1. Introduction
The World Health Organization (WHO) reported that there are 1 billion adults diagnosed with hypertension globally and that estimate is projected to increase by approximately 1.7 billion (60%) by 2025 [2]. Increase in global hypertension has been attributed to a steady increase in hypertension in developing countries [2]. A systematic review of literature [3] on hypertension prevalence in Sub-Saharan Africa found hypertension to be more prevalent in urban than rural areas. This was attributed to a population shift from rural to urban areas, increased consumption of processed foods, obesity and physical inactivity. Hypertension is defined as an average systolic blood pressure of greater or equal to 140 mm/Hg or a diastolic blood pressure of greater than or equal to 90 mm Hg [4,5].
Uncontrolled blood pressure is one of the primary risk factors for cardiovascular diseases, stroke, premature morbidity and mortality worldwide [2,6,7]; and has been identified as the third leading cause of disability worldwide [5,8].
In the Sub-Saharan Africa, much attention over the past few decades have been primarily on the prevention of communicable diseases [2] such as the Human immunodeficiency virus/acquired immunodeficiency syndrome (HIV-AIDS). However, noncommunicable diseases, such as hypertension is emerging in the Sub-Saharan Africa region as major population health crises [3,8]. Cameroon, a country in the Sub-Saharan African region is also experiencing a public health emergency with increasing number of hypertensive patients. A 2007 study [9] examined hypertension burden and related risk factors (smoking, obesity, alcohol consumption and sedentary lifestyle) among adults in Cameroon. The researchers reported that in 1994, the prevalence rate of hypertension and diabetes was approximately 8% and 1% respectively. In 1998, hypertension prevalence increased to 18% and diabetes to 6%.The increase in the number of hypertensive patients is thought to be related to a population shift from rural to urban areas, increased consumption of processed foods, obesity, and physical inactivity [9].
Treatment with anti-hypertensive medications has been shown to reduce disease related complications such as cardiovascular disease, stroke, kidney disease and sudden death, yet non-adherence remains a significant global health problem [5,6,18]. Despite numerous studies that have identified factors associated with medication non-adherence in developed countries [10-12], no studies have been published in Cameroon to address this problem. Therefore, further exploration for this study was necessary. The purpose of this study was to investigate factors associated with medication adherence among hypertensive adults in the North West Region of Cameroon.
2. Theoretical Framework - Social Cognitive Theory of Self Efficacy
This study utilized Bandura’s theory of self-efficacy. Self-efficacy theory is developed from social cognitive theory that suggests that behavior, cognition and environment have interacting influences among each other [13]. Self-efficacy, "refers to beliefs in one's capabilities to organize and execute the courses of action required to manage prospective situations" [14]. The principle behind selfefficacy is that, the ability to modify a behavior is influenced by expected outcome gained from that modification and the ability to self-motivate to maintain the desire outcome [13]. It is the confidence one feels about performing a task, the confidence in overcoming the barriers to achieve the given task and the outcome expected.
Self-efficacy has been recognized as a predictor of health behavior [15]. Individuals with chronic diseases who perceive high levels of self-efficacy are more likely to adhere to treatment recommendations than individuals with low efficacy [16]. Therefore, the belief that blood pressure can be controlled by adhering to medication regimen may become a stimulus to trigger a hypertensive patient to adhere to treatment recommendations. It was reported that patients with high self-efficacy would have higher adherence to treatment recommendations than those with low self-efficacy [15,16]. Factors examined in this study, e.g. demographic characteristics have been associated with the outcome of medication adherence [21].
2.1 Operational definition of terms
2.1.1 Hypertensive patient
This is a patient with blood pressure readings greater than or equals to 140/90mm/Hg [4,5] and is currently taking one or more antihypertensive medications.
2.1.2 Medication Adherence
Adherence was defined as the extent to which a person's behavior i.e., taking medication, following a diet, and/or executing lifestyle changes corresponds with agreed recommendations from a health care provider [18]. Adherence is the endurance from the practice and maintenance of desired health behaviors and is the result of active participation and shared decision making between patients and health care providers [19,20].
2.1.3 Factors associated with hypertensive medication
It was defined as variables found in the literature associated with treatment adherence. This would be measured by the self-reported responses to the 15-items on demographic questionnaire. Twelve items were adopted from a study [21] and three additional items are specific to the study population. Variables included age, gender, marital status, education level, occupation, monthly household income, smoking, alcohol consumption, perceived health status, number of hypertensive medication used, duration on antihypertensive drugs, and distance from home to clinic, methods of transportation, and traditional medicines use.
3. Research Design
A descriptive cross-sectional research design utilized two selfadministered questionnaires collected between July 31 and August 31 2014. This design was chosen because it is quick, economical, and provided the researcher with information relating to the relationships and associations between variables of interest, as they exist in the natural state.
4. Population and Setting
This study was conducted at two hospitals in the North West Region of Cameroon. The first hospital: Bamenda Regional Hospital is own and operated by the government. The second hospital, St. Monica Hospital - Ndop is a small rural hospital about 30 Km from Bamenda and is own and operated by the Catholic Mission. The North West region was chosen because it is the second largest and most densely populated region among Cameroon’s ten regions [22].
A convenience sample of adult males and females, who were established patients at the outpatient hypertension clinics at both hospitals were eligible to participate in the study.
Inclusion criteria for sample selection:
- Eighteen (18) years and above
- Diagnosed with hypertension for at least 6 months
- Speaks and understand English or Pidgin English
- Currently taking at least one antihypertensive medication for the past 6 months
Exclusion Criteria:
- Pregnant women
- Patients with mental illness
- Patients needing emergency care
- Patients who were critically ill.
5. Ethical Considerations
Approval to conduct this study was obtained from William Paterson University Institutional Review Board Committee, Bamenda Regional Hospital and St. Monica Hospital. All participants were informed of the study purpose and a verbal consent was obtained. Confidentiality and anonymity of each participant was maintained.
5.1 Instruments and data collection methods
Data was collected using two self-administered surveys. A standardized demographic questionnaire was adapted from the study by Lee et al. [21] and modified to the population of interest. This questionnaire included demographic variables: age, gender, marital status, education, occupation, income, smoking, alcohol, number of antihypertensive medication used and duration on antihypertensive medication. Distance from home to clinic, traditional medicines use, method of transportation, and perceive health status was added to provide a better caption of the population of interest.
A second questionnaire was the Modified Medication Adherence Scale (MMAS-8) [1]. The MMAS-8 has been used in numerous studies measuring hypertension medication adherence [23,21]. This instrument has a Cronbach alpha = 0.83.
The researcher who was familiar with the region approached established patients who presented at the clinics for scheduled appointments. The purpose of the study was explained and the questionnaires were read in English and Pidgin English. Pidgin English is a local language spoken by many in this region. Reading the questionnaires in English and Pidgin was necessary to increase sample size and thus generalizability of the study. Participants who provided verbal consent were given the demographic and the MMAS- 8 questionnaires to complete. The researcher was present to answer questions.
5.2 Data analysis
Data was analyzed using the Statistical Package for the Social Sciences for Windows 11.0 [24]. Descriptive statistics was computed for patient’s characteristics. Chi-square testing was calculated to determine relationships between socio-demographic variables and medication adherence. A Pearson correlation was used to examine statistically significant relationships between the research variables and medication adherence and to determine if there were any statistically significant correlation between blood pressure readings and medication adherence.
6. Results
6.1 Demographic variables
6.1.1 Questionnaires distribution
Two hundred and ten questionnaires were distributed and collected by the researcher at two hospital-based clinics in the North West Region of Cameroon. Two hundred and six (206) were completed and returned (response rate of 98%). Six questionnaires had missing data and were removed. The total sample (N = 200) included patients from regional hospital clinic (n = 164), and a rural hospital clinic (n = 36). No significant differences were identified between these groups so the samples were aggregated.
6.1.2 Sample
A convenience sample of adult hypertensive patients from two local hospitals (N = 200) who were 18 years or older and who met research criteria participated in this study.
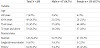
In Table 1, the majority of the respondents (45.5%, n = 91) were between the ages of fifty-five and sixty nine years, with nearly twice as many females to males (65.5%, 34.5%) respectively. There was no statistically significant difference in the mean age for males or females. Sixty four percent (n = 128) of participants indicated “married” as their marital status with no significant difference in gender. However, approximately forty seven percent of widow were females (n = 63).
6.1.3 Education, occupation and income
In Table 2, the majority of participants had primary or below primary educational preparation (66.5%). Eight percent (8%) reported earning a university degree. The majority reported their occupation as a housewife (35%), followed by being employed (30.5%). When analyzed by gender, the (52%) of females were housewives (n = 69) and the majority (40%) of males were employed (n = 27), with an equal percent (26%) of females employed outside of the home (n = 34). Twenty three percent of the participants were retired (n = 46). Computation for monthly income indicated that the majority of the participants (65%) had a monthly income less than 50,000 Francs ($100.00). A quarter of the participants earned over 100,000 Francs ($200.00). A statistically significant difference was found in earnings between genders (r (198) = -.367, (p<.05), with women likely making less money than men do.
6.1.4 Smoking and alcohol use
In Table 3, the majority of participants (96.5%) did not smoke cigarette and did not drink alcohol (63.5%). However, when analyzed by gender, there was a statistically significant association with males who smoked cigarettes (r (198) = .265, p< .05), men were more likely to smoke cigarettes than women. No statistically significant association was found with gender and alcohol use.
6.1.5 Variables related to hypertension
Systolic & diastolic Blood Pressure, number of anti-hypertensive medications taken, duration on anti-hypertensive medication and traditional medicine.
In Table 4, approximately 47% (n = 94) of the participants had a normal blood pressure readings. The mean systolic blood pressure was 141mm/Hg (SD = 20.1723) and the mean diastolic blood pressure was 85mm/Hg (SD = 12.175). Approximately 55% (n = 109) reported taking one anti-hypertensive medication. The majority of participants (53.5%) reported taking antihypertensive medications for over five years. When asked about traditional medicines used for hypertension, 86.5% (n = 173) reported that they do not take any traditional medications.
6.1.6 Medication adherence behaviors
Medication adherence, distance to hospital, method of transportation and health perception.
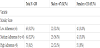
In Table 5, adherence score ranged from “0” to “8”, Low (< 6), medium (6 - < 8) and high (=8) adherence (Morisky et al., 2007). The total mean score was 6.33, SD = 2.089. Approximately 31%, (n = 63) achieved a low medication adherence, 32%, (n = 64) medium adherence and 36% (n = 73) were found to be at high adherence. Approximately 68% (n = 137) of participants achieved a score greater than six and were considered adherent to antihypertensive medications.
In addition, in Table 5, 75% (n = 150) of the participants lived under 10 Km, with half of the respondents (n = 100) reported using taxis for their method of transport. When asked about perceived health status, the majority (46.5% n = 93) perceived their health status to be “fair” with no significant difference in gender.
6.1.7 Statistical analysis
The chi-square test of independence was conducted to determine whether each independent variable, measured as either continuous or categorical, were contingent on medication adherence. Two statistically significant chi square test results were found: alcohol use and level of education.
A chi-square test of independence was calculated to test whether or not the alcohol use was independent of medication adherence. A statistically significant interaction was found (X2 = 10.226, df = 2, p<.05).
A chi-square test of independence was calculated to test whether or not level of education was independent of medication adherence. A statistically significant chi square result was also found (X2(1) = 17.760, df= 6, p<.05). Participants who reported their educational level to be primary or below primary were more likely to have lower medication adherence than participants who reported a higher education level.
6.1.8 Relationship between blood pressure and medication adherence
In Table 6, a Pearson correlation coefficient was calculated to determine any association between systolic blood pressure and medication adherence. A weak negative correlation was found (r (198) = -.204, p<.05), indicating a statistically significant inverse relationship between the two variables. The higher the systolic blood pressure, the lower the adherence scores.
A Pearson correlation coefficient was calculated to determine any association between diastolic blood pressure and medication adherence. A weak negative correlation was also found (r (198) = -.237, p<.05), indicating a statistically significant inverse relationship between the two variables. The lower the diastolic blood pressure, the higher the adherence scores.
7. Summary of Results and Discussions
The purpose of this study was to investigate factors associated with medication adherence among hypertensive adults in the North West Region of Cameroon. The study was guided by Bandura’s theory of self- efficacy. Self-efficacy is "the belief in one’s ability to organize and execute any courses of action required to manage a situation [14]. The principle behind self-efficacy is that, behavior is influenced and could be modified by expected gained from that modification. Therefore, the belief that blood pressure could be controlled by adhering to medication regimen could become the stimulus to trigger a hypertensive patient to adhere to medication. Self-efficacy has been recognized as a predictor of health behavior [15]. Patients with high self-efficacy have been found to have higher adherence rate than those with low self-efficacy [17]. In this study patients were considered efficacious when the adherence score was greater than 6 [1] and accompanied with a normal blood pressure i.e. BP <140/90 [25,4,26]. Approximately 68.5% of participants (n=137) had adherence score >6 and considered adherent - the higher the adherence score, the lower the blood pressure reading. This findings support the concepts of selfefficacy and medication adherence.
This study utilized the 8 item self-reported Morisky Medication Adherence Scale (MMAS-8) questionnaire to investigate factors associated with medication adherence among hypertensive adults in the North West Region of Cameroon. Adherence scores were assessed as low (< 6), medium (6 - < 8) and high (= 8) [1]. Patients with scores greater than six (6) were considered adherent to anti-hypertensive medications. In comparison with other studies, adherence in this study was found in 68.5% of participants, which was higher than WHO global adherence estimates of 48-50% [18]. This finding is similar to adherence rates (67%) reported among hypertensive adults in a recent cross sectional survey conducted in Palestine using the MMAS-8 scale [27]. Similar adherence rates of 41% – 71% have been reported in other studies using the MMAS-8 [27,21,28,29]. While others have also reported similar adherence rates of 51% - 60% from other developing countries [30-32].
Numerous studies have evaluated demographic variables associated with medication adherence among hypertensive adult specifically, age, gender, marital status, occupation, income, education [31,21,33,34,35] using different adherence measures. The authors in this study found a statistically significant (X2(1) = 17.760, df = 6, p<.05) association between level of education and medication adherence. The more educated the participants the higher the adherence score. Karakurt et al. [31] found similar results among hypertensive adults in Turkey - education level was significant at (X2 = 20.815 SD = p <0.01). Ironically, approximately 67% of participants recorded their education level to be primary (6th grade) or below primary education.
Education and literacy has a direct impact on adherence [36]. Mancuso & colleagues [37] conducted a longitudinal study examining health literacy and asthma outcomes; the researchers reported that low health literacy was associated with poor asthma outcome. While individuals with limited health literacy or education may come from many walks of life, the problem of limited health literacy is often greater among older adults who are more likely to have limited education, and English proficiency [38]. In this study, the mean age was approximately 62 years. Among participants who were considered adherent (68.5%, n=137), the majority (45%, n=62) were between 55- 69 years. Our finding was similar with a previous study in a Palestine population using the MMAS-8 [39]. In that study, 46% of participants reported education, level of primary or below and mean adherence score was 4.5-8.
The ability to read and understand medication labels and treatment recommendations is crucial in improving adherence, it is therefore important for health care providers to provide instructions to patients at the grade level that is understood by the patients.
With regards to alcohol consumption, approximately 64%, (n = 127) reported that they did not drink alcohol. We assessed only history of drinking habit - “Do you drink alcohol” and possible response were either “yes” or “no”. A statistically significant inverse relationship was found (X2 = 10.226, df = 2, p<.05). As alcohol use increases, medication adherence rate decreases.
Studies, which have reported relationship between alcohol and adherence, have been primarily on HIV medications [40,41]. A recent systematic review of literature by Grodensky [41] failed to identify that none of the HIV studies addressed alcohol use and medication adherence. The researchers suggested that there is a need for further rigorous studies in the HIV diseases.
Problems with drinking alcohol also has significant implications for clinicians in terms of medication adherence because of potential for alcohol and drugs interactions, and high probability of patients forgetting to take their medication due to alcohol intoxication. In this study, though there was a statistically significant interaction in alcohol and medication adherence (X2 = 10.226, df = 2, p<.05, the percentages of people who reported drinking alcohol was relatively small. An anecdotal reason for this may be because patients are reminded, on a routine basis, at every clinic visit to refrain from drinking alcohol while on medications.
8. Conclusion
Medication adherence is an essential population health strategy in addressing worldwide epidemic of chronic diseases and related complications associated with non-adherence. These complications include but not limited to cardiovascular diseases, kidney diseases, stroke, premature morbidity and mortality. Though medication has been shown to slow disease progression, non-adherence remains a major global health problem [18,26]. This study results showed that majority (68 %, n = 137) reported a higher medication adherence rate among hypertensive adults in North West Region Cameroon. Though many variables have been found to be contributory to medication adherence in the western region, only education and alcohol were shown to be at the statistically significant level (p=.05) in this study.
Long-term reduction strategy focused in identifying factors associated with medication adherence might underscore its important in hypertension control. Efforts focused on customized intervention programs may likely improve patient outcome and provide major benefits in global hypertension control efforts.
Competing Interests
The authors declare that they have no competing interests.
References
- Morisky DE, Ang A, Krousel-Wood M, Ward HJ (2008) Predictive validity of a medication adherence measure in an outpatient setting. Journal of Clinical Hypertension10: 348-354 [CrossRef] [Google Scholar] [PubMed]
- World Health Organization (2002) Reducing risks, promoting healthy life. Geneva Switzerland [Google Scholar]
- Addo J, Smeeth L, Leon DA (2007) Hypertension in Sub-Saharan Africa: A systematic review. American Heart Association 50: 1012-1018 [CrossRef] [Google Scholar] [PubMed]
- The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: JNC-7 report. NHLBI [View]
- World Health Organization Report (2013) A global brief on Hypertension: silent killer, global public health crises. World Health Day: Geneva, Switzerland [Google Scholar]
- Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, et al. (2005) Global burden of hypertension: Analysis of worldwide data. The Lancet 365: 217-223 [CrossRef] [Google Scholar] [PubMed]
- Chockalingam A, Campbell NR, Fodor JG (2006) Worldwide Epidemic of Hypertension. The Canadian Journal of Cardiology 22: 553-555 [CrossRef] [Google Scholar] [PubMed]
- Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJ, et al. (2002) Comparative risk assessment collaborating group: Selected major risk factors and global regional burden of disease. The Lancet 360: 1347-1360 [CrossRef] [Google Scholar] [PubMed]
- Kengne AP, Awah PK, Fezeu L, Mbanya JC (2007) The burden of high blood pressure and related risk factors in urban Sub-Saharan Africa: Evidences from Douala Cameroon. African Health Sciences 7: 38-44 [CrossRef] [Google Scholar] [PubMed]
- Chapman RH, Benner JS, Petrilla AA, Tierce JC, Collins SR, et al. (2005) Predictors of adherence with antihypertensive and lipid-lowering therapy. Arch Intern Med 165-1147-1152 [CrossRef] [Google Scholar] [PubMed]
- Richter A, Anton SF, Koch P, Dennett SL (2003) The impact of reducing dose frequency on health outcomes. Clinical Therapy 25: 2307-2335 [CrossRef] [Google Scholar] [PubMed]
- Grant RW, Devita NG, Singer DE, Meigs JB (2003) Polypharmacy and medication adherence in patients with type-2 diabetes. Diabetes Care, 26: 1408-1412 [CrossRef] [Google Scholar] [PubMed]
- Bandura A (1977) Self-efficacy: Toward a unifying theory of behavior change. Psychological Review 84: 191-215 [View]
- Bandura A (1982) Self-efficacy mechanism in human agency. American Psychology 37: 122-147 [CrossRef] [Google Scholar]
- Strecher VJ, DeVellis BM, Becker MH, Rosenstock IM (1986) The role of self-efficacy in achieving health behavior change. Health Educ Q Spring 13: 73-92 [CrossRef] [Google Scholar] [PubMed]
- Kobau R, Dilorio C (2003) Epilepsy self-management: a comparison of selfefficacy and outcome expectancy for medication adherence and lifestyle behaviors among people with epilepsy. Epilepsy Behavior, 4: 217-225 [CrossRef] [Google Scholar] [PubMed]
- Schoenthaler A, Chaplin WF, Allegrante JP, Fernandez S, Diaz-Gloster M, et al. (2009) Provider communication affects medication adherence in hypertensive African Americans. Patient Education and Counseling 75: 185-191 [CrossRef] [Google Scholar] [PubMed]
- World Health Organization (2003) Adherence to long term therapies: evidence for action. WHO report Geneva, Switzerland: World Health Organization [Google Scholar]
- Osterberg L, Blaschke T (2005) Medication adherence. New England Journal of Medicine. 353: 487-497 [Google Scholar]
- Horne R (2006) Compliance, adherence, concordance: Implications for asthma treatment. Chest 130: 65-72 [CrossRef] [Google Scholar] [PubMed]
- Lee GKY, Wang HHX, Liu KQL, Cheung Y, Morisky DE, et al. (2013) Determinants of medication adherence to antihypertensive medications among a Chinese population using Morisky Medication Adherence Scale, PLoS ONE 8: e62775 [CrossRef] [Google Scholar]
- Cameroon National Statistics [View]
- Krousel-Wood M, Thomas S, Muntner P, Morisky D (2004) Medication adherence: a key factor in achieving blood pressure control and good clinical outcomes in hypertensive patients. Current Opinion in Cardiology 19: 357-362 [CrossRef] [Google Scholar] [PubMed]
- SPSS Inc (2009) PASW Statistics for Windows, Version 18.0. Chicago: SPSS Inc
- Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, et al. (2003) The seventh report of the Joint National Committee on the prevention, detection, Evaluation and treatment of high blood pressure. Hypertension 42: 1206-1252 [CrossRef] [Google Scholar] [PubMed]
- World Health Organization Report (2013) A global brief on Hypertension: silent killer, global public health crises. World Health Day: Geneva, Switzerland [Google Scholar]
- Zyoud SH, Al-Jabi SW, Sweileh WM, Morisky DE (2013) Relationship of treatment satisfaction to medication adherence: findings from a crosssectional survey among hypertensive patients in Palestine. Health and Quality of Life Outcomes 11: 191-197 [CrossRef] [Google Scholar] [PubMed]
- Williams NJ, Jean-Louis G, Pandey A, Ravenell J, Boutin-Foster C (2014) Excessive daytime sleepiness and adherence to antihypertensive medications among Blacks: analysis of the counseling African Americans to control hypertension (CAATCH) trial. Patient Preference and Adherence 8: 283-287 [CrossRef] [Google Scholar] [PubMed]
- Hyre AD, Krousel-Wood MA, Muntner P, Kawasaki L, DeSalvo KB (2007) Prevalence and predictors of poor antihypertensive medication adherence in an urban health clinic Setting. The Journal of Clinical Hypertension 9: 197-186 [CrossRef] [Google Scholar] [PubMed]
- Ibrahim OM, Jirjees F, Al-Obaidi H (2011) Barriers affecting compliance of patients with chronic diseases: A preliminary study in United Arab Emirates population. Asian Journal of Pharmaceutical and Clinical Research. 4: 42- 45 [Google Scholar]
- Karakurt P, Magfiret K (2012) Factors affecting medication adherence in patients with hypertension. Journal of Vascular Nursing 30: 118-126 [CrossRef] [Google Scholar] [PubMed]
- Ramli A, Ahmad NS, Paraidathathu T (2012) Medication adherence among hypertensive patients of primary health clinics in Malaysia. Patient Preference and Adherence 6: 613-622 [CrossRef] [Google Scholar] [PubMed]
- Wong MC, Jiang JY, Griffiths SM (2011) Factors Associated with Antihypertensive Drug Compliance in Chinese Patients: A Cohort Study. Journal of Clinical Pharmacy & Therapeutics 36 179-186 [CrossRef] [Google Scholar] [PubMed]
- Vlasnik JJ, Aliotta SL, DeLor B (2005) Medication Adherence: Factors influencing compliance with prescribed medication plans. TCM 22: 47-51 [CrossRef] [Google Scholar]
- Osamor PE, Owumi BE (2011) Factors associated with treatment compliance in hypertension in Southwest Nigeria. Journal of Health, Population, & Nutrition 29: 619-628 [Google Scholar] [PubMed]
- Institute of Medicine (2004) Health Literacy: A Prescription to End Confusion [View]
- Mancuso & Rincon (2006) The impact of health literacy on longitudinal asthma outcomes. Journal of General Internal Medicine 21: 813-817 [Google Scholar]
- Nielsen-Bohlman L, Panzer AM, Kindig DA (2004) The Extent and Association of Health Literacy
- Ibrahim OHM, Jirjees FJ, Mahdi HJ (2011) Barriers affecting compliance of patients with chronic diseases: A preliminary study in the United Arab Emirates (UAE) population. Asian Journal of Pharmaceutical and Clinical Research 4: 42-45 [Google Scholar]
- Cook RL, Sereika SM, Hunt SC, Woodward WC, Erlen JA, et al. (2004) Problem Drinking and Medication Adherence Among Persons with HIV Infection. Journal of General Medicine [CrossRef] [Google Scholar] [PubMed]
- Grodensky CA, Golin CE, Ochtera RD, Turner BJ (2012) Systematic Review: Effect of Alcohol Intake on Adherence to Outpatient Medication Regimens for Chronic Diseases. Journal of Studies on Alcohol and Drugs 73: 899-910 [CrossRef] [Google Scholar] [PubMed]