm (15 abortion and 4 still birth compared to 12 abortions and 2 still birth in intervention arm ) while deaths are higher in the intervention arm 4.4 % versus 2.2% .
We established by interviewing the women that the shape and appearance of biscuits were liked by more than 60% of participants. The taste of biscuits was also assessed and more than half of the participants found it good with 57 % felt aroma is satisfactory.
5. Discussion
We found no significant increase in neonatal birth weight for term infants with supplementation of energy dense biscuits. The lack of an observed effect of the high energy biscuits could be for a number of reasons: These women were chronically malnourished and, as a result, stunted. This is likely to result in a reduced pelvic capacity, adverse epigenetic programming [16] and, in common with other similar studies we were unable to show an effect over the course of a single pregnancy. The effect might also have been blunted by the compliance though reported compliance was 75% and we do not have a reason to that this was over reporting. The intake of the energy dense biscuits could have also led to reduction in appetite in general but we do not have quantifiable dietary data so difficult to comment. The comparison arm also received a food ration and this could have improved dietary intake in women in this Arm as well but this is hard to quantify as the ration (wheat and oil) was not restricted to the pregnant women but used in general for meals by all family members.
There was however, a higher maternal Ferritin level, one of the secondary outcomes, in the intervention group suggesting there was a replenishment of iron stores with high energy biscuits. It is widely accepted that serum ferritin remains the best indicator of iron stores in the absence of inflammation [17] and poor compliance to iron supplements during pregnancy are associated anaemia in puerperium even [18]. Though we cannot exclude inflammation as a contributor to the difference, there was no clinical reason to suspect this. It seems more likely that iron absorption and storage was enhanced.
We also found higher but not statistically significant number of deaths in the intervention arm. This paradoxical finding was also made by Personn et al in a multiple micronutrient (MMN) study in which the authors attributed asphyxia as the cause of this higher mortality [19]. In our trial this could be a chance finding. The frequency of skilled birth attendants was similar across groups but surprisingly in both groups combined, most deaths occurred in facility based deliveries in our trial another finding which warrants further scrutiny.
To our knowledge this is the first study in our region where macro and micronutrients are used in the form of biscuits. However, Ceesay et al tested high energy groundnut biscuits in Gambian pregnant women and found substantial reduction in the prevalence of stillbirths and in early neonatal mortality [20]. Evidence suggests poor compliance of MMN in form of tablets. The other advantage is the provision of high energy food in the form of these biscuits can be a practical option when mass delivery is needed as in pregnant females during disaster settings thereby saving women and children during critical situations.
The strengths of our study are the population which is more close to population of Pakistan, good follow ups, robust measurement of birth parameters within 24 hours of delivery. Our limitations were a small sample size that could have failed to detect any small changes in anthropometric measurements and subjectivity in the measurement of compliance.
Competing Interests
The author declare that there is no competing interests regarding the publication of this article.
Author Contributions
FNQ, AZ, SZ, FQ and AK made substantial contributions (1) to design,
acquisition and analysis and interpretation of data; 2) was involved
in drafting the manuscript and revising it critically for intellectual
content and 3) has given final approval of the version to be published
FNQ, SZ, SS and NB have made substantial contributions (1) to
acquisition of data, 2) has been involved in drafting the manuscript
and 3) has given final approval of the version to be published
FNQ, NB, SS were involved in data analysis and compilation of results
FNQ, AZ, SS, SZ, NB were involved in drafting the manuscript or
revising it critically for important intellectual content; and 3) has
given final approval of the version to be published
Disclosure of Support
Drs Farah Naz Qamar and Shazia Sultana received research training support from the National Institute of Health’s Fogarty International Center (1 D43 TW007585-01). The sponsors did not have a role in study design, data analysis or report writing.