1. Introduction
Autism spectrum disorders (ASD) are developmental disorders associated with a high individual and social burden, but their aetiology is poorly understood. The prevalence of ASD among 3-17 year-old children has suddenly increased, reaching 2.24% in a 2014 national survey in the United States [1]. The prevalence of ASD is likely to increase in Japan [2].
Vitamin D is a secosteroid associated with peripheral calcium homeostasis and nervous system function [3]. Vitamin D exists in two major forms, vitamin D2 from plants and D3 from animals. Both vitamin D2 and D3 are biologically inert and require activation through two hydroxylation processes involving 25-hydrooxylase (CYP2R1) and 1α-hydroxylase (CYP27B1), located in the liver and kidney, respectively [4]. 1, 25-dihydroxyvitamin D (1, 25OHD) is a biologically active metabolite produced by two hydroxylation reaction steps in the nervous system [5]. Vitamin D modulates the central nervous system thorough its receptors which are expressed in neuronal and glia cells in almost all regions of the central nervous system [6].
It has been suggested that vitamin D reduces the risk of ASD. Cohort studies, have shown low neonatal vitamin D to be a possible risk factor for ASD [7,8]. Studies have also investigated the association between vitamin D concentrations during pregnancy and total behavioral and neurodevelopmental problem [9-11]. However, prospective studies have not found an association between 25-hydroxyvitamin D (25OHD) concentration and ASD.
ASD usually appears during the first three years of life [12]. In one case report, Vitamin D supplementation led to significant reduction in core symptoms of ASD [13]. The present study was designed to investigate the effect of vitamin D3 supplementation corresponding to twice the daily requirement for 9 months on core symptoms of 3-yearold Japanese children with ASD.
2. Materials and Methods
2.1 Subjects and setting
Prior to the study, approval was obtained from the ethics committee of Bukkyo University (project registration number in 2018: 7). We enrolled 5 males and 1 female Japanese ASD children aged 3 years. The researchers were present at the child welfare institution (Mukunokien, Kyoto, Japan) where the study was conducted to assure the proper management of safety and confidentiality in the study. The manager of the institution invited parents to participate in the study, and all the children whose participation was requested from January to September in 2019 were enrolled. All subjects took oral vitamin D supplements (Baby D®200: 5.0μg/day of vitamin D3 oil purchased from Morishita Jintan Co., Ltd., Osaka) for 9 months.
2.2 Adaptive function test
All children were assessed for autism behavior using the Childhood Autism Rating Scale (CARS) [14]. An adaptive behavior scale (Vineland-II) [15] was used to identify communication, daily life, social and motor skills through a semi-structured interview conducted with parent and caregiver. The Short Sensory Profile (SSP) was used to quickly identify children with sensory processing problems from parent reports of sensory behaviors in their child [16].
The tests were performed by skilled occupational therapists.
2.3 SerumCa, iPTH and 25OHD
Blood was collected by venipuncture and serumCa, iPTH and 25OHD concentrations were measured by Kyoto Microbio Laboratory, (Kyoto, Japan).
2.4 Statistical analysis
The differences between before and after intervention with vitamin D3 supplements were evaluated using the Wilcoxon test. A p-value of < 0.05 was considered to be statistically significant. Analyses were carried out using SPSS 21 for Windows (IBM, Japan).
3. Results and Discussion
3.1 Study subjects
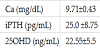
Characteristics of the study subjects are shown in Table 1. Age was 3 years for all the children (males, n=5 females, n=1). Ca and iPTH were within the normal range, but 25OHD was below the sufficient value (>=30ng/mL) (Table 1).
3.2 Change in serum 25OHD
Serum 25OHD was classified as normal (>=30 ng/ml), insufficient (>20 to 29.9), or deficient (<=20). In this study, the level was deficient (n=2) or insufficient (n=4). Nine-month intake of vitamin D3 supplements increased serum Ca and 25OHD concentration significantly (Figure 1). Serum Ca and iPTH were within normal range for 9 months. The vitamin D deficient group decreased from 2 children to 1 (1: became insufficient) and the insufficient group decreased from 4 children to 3 (1: became sufficient). These results suggest that vitamin D3 supplement intake increased serum 25OHD levels.
3.3 Adaptive function
The CARS and SSP scores decreased in all except one child who had originally high 25-hydroxy vitamin D levels (28 ng/mL) (Figure 2).
Among the ASD children in this study, vitamin D administration had a positive effect on “communication skills”, “ADL skills”, “social skills” or “motor skills” in two children, based on the Vineland-II (Figure 3).
Many epidemiological studies have assessed the relationship between vitamin D and ASD [17]. The majority have examined the relationship between the vitamin D status of pregnant women and the risk of ASD in their children, and reported the vitamin D status of ASD children. Some studies have found no relationship between vitamin D status and ASD [18,19].
A few studies have reported the effect of vitamin D supplementation in women during pregnancy and in children with ASD. Vitamin D supplementation at adequate dose during pregnancy reduces the incidence of autism [20]. Administration of vitamin D administration to a vitamin D deficient 32-month-old boy with ASD improved his core symptoms of autism [13]. Among the children in this study, vitamin D supplementation had an ameliorative effect on “communication skills”, “ADL skills”, “social skills” or “motor skills” associated with the disorder.
Vitamin D is regarded as a hormone that is active not only in regulating blood calcium but also in brain development. Vitamin D may have a positive effect on serotonin, which affects brain development [21]. The developmental disruption of serotonin signaling may be involved in autism [22]. These results suggest that vitamin D supplementation may ameliorate clinical symptoms in ASD children.
This is a preliminary study with a very small number subjects, and it was uncontrolled. Further study with larger numbers of subjects is warranted, and could reveal optimal 25OHD levels for ameliorating ASD symptoms and preventing falls in ASD children.
4. Conclusion
These findings indicate that vitamin D supplementation might improve adaptive function.
Competing Interests
The authors declare that they have no competing interests.
Author Contributions
Dr. Hasegawa was responsible for the study conception, design, and
analysis, interpretation of data, and drafting of the manuscript.
Ms. Mochizuki was responsible for data acquisition and proof
reading of the manuscript, and she participated in the data analysis.
Dr. Yamada was responsible for the data acquisition and proof
reading of the manuscript.
Acknowledgments
The author acknowledges Ms. Chizu Shibuya and Ms. Fumie Fukuda for then kind help.