1. Introduction
Osteoarthritis of the knee (OA) is well known to be a disease characterized by pain, stiffness, swelling and deformation of the joints, which develop slowly and worsen over time [1,2]. Progressive cartilage degeneration of the knee is also reported to lead to deformity and outward curvature of the knee responsible for both the development of a limp and total knee replacement surgical procedures [3]. It is also accepted that OA is often associated with excess body weight called obesity, and a history of repeated injury of the knee. Although OA is not life-threatening disease, it can deteriorate the quality of life and an economic burden through the clinical symptoms such as pain in affected joints during or after movement [4]. Histological observation of OA clearly showed the degradation and destruction of proteoglycan and collagen, which are mainly caused by matrix metalloproteinases [2,5]. It is also showed that OA is not classified to be inflammatory diseases, but there is much evidence that synovial fluid obtained from OA contained much higher levels of several types of inflammatory cytokines, including IL-1β, IL-6 and TNF-α as compared with healthy control and the concentrations of cytokines in synovial fluids are correlated with OA severity [6,7]. Furthermore, it is also reported that nitric oxide (NO), a member of reactive oxygen species, plays a pivotal role in the development of OA through its activities on apoptotic cell death and tissue destruction in the joint, which are associated with cartilage matrix degradation [8,9].
Currently available treatment of OA includes the use of nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen and intra articular injection of either hyaluronic acid or corticosteroids [10,11]. Physical and occupational exercises are also used to prevent the development of OA [10]. These treatments are well known to relieve pain, inflammation and improve functionally, but do not resolve the pathological process once triggered [10,12]. On the other hand, there are much evidence that oral administration of dietary supplements, especially glucosamine hydrochloride (GH) and chondroitin sulfate into patients with OA could favorably modify the clinical conditions of the disease such as pain, stiffness and joint swelling [11-14]. It is also reported the suppressive effects of GH and chondroitin sulfate on joint space narrowing and osteoarthritis progression [15]. Although these therapeutic effects of agents are speculated to be owing, in part, to inhibition of metalloproteinase activity, prostaglandin biosynthesis and degradation of glycosaminoglycan, as well as stimulation of hyaluronic acid synthesis in the joint [15], the mechanisms by which dietary supplements could modify the clinical conditions of OA are not well defined.
Periostin was originally identified in a mouse osteoblastic cell line as a matricellular protein, which is classified into the fascilin family [16,17]. This protein was secreted from various types of cells such as fibroblasts and other structural cells after the stimulation with inflammatory cytokines [16]. Periostin is reported to be an important regulator of fibrosis and collagen deposition [18]. Although periostin is recognized to be involved in repairing and remodeling of injured tissues such as bone fracture and heart tissues after myocardiac infarction [18], it is reported that periostin plays essential roles in the development of OA through amplifying inflammatory events and accelerate OA pathology [1,2]. The present study, therefore, was undertaken to examine the influence of GH on periostin-induced biochemical mechanisms responsible for the development of OA through examining the influence of GH on the production of NO, which is an important final effector molecule in the development of OA, from synoviocytes in vitro.
2. Materials and Methods
2.1 Reagents
GH, purchased from SIGMA-Aldrich Co. Ltd. (St Louis, MO, USA) was dissolved in Synoviocyte Growth (SG) Medium (Cell Applications, Inc., San Diego, CA, USA) at a concentration of 10.0 mg/ml, sterilized by passing through 0.2 μm filters and stored at 4°C until used. Recombinant human periostin was purchased from R & D Systems, Inc. (Minneapolis, MN, USA) as preservative free pure powders. Periostin was also dissolved in SG Medium, sterilized and stored at 4°C until used.
2.2 Cell culture
Human synoviocytes (HFLS-OA) obtained from the inflamed synovial tissues of an OA patient (Cell Applications, Inc., San Diego, CA, USA) was suspended in SG Medium at a concentration of 1 x 105 cells/ml and used as a target cell. To examine the influence of periostin on NO production from HFLS-OA, 1 x 105 cells (1.0 ml) were introduced into 24-well culture plates in triplicate and stimulated with various concentrations of periostin in a final volume of 2.0 ml. After 24 h, culture supernatants were collected and stored at -40°C until used. To prepare cells for examining the influence of GH on transcription factor (NF-κB) activation and iNOS mRNA expression in HFLS-OA after periostin stimulation, 1 x 105 cells (1.0 ml) were introduced into each well of 24-well culture plates in triplicate. The cells were then stimulated with 100.0 ng/ml periostin in the presence of various concentration of GH in a total volume of 2.0 ml for 4 and 12 h, respectively. In all experiments, GH was added to cell cultures 2 h before stimulation.
2.3 Assay for NO
NO levels in culture supernatants were examined in duplicate with commercially available Griess reagent kits, which is measurable NO2 and NO3 (Dojin Co., Ltd., Kumamoto, Japan) according to the manufacturer’s recommended procedures.
2.4 Assay for transcription factor activation
NF-κB activity in cultured cells was measured using NF-κB P65 ELISA test kit (Active Motif Co. Ltd., Carlsbad, Calif., USA) according to the recommended procedures.
2.5 Assay for mRNA expression
Poly A+ mRNA was separated from cultured cells with oligo (dT)- coated magnetic micro beads (Milteny Biotec, Bergisch Gladbach, Germany). The first-strand cDNA was synthesized from 1.0 μg of Poly A+ mRNA using a Superscript cDNA synthesis kit (Invitrogen Corp., Carlsbad, CA, USA) according to the manufacturer’s instructions. Polymerase chain reaction (PCR) was then carried out using a GeneAmp 5700 Sequence Detection System (Applied Biosystems, Forster City, CA, USA). The PCR mixture consisted of 2.0 μl of sample cDNA solution (100 ng/μl), 25.0 μl of SYBR-Green Mastermix (Applied Biosystems), 0.3 μl of both sense and antisense primers, and distilled water to give a final volume of 50.0 μl. The reaction was conducted as follows: 4 min at 94°C, followed by 40 cycles of 4 min at 95°C, 1 min at 60°C and 1 min at 70°C [19]. GAPDH was amplified as an internal control. mRNA levels for iNOS were calculated by using the comparative parameter threshold cycle and normalized to GAPDH. The nucleotide sequences of the primers were as follows: for iNOS, 5’-TGCAGACACGTGCGTTACTC-3’ (sense) and 5’-GGTAGCCAGCATAGCGGATG-3’ (antisense), and for GAPDH, 5’-TGCACCACCAACTGCTTAGC -3’ (sense) and 5’-GGCATGGACTGTGGTCATGAG-3’ (antisense) [19].
2.6 Statistical analysis
Statistical significance between control and experimental groups was examined by ANOVA followed by Dunette’s multiple comparison test. Data analysis was performed by using ANOVA for Mac (SPSS Inc., Chicago, IL, USA). The level of significance was considered at a P value of less than 0.05.
3. Result
3.1 Influence of GH on NO production from HFLS-OA after periostin stimulation
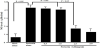
The first experiments were undertaken to examine whether periostin stimulation could induce NO production from HFLS-OA. HFLSOA (1 x 105 cells/ml) was stimulated with various concentrations of periostin in triplicate and culture supernatants were collected 24 h after culture for measurement of NO levels. As shown in Figure 1, periostin stimulation caused increase in NO production from HFLS-OA, which was firstly observed at 50.0 ng/ml and peaked at more than 100.0 ng/ ml. The next experiments were designed to examine the influence of GH on NO production from HFLS-OA in response to periostin stimulation. HFLS-OA (1 x 105 cells/ml) was stimulated with 100.0 ng/ml periostin in the presence of GH at concentrations of 0.5 mg/ ml to 2.0 mg/ml and NO levels were measured 24 h after stimulation. As shown in Figure 2, treatment of cells with GH caused inhibition of NO production, which was increased periostin stimulation. The minimum concentration of GH that caused significant suppression was 1.5 mg/ml.
3.2 Influence of periostin on NF-kB activation in HSLF-OA after periostin stimulation
The third experiments were designed to examine the influence of GH on transcription factor activation in HFLS-OA in response to periostin stimulation. HFLS-OA (1x105 cells/ml) was stimulated with 100.0 ng/ml periostin in the presence of GH at concentrations of 0.5 mg/ml to 2.0 mg/ml and NF-κB P65 activity was measured 4 h after stimulation. As shown in Figure 3, addition of GH at more than 1.5 mg/ml into cell cultures significantly suppressed NF-κB P65 activation, which was increased by periostin stimulation.
3.3 Influence of GH on the iNOS mRNA expression in HFLS-OA after periostin stimulation
The final experiments were carried out to examine the influence of GH on iNOS mRNA expression in HFLS-OA after periostin stimulation. HFLS-OA (1x105 cells/ml) was stimulated with 100.0 ng/ml periostin in the presence of GH at concentrations of 0.5 mg/ml to 2.0 mg/ml for 12 h and iNOS mRNA expression was examined by real time RT-PCR. As shown Figure 4, treatment of cells with GH at more than 1.5 mg/ml caused significant suppression of iNOS mRNA expression in HFLS-OA, which was increased by periostin stimulation.
4. Discussion
OA is well known to be a slowly progressive degenerative disease, involving cartilage and structural cells in the joints, which caused significant pain and disability [1,2]. Although several types of agents, including NSAIDs, corticosteroids and hyaluronic acid, are used for the treatment of OA, these agents could not resolve the pathological process once triggered [10-12]. On the other hand, dietary supplements such as GH and chondroitin sulfate are used frequently in the treatment and prevention of OA and reported that these two agents reduce space narrowing in affected joints and radiographic progression of OA [11-15]. However, the therapeutic mechanism(s) of these two agents are not well defined. The present study, therefore, was undertaken to examine the influence of GH on the ability of synoviocytes to produce NO, which is one of the important final effector molecules in the development of OA [8,9] by an in vitro cell culture technique.
The present results clearly showed that treatment of synoviocytes from an OA patient with GH significantly inhibited NO production after periostin stimulation. The minimum concentration of GH that caused significant suppression was 1.5 mg/ml. It is reported that after oral administration of GH at 1500 mg/day that is recommended therapeutic dose of OA [20,21] for three days into healthy human, plasma levels of GH reaches approximately 2.0 mg/ml [22] to 4.4 mg/ ml [23], which are higher levels than that inducing suppressive effect of GH on NO production in vitro. Pharmacokinetics of GH was further investigated in OA patients after oral administration at 1500 mg oncedaily for 14 days [24]. This report showed that GH was bioavailable in the joint and the level of GH was higher in the synovial fluid compared to plasma (up to 25% higher). Judging from these reports, the findings of the present in vitro study may reflect the biological function of GH in vivo. NO is synthetized in mammalian cells by the conversion of L-arginine to L-citrulline, which is mediated by one of three isoforms of nitric oxide synthase (NOS). NOS enzymes, namely endothelial NOS (eNOS) and neuronal NOS (nNOS), constitutively produce relative low levels of NO, which is function in maintaining homeostasis [8,9]. On the other hand, inducible NOS (iNOS) is expressed for longer period in cells upon activation by inflammatory cytokines and produces much higher levels of NO, which responsible for the oxidation of proteins, lipids and ribonucleases, among others [8,9]. It is also accepted that NO synthesized by iNOS diffuses out of the cells and reacts with superoxide to generate peroxynitrite responsible for a number of destructive events in cartilage such as chondrocyte apoptosis, proteoglycan degradation and breakdown of the extracellular matrix through the enhancement of activation of matrix metalloproteinases [8,9]. Pain is the most important symptom of OA and the major determinants in functional disability [1,2]. It is reported that injection of superoxide dismutase into mice prevents not only peroxynitrite formation but also hyperalgesia associated with carrageenan injection [25], indicating that superoxide, NO and peroxynitrite play essential roles in the development of pain and nociception. Taken together, the present results may suggest that oral administration of GH into OA patients prevents NO production from synoviocytes and results in inhibition of joint space narrowing through the inhibition of cartilage destruction and relieve pain in affected joints.
Periostin has been shown to activate NF-κB, which helps to mediate transcription of several types of genes such as IL-1β and iNOS, in keratinocytes and fibroblasts, resulting in increase in the ability of cells to produce both inflammatory mediators and enzymes [26,27]. These reports may suggest that GH inhibits NF-κB activation after periostin stimulation and iNOS mRNA expression, resulting in iNOS production in synoviocytes. This speculation may be supported by the observation that addition of GH into cell cultures caused the inhibition of both NF-κB activation and iNOS mRNA expression, which were observed in cells after periostin stimulation. NF-κB activation requires the increase in Ca2+ levels in cytosol [28]. It is also reported that GH could inhibit the increase in intracellular Ca2+ levels in both rat microglial cells after lipopolysaccharide stimulation and cardiomyocytes induced by angiotensin II stimulation in vitro [29]. Furthermore, GH is reported to inhibit the activation of several types of protein kinases, which are responsible for transcription factor activation [30,31]. From these reports, there is possibility that GH inhibits the activation of protein kinases through the inhibition of increase in Ca2+ levels in synoviocytes after periostin stimulations resulting in suppression of iNOS production and NO generation.
5. Conclusion
The present results clearly demonstrated that GH exerts the inhibitory effects on periostin-induced NO generation in human synoviocytes. These results strongly suggest that the ability of GH to suppress NO production from synoviocytes may account, at least in part, for the clinical efficacy of GH on OA.
Competing Interests
The authors declare that they have no competing interests.
Author Contributions
Contribute to cell culture and sample collection.
Assay for NO levels, NF-κB activation.
Data analysis, including statistical analysis (for data presented in: Figures 1-4).
Preparation of Figures 1-4.
Assay for iNOS mRNA expression.
Kazuhito Asano:
Contribution to study design.
Participation in the methodological design and protocol.
Contribution to the entire manuscript writing.