1. Statement of the Problem/ Issue
Innovative nurse practitioner (NP) roles continue to evolve across all health care sectors, provincially and internationally. Nurse Practitioners started in primary care. Other sectors have found the NP role valuable for patients and are following suit. Nurse Practitioners practice autonomously in some jurisdictions and practice settings as the most responsible provider. The NP frontiers of community driven primary care have now intersected with hospital and long term care. Hospitals deliver primary, secondary and tertiary care services. Portals of NP access span outpatient care; emergency and ambulatory clinics, to inpatient care; admission, management, and supporting patient discharges. Academic and community hospitals, in both rural and urban settings have overlapping common, yet unique care populations that NPs can support. The transitional hospital journey through acute care, post-acute, alternate levels of complex chronic care and end of life care for seniors who are not able to return to their homes are the challenging lived realities. Maximizing NP health human resource contributions to improve hospital care for patients, families and teams is key. Autonomous and collaborative interprofessional models of care in the form of consultation, shared care or as the formal most responsible provider are quality solutions [1-7].
2. Statement of Purpose
This aim of this research is to examine patient, family and staff experiences with the quality of Nurse Practitioner care provided as the Most Responsible Provider for hospitalized seniors. Targeting the hospital NP Model of care as the MRP intervention is the goal.
3. Conceptual Theoretical Framework
The Shuler Nurse Practitioner Practice Model theoretical framework is relevant and effectively blends with the NP as MRP practice model. The model synergizes with the APN dimension of practice recognizing clinicians, educators and researchers. The metaparidigm of nursing visualizes the NP expansion of nursing knowledge and skills into medicine. The theoretical model constructs includes holistic patient care needs, NP and patient interactions, self-care, health promotion and prevention, and wellness. Furthermore, the person is viewed from a holistic lens as a rational being with intrinsic value and worth. Health trajectories can span from restoration, maintenance, wellness, episodic, and comprehensive care. Nursing is a profession and follows a process focus. The model guides how patient interaction, assessment, intervention and evaluation should occur with wellness, and acute and chronic illnesses. Lastly, the environment is recognized as affecting people [8].
4. Significance and Justification
Rationale for this study relates to the limited understanding of the Nurse Practitioners as the Most Responsible Provider from hospital admission, during treatment, and until discharge. Scientific background to the study reveals that evidence for NP based hospital roles positively impacting patient care do indeed exist. Information regarding NPs practicing in MRP roles in pockets of primary care is found in the literature.
Hospital based NP roles have only been evaluated in the context of consultative or shared care with physicians and teams. Forecasted significance of this study relates to learning about NPs functioning at their maximal scopes of practice as the MRP, and the value added quality caring hospital experience. Nurse Practitioners are an innovative safe solution to meet the hospital care needs of senior or those living with chronic diseases.
5. Education and NP Practice Domains
Nurse Practitioners are competent and caring clinicians. Their value added advance practice nursing (APN) dimensions maximize their scope of contribution for care impacts. The Canadian Nurses Association (CNA) highlights four valued competencies that NPs anchor their roles within. These domains are based upon NP depth, breadth and range of nursing knowledge, theory and research. These advanced competencies enhance their clinical experience predominately, as well as other non-clinical dimensions of practice. The domains of clinical, research, leadership, and consultation/ collaboration competencies are core pillars strengthening NP practice [9]. Nurse Practitioner competencies build upon their expertise as Registered Nurses (RNs), with expanded practice dimensions previously associated with medicine to merge within the NP role [10]. Nurse Practitioner educational entry to practice expectations has shifted from baccalaureate to graduate/masters preparation in Canada. In the United States, the expectation is a Doctorate of Nursing Practice (DNP) by 2015 [11].
6. Ontario NP Landscape
As of March 2012, 2,259 NPs are registered to practice in Ontario [12]. Four (4) NP Specialties exist within the RN Extended class (RNEC).
The title Nurse Practitioner is protected. Of these specialties, the NP-Primary Health Care (PHC) has the largest numbers (1,632), followed by the NP–Adults (441) and then NP – Pediatrics (200). The final specialty, NP–Anesthesia has graduated two classes and registration is underway presently in Ontario. The number of NPs in Ontario has doubled from 1,344 to 2,777 between 2007 and 2011 [13]. This reflects increased provincial investment in NPs, however, they still account for only 1% of all Registered Nurses (RNs) in the province [10]. In 2012, 1,874 NP were on the job in Ontario compared to 729 in 2007. More than half of NPs work in community practice [14]. The CNO practice standards for NPs are generalized to all specialties and delineate the controlled acts and competencies authorized for NPs [10].
A paradigm shift regarding the divide traditionally associated with practice settings is narrowing with the alignment of the NP specialties in all geographical practice settings [1].
The notion that NP PHCs can only practice in communities, and NP Adult or NP Pediatrics are only authorized to practice in hospitals is diluting. Nurse Practitioner knowledge as generalists or specialists can be portable, transferrable and responsive to care needs of a variety of patients in diverse settings. Professional self- regulation as NPs and matching competence and confidence for care delivery accountabilities is the expectation.
7. Authorized Controlled Acts for NPs
In Ontario NPs are authorized by regulation to perform seven controlled acts.
These include 1) communicating a diagnosis; 2) performing a procedure below the level of the dermis, 3) insertion into a body orifice, 4) application of prescribed energy, 5) setting or casting, 6) administration of a substance by injection or inhalation and lastly 7) prescribing, dispensing or compounding drugs [10]. Federal approval for prescribing Controlled Drugs and Substances is granted in early 2013. Provincial regulations for NP prescribing authorization are underway. They are essential for acute and chronic pain and symptom management across all care settings [10].
8. Ontario’s Senior Health Care Strategy
The Action Plan for Health Care in Ontario has changed how it funds hospitals. The historical global funding is shifting to funding based on the volume of patients seen and on the quality of services delivered. The recently launched Ontario Seniors Care Strategy targets helping seniors to stay healthy and live longer with supports to optimize independence [5,15].
Ontario’s seniors aged 65 and over are expected to double by 2036. More than 20% of seniors, who are considered frail, are expected to triple in Ontario’s oldest, aged 90 and over. Frailty is associated with the presence of multiple chronic health conditions, vulnerability to loss of function, and greater health care needs [16]. Care of adults is core health call business.
Seniors account for 63% of acute inpatient days and 43% of provincial health expenditures. They face a twofold risk for adverse events, surgical complications, loss of independence, increased lengths of stay and readmissions. Ontario hospitals report their total inpatient days accounted for by seniors’ averages 43 % to 73 % [16].
Hospitals report that the proportion of seniors accounting for nonacute hospital stays, also referred to as alternate level of care (ALC) days range from 71% to 89 %. Geriatric hospital care has demonstrated positive outcomes including cost effectiveness, improved physical and cognitive function, decreased rates of institutionalization, decreased length of stay, improved patient and family satisfaction, better human resource knowledge and retention, and improved collaboration [16,17]. Ensuring an NP workforce prepared to care for older adults is a social imperative [18].
9. Research Study Objectives
- To determine patient, family and staff satisfaction with the quality of care provided by NP as the MRP in a community hospital in Ontario.
- To correlate scores on NP satisfaction survey responses between staff, patients and families.
- To quantify the number of patients admitted, treated and discharged by the NP as the MRP
10. Definition of Term
Most Responsible Provider (MRP) definition encompasses primary responsibility and consistent care assumed by the NP across the care trajectory during admission, treatment, diagnostics, diagnosis, prescribing, and discharge.
11. Limitations
Information embedded in this research was limited to one hospital site in Ontario for this pilot study. Data accuracy captured electronically for admissions, expirations, and discharges was reliant on valid coding health records documentation or decision support data extraction and analysis. Human error and technological inaccuracies have a potential to impact the reliability of the data secured. Survey responses are individualized based on perceptions, experiences and practices. The potential for bias must be acknowledge as an employee and researcher of the hospital surveyed. Researcher vigilance to mitigate bias remain objective and adhere to research principles for reliability and generalizability was upheld.
12. Review of Literature
A literature search was conducted both independently and jointly with a Hospital Librarian to improve the research yield. The APN McMaster Database searched CINAHL, Embase, and MEDLINE. PubMed and Evidence Based Medicine included the Cochrane Database of Systematic Reviews for English language articles published in the last five (5) years. Landmark sentinel literature beyond five (5) years that informed the research inquiry was considered for inclusion. Search terms included Nurse Practitioner OR Advanced Practice Nursing OR Physician to retrieve articles examining NP/MD roles.
The search retrieved 339 articles of which ten (10) were selected for further review. The APN Literature Database yielded another 12 from 238 articles. CINHAL search yielded nine (9) titles reviewed from 191 results. Search criteria NP AND Hospital yielded 254 results, 14 articles were selected to review. Controlled Vocabulary Medical Subject Headings (MeSH) included (nurse practitioner, length of stay, attending physician, and hospital) in MEDLINE. Nurse Practitioner OR Advanced Practice Nurse keywords/titles in Cochrane Library were utilized. Google scholar search engine yielded two (2) relevant unpublished articles. Two (2) Ontario dissertations and one (1) article in press on hospital based NP roles were reviewed.
The total sample of articles yielded was N = 833. Inclusion criteria included Nurse Practitioner, hospital focused, most responsible provider/practitioner and care of the older adult/seniors. Exclusions related to noncomparable models of care or staff mix of n = 795 (833- 38). A subsample of articles n = 38 were analyzed for inclusion and then a decision was struck to include 12 for relevancy and criteria fit. Thirteen (13) studies met inclusion criteria: three (3) randomized controlled trials, two (2) mixed methods, two (2) descriptive surveys, 2 systematic literature reviews, one (1) pilot study, one (1) retrospective study and two (2) descriptive case studies.
13. NP as Most Responsible Provider & Patient Care Accountability
The NP as the most responsible provider must be clearly established and communicated. Responsibilities for patient care upon admission include comprehensive history taking, provisions for ordering diagnostics tests, prescribing medications and treatments, rendering provisional diagnosis, regular care monitoring, documentation during hospital care until discharge, ensuring on call coverage, thorough dictation and completion of the medical record upon discharge, and concluding with linkages to relevant community primary care providers and resource services or referrals to specialists for transfer of accountability and responsibility [6,7]..
A hybrid range of NP models of care delivery exist. Nurse Practitioners may function in a short term consultative model similar to specialists; and they may support admission and treatment in a shared care dyad with a physician colleague. Nurse Practitioners that are involved in shared care may also discharge the patient with prescriptions, necessary referrals and linkages to community resources.
To date only a few hospital organizations with Ontario NPs leading as early adopters are designated as the MRP. The designation MRP can be used interchangeably with Most Responsible Provider/ Practitioner. The term is not legally defined; however the MRP refers to the provider who has primary responsibility and accountability for the care of a patient within the hospital [7].
Lakeridge Health NP- Led Hospital Model of Care in Whitby, Ontario is the first pioneering hospital to showcase their senior care delivered by NPs as the MRP. They were granted full admitting rights through organizational supports in July 2012 [6]. In the free standing specialty hospital, complex continuing care, rehabilitation, geriatric patients and interprofessional teams are experiencing the positive outcomes of an NP as the MRP. Both provincial and national accolades have been received by dignitaries. Shadowing experiences from other provincial hospitals have occurred including national interest from Israel and Australia. The status quo has been disrupted through richening patient care access and choice with NP admission privilege power through courageous change. Hospital gate keeping influences through cultural shifts, increased awareness and championing leadership for access and equity in supporting patient care is being realized.
14. Future Research
Future research opportunities are rich. A focus on capturing the extent that hospital NPs function as both the formal and informal MRP is needed. Highlighting the barriers and facilitators for role functioning, for both NP staff employees and NP non-employee privileged staff would be informing. Studying from the lens of both academic and community hospital nuances, models of care, clinical subspecialties, role domains, levels of specialist consultation, NP leadership enablement, Chief Nurse Executive(CNE) & NP governance, fiscal considerations, NP mentorship, satisfaction (patient, staff, NP), hospital and Local Health Intigration Networks(LHIN) outcome indicators and lastly NP recruitment and retention.
15. Limitations
The literature synthesis highlighted only four (4) original studies including Ontario hospitals [1,2,19,20] Two (2) studies included NPs in Ontario hospitals [21]. One study included Quebec hospital NPs [22]. No studies identified the NP as the formal MRP.
Although some of the research combines both teaching and academic hospital models of care, focusing presently solely as the NP MRP may threaten generalizability to hospitals where staff mix and models of care may vary. The literature predominately focuses on NP roles in academic hospitals. A focus on Ontario and Canadian hospital roles highlighted the lack of research for NPs as MRPs.
16. Research Methodology
16.1 Setting
The study setting ocured in a small free standing specialty community hospital without access to an attached emergency department.
The model of care is an NP- Led hospital in the Central East Local Health Integrated Network in Ontario, Canada. The NPs have been enabled and empowered deliver senior care as MRPs since the proclaimed legislative and regulatory authorizations in July 2012. The hospital celebrated a successful shared care NP & MD model of care from 2008 until 2012. NPs admit, treat and discharge patients requiring alternate level of care, complex continuing care and geriatric rehabilitation care.
16.2 Population and sample
The population focus is directed towards seniors, over the age of 65, admitted as inpatients. The bed capacity is 74. There are 26 beds on the third floor focusing on Geriatric Rehabilitation/Restorative Care with the goal aimed at discharging home. The fourth floor has 48 patients, 24 per unit. One of the units is secured for managing dementia and responsive behaviors. Patients are Alternate Level of Care (ALC)/Complex Continuing Care (CCC) awaiting Long term care (LTC) or face long term hospitalization due to complex resource intensity and care resources.
Multiple complex comorbidities and frailty syndromes are the seniors lived reality with vascular disease (dementia, stroke, cardiac, renal, diabetes) and pulmonary diseases. Musculoskeletal challenges associated with falls and impaired mobility. Neurological functional limitations with instrumental and basic activities of daily living related to cognitive impairments are experiences. Challenging responsive behaviours, fluctuating capacity and polypharmacy management increase the complexity of care. End of life and palliative care are also delivered for symptom management and comfort care.
The NP team includes three full time MRPs with primary health care and/or adult extended class specialties. The collaborative interprofessional team includes Nursing, Pharmacist, Physiotherapist, Occupational Therapist, Recreational Therapist, Dietician, Speech Language Pathologist, Chaplain, Patient Care Specialist/Manager, Clerk, Personal Support Workers and a consulting specialist physician when required.
16.3 Research design
A mixed methods pilot study examined quantitative data related to the number of admissions and discharges and qualitative satisfaction surveys for patients, families and staff. Quantitative measures will calculate the number of NP admissions, discharges, and transfers from July 1, 2012 until December 31, 2013.
16.4 Study criteria
An inclusion criterion includes adults over the age of 65 admitted to the Nurse Practitioner as the Most Responsible Provider. Agreement to participate by staff, and patients if capable or by patient’s family as acting Power of Attorneys to complete the surveys. Participants are required to be fluent in English. Exclusion criterion includes refusal to participate and those who are non-English speaking.
16.5 Tools
Twenty staff and ten patient and family quantitative closed ended questions were designed. The surveys are rated on a Likert Agreement Scale with one qualitative open section. Rankings ranged from 1 strongly disagree, 2 somewhat disagree, 3 undecided, 4 somewhat agree to 5 strongly agree. The Flesch Kincaid Readability Score of surveys improved from the pilot surveys in 2005 which were Grade 12 level to a Grade 10 level when revising the survey for this study.
16.6 Recruitment
A research study letter and informed consent was provided to all participants on double noncarbonated record paper for the researcher to keep the original and participants to keep a signed copy. Surveys were sealed by respondents in an addressed envelope, returned directly to the Program Director/Administrative Assistant. A total of 125 surveys were utilized, 75 surveys were distributed to patients and families, and 50 to staff.
16.7 Data collection methods
The data set for analysis of admission, transfers, expiration/ deaths and discharges was supplied by the Hospital Decision Support Unit.
Survey tools for patient, family and staff were adopted from the Hospital NP Shared Care Model Evaluation in 2005 for the NP MRP formal model of care to facilitate readability, comprehension and ease of completion. Data was entered and calculations were performed in Microsoft Excel by the researcher. A data analysis imported the data into SPSS Version 22 (IBM, 2013) for further calculation performance.
Information pertaining to the study was provided by email communication prior to commencing the study and survey distribution. An Noncarbonated Record (NCR) information sheet detailing the intent of the study, and an informed consent to opt in or out of the research was also attached to each of the patient, family and staff surveys prior to completion, to facilitate the purpose of the research, maximize participation and allow the participant to keep a copy of the related study documents. Surveys were provided to all patient, family and staff participants as well as an addressed envelope for the results to be sealed and mailed directly to the Program Director/Administrative Assistance to promote confidentiality. Two reminder emails were issued to optimize participation.
A mixed methods design utilized qualitative surveys for patients, families, and team. A convenience sample size target for this pilot study of 75 patients, families and 50 staff. They were distributed by the nurses and managers. The pilot study surveys commenced from December 2013 until January 2014.
16.8 Human rights protection
The study utilized both primary data collection and secondary data analysis. Study approval was received from Capstone Academic Committee Members Dr. Dunford and Dr. Pomeroy. D’Youville College Internal Research Board full approval was granted October 2013. Hospital Research Ethics Board full approval was authorized in November 2013.
Researcher competency and safety certifications were obtained from the American National Institute of Health Clinical Research Training in May 2013 and the Canadian Tri-Council Policy Statement on Ethical Conduct for Research in June 2013. A proactive Ontario Criminal Reference Check was conducted in September 2013 in an effort to mitigate human subject vulnerability representative for seniors.
16.9 Treatment of data
Subject data was maintained confidentially without identifiers. The computer was locked in an office. Data was encrypted and password protected. Research data will be maintained and shredded after six years according to Canadian requirements.
17. Results
17.1 Description of sample
Outcome 1: Quantify the number of patients admitted, treated and discharged between July 2012 & December 2013.
17.2 Patient demographics
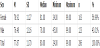
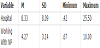
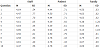
Third floor patients averaged 78.22 (SD = 11.00) years of age. This population was more rehabilitative or restorative care focused with a goal to be discharged home. Female patients averaged 81.06 (SD = 10.59) years of age representing 48.15% of the floor, while males were 75.58 years old (SD = 10.76) representing 51.85% of patients. The patient demographics for floor 3 are displayed in Table 1.
Fourth floor patients averaged 77.87 (SD = 11.70) years of age. This population consisted of more complex continuing care patients awaiting long term care (LTC), or those who were resource intensive and not suitable for LTC. Females on this floor averaged 78.92 (SD = 11.27) years of age representing 56.99% of the floor, while males were 76.48 (SD = 12.16) years of age and represented 43.01% of the floor. The patient demographics for floor 4 are displayed in Table 2.
17.3 Admissions
Total patients admitted (N = 602) by NPs were examined for the last six months of 2012 and the 2013 calendar year. Specifically, NPs admitted 189 from July 2012 through December 2012. In the calendar year 2013, NPs admitted 413 patients. The NPs averaged 33.4 (SD = 4.25) admissions monthly.
17.4 Discharges
The total number of discharges performed by NPs, was examined during the same time period as admissions. NPs discharged 555 patients from July 2012 until December 2013 to their own homes, retirement homes or nursing homes. From July 2012 until December 2012, 145 patients were discharged. Another 410 patients were discharged from January through December 2013. An average of 30.8 discharges per month occurred.
17.5 Expirations
The total number of deaths was examined during the same time period as the admissions and discharges. Three patients expired within the time frame of July 2012 until December 2012, and 22 patients expired during the calendar years 2013. A total of 25 patients died from July 2012 to December 2013 resulting in an average of 1.4 patients expire per month.
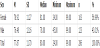
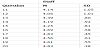
A total of 45 patients were transferred to an acute care facility such as the emergency department or for diagnostic testing at another hospital site. Overall, from June 2012 until December 2013, the average of 2.5 patients per month were transferred. More specifically, from June 2012 until December 2012, 19 patients required transfer out, the remaining 26 transfers occurred during 2013. Table 3 details patient discharges and deaths by floor.
Outcome 2: Outcome from satisfaction surveys.
17.6 Characteristics of staff
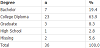
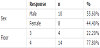
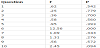
The education attainment of surveyed staff included: 4.3% graduate prepared, 10 % baccalaureate, 32.9 % college diploma, and 1.4 % were high school graduates (Table 4). Staff have been employed at the hospital for a mean of 8.33 years (SD = 8.09). They have worked with an NP (e.g., exposed to NP practice experience and established role expectations) for an average of 4.27 years (SD = 3.14). Table 5 details the years employed and years working with NP. Overall, 16.6% (n = 6) of the staff worked on both floors, while the remaining 83.33% (n = 36) work only on one floor.
17.7 Characteristics of patient sample
The demographics of the surveyed patients are presented next. More males (n = 10) versus females (n = 8) responded to the survey. A greater percentage of the fourth floor patients responded to the survey (77.8%) compared with the third floor (22.2%). Table 6 details the patient response to the survey.
17.8 Characteristic of family sample
All survey respondents were from the patients’ designated Power of Attorneys (POA). The POAs rated six patients incapable, while the remaining 10 patients were perceived as capable (Table 7); whereas, all patients were deemed clinically incapable by the attending MRP.
17.9 Outcomes of Research Questions
17.10 Results of survey responses
Ultimately, the attending NP, serving as MRP, clinically evaluated each patient to determine participant’s capacity, irrespective of the POA’s analysis. Accordingly, only 26 patients were deemed capable of completing their own surveys, of which 18 participated. Thus, 69 % of patients completed their own survey. Family surveys responses were completed by designated POAs, some in tandem with incapable patients (16 out of a possible 39). Five families declined/opted out of the research for an undisclosed reason. Eligible family participation rate was lower at 41%. Reduced availability of POAs limited response rate. Staff response rates were 36 out of a possible 50 equating to a good 72% response rate.
The Likert scale findings showed a strong higher trend toward strongly agree responses. The frequency of strongly agree (5) was higher than somewhat agree (4) for survey questions. Question 12 (The NPs reduce transfers to the Emergency department was the only item that somewhat agree (4) was greater than strongly agree (5).
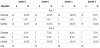
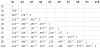
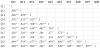
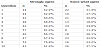
Cronbach’s test of internal reliability was performed on all surveys. A reliability score of a = 1 is the perfect scenario representing 100% for internal consistency. Cronbach’s alpha for the 20 survey questions was high, a =943. A correlation matrix, depicting the direction and strength of association between each question, was created for questions 1 through 10 (Table 8) and questions 11 through 20 (Table 9).
Outcome 3: Outcomes of correlated surveys.
Table 10 displays the average responses to questions 1 through 10 by respondent. Table 11 details the average response to questions 11 through 20 for the staff respondents.
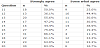
The frequency and percentage of strongly agree and somewhat agree responses for questions 1 through 10 are displayed in Table 12 and questions 11 through 20 in Table 13.
A one-way analysis of variance (ANOVA) with category of respondents (staff, patient, or family) as the independent variable and question 1 through 10 as the dependent variables was conducted to determine whether the three categories of respondents significantly differed. Because the category of respondents exceeded two groups, the ubiquitous t-test was inappropriate. The responses to question 6 (NPs are approachable) were statistically significantly different, F (2, 67) = 12.56, p < .001, and the responses to question 10 (overall satisfied with NP care) approached statistically significant differences, F (2, 67) = 2.45, p = .094.
Bonferroni post hoc comparisons of the three categories of respondents to question 6 indicate that the staff responses were statistically significantly different from the family responses (Mdiff = .764, SE = .165) at p < .001; the patient responses were significantly different from the family responses (Mdiff = .819, SE = .189) at p < .001. A means plot comparing the responses to question 6 is displayed in Figure 1, and Figure 2 displays a means plots of the responses to question 10. Table 14 displays the outcomes of the ANOVAs. Tables 15 and 16 display the survey questions from 1 through 10, and 11 through 20.
17.11 Qualitative thematic findings?
Wordle was utilized for word cloud generation of patient, family and staff qualitative survey responses. Survey text responses were inserted to generate the three word clouds which give greater prominence to words that appear more frequently.
Patient word clouds in Figure 3 showed high frequency representation of family care, approachable, necessary, and treatment. Frequent large font word clouds generated for family surveys in Figure 4 included NP, NP names, care, happy, family, and addresses concerns. Medium sized font word frequency illustrated respectful, friendly, prompts, helpful, informative, and great just to capture a few. Staff survey responses highlighted frequent mention of NPs, team care, great, and professional in Figure 5.
Patient survey qualitative responses: Survey verbatim quotations shared include:
Positive Exemplars:
Satisfaction with care
- X is very pleased about the care that x provides.
- Very satisfied with NP. She is very approachable and explains health issues all the time.
NP advocacy
- X was a solid advocate who really stepped up to achieve the necessary treatment I required. She followed my progress daily and intervened with med adjustments and outside contacts to obtain necessary treatment. Her determination to re-enact ECT to dispel my psychotic episode has made a world of difference.
Professional virtues & attributes
- Compassionate, responsive to inquiries and concerns, approachable, collaborative approach to treatment includes patient/family.
- NP is extremely caring, kind, considerate of family needs.
- Very approachable. Consults with families. I find the NPs to be more approachable than doctors and try very hard to communicate with patients overall. I believe this model of care to be the best. They explain medical problems and treatments effectively and frequently inform family of how the patient is doing. The only concern is sometimes being short staffed but this is not though fault of their own. I hope this model of care becomes more prevalent in Canada.
NP responsiveness
- Having an NP present on the floor allows timely patient care and support for the care team.
Patient Opportunities for Improvements:
Communication
- Better communication and final check should be completed before patient is transferred to another hospital, unit, and ambulance.
- I would like to see weekly meetings or emails sent to families explaining what is happening as patient can’t remember and family hours don’t connect with NP.
18. Family Survey Qualitative Responses:
Positive Exemplars:
Satisfaction with care
- Our family is very pleased with the care x has given to our mom. All the staff are very friendly and she is happy.
- You can always go to x about anything for concerns for my brother and x is right on it and things are done promptly.
- My father had several close calls and if the NP was not present or doing her job, dad would be long gone by now. Thank you to the NP and all staff.
- We are extremely happy with the NP and greatly relieved knowing she is always on the floor and very accessible. She has built a very good relationship with my mother, who we feel is more relaxed knowing the NP is there for her.
Family opportunities for improvements:
NP Role clarity
- NP role needs to be more clearly defined to family since this situation is atypical.
- My family members have had contact with 3 NPs over 3 months. One was more abrupt and not willing to spend time to listen to our concerns. We would assume the NP is in daily contact with the PSWs that are directly in contact with the patient regarding attitude, appetite, alertness, coherentness and general state of wellness. This information could be relayed to the family periodically so more information would lead to a better outcome for the patient. Not enough discussion before changes in medications.
19. Staff Survey Qualitative Responses:
Positive Exemplars:
Interprofessional
- As a pharmacist I value the interprofessional collaboration with the NPs to enhance patient outcomes.
Satisfaction
- Great to have you here. We can always count on you.
- I have thoroughly enjoyed working with x and the other NP and consider it an honour to be part of their team.
- I love the contribution of the NP program professionally and personally.
- More approachable, more rounded with info and more willing to consult as required. Less limited by professional ego which has been a common theme with some Drs.
- I really enjoy working with NPs because they are approachable, are available and easy to communicate your concerns with.
- I very much enjoy working with NPs. They are approachable and easy to have a dialogue with as an allied health professional.
- They are a great asset to the team. NPs should be on call for weekends as they know the patients, the on call Drs do not.
Knowledgeable
- It has been a privilege to work alongside the NPs. They are an excellent source of knowledge on the floor. They spend a good deal of time with our patients and fit very well into our multidisciplinary team.
- X is a very knowledgeable and approachable NP. I feel very comfortable around her and know that her experience, wisdom and knowledge add to her overall delivery.
Holistic patient centered care
NPs provide/apply a much more holistic approach to patient care due to their nursing background.
Staff opportunities for improvements
Advance directives
- I do not like that the NP fills out the advance directives before giving to families. It should be discussed with them first and I feel a prefilled form may influence what should be a personal decision and they may feel intimidated about choosing a different choice.
- Always make time to see every patient every day if not every other. They are a great asset when the doctor is unavailable.
20. Discussion
20.1 Study overview
Evidence for Nurse Practitioners (NP) hospital based roles positively impacting patient care exists. Information on the NP in the MRP role exists in pockets of primary care in Canada and the United States. NP hospital roles have only been evaluated in the context of consultation and shared care. There is limited understanding of the NP role from the MRP lens during care across the hospital trajectory.
This capstone was targeted at a quality initiative focusing on maximizing Nurse Practitioners scope of practice in hospitals. The study aim Nurse Practitioners as Most Responsible Providers: Impact on Care for Seniors Admitted to An Ontario Hospital was to examine patient, family and staff experience with the quality of NP care delivered as the MRP from admission to discharge. A mixed methods pilot study examined both quantitative and qualitative primary and secondary data sources. The three study objectives are to first, determine patient, family and staff satisfaction with the quality of care provided by NP as the MRP in a community hospital in Ontario. Second, to correlate scores on NP satisfaction survey responses between staff, patients and families. Lastly, to quantify the number of patients admitted, treated and discharged by the NP as the MRP. The Shuler Nurse Practitioner Model is the conceptual and theoretical model utilized to guide, shape and integrate with the NP as MRP practice constructs synergizing delivering advanced practice nursing with medicine scope of practice overlaps. The Shuler Nurse Practitioner Model is the conceptual and theoretical model utilized to guide, shape and integrate with the NP as MRP practice constructs synergizing delivering advanced practice nursing with medicine scope of practice overlaps.
Results of the comprehensive literature review undertaken to determine available quality research geared at answering: How Does the Nurse Practitioner as The Most Responsible Provider Affect Care For Seniors Admitted To Hospitals In Ontario Canada? A comprehensive literature search methodology was utilized to identify hospital studies. Studies describing NP models of care anchored in assuming most responsible practitioner roles with a focus on caring for seniors were targeted. Results revealed that 13 studies met inclusion criteria. Namely, three (2) randomized controlled trials, two (2) mixed methods, two (2) descriptive survey, two (2) systematic literature reviews, one (1) pilot study, one (1) retrospective study and two (2) descriptive case studies.
Data analysis results impressively captured a total of 602 admissions, 555 discharges, 25 deaths and 45 transfers occurred with NPs practicing as MRPs. The average senior was 78 years old. Survey response rates were 65%, families 41%, and staff 75%. Satisfaction surveys revealed staff worked with NPs for an average of 4 years. Chronbach alpha demonstrated high internal consistency across all groups (a .943). ANOVA analysis showed statistical significance with Question 6 NP approachability (p< .001). Bonferroni post hoc analysis revealed that staff responses statistically differed from family responses (P <.001). Correlation matrix of questions significant at both 0.05 and 0.01 levels (two tailed).
21. Implications for Practice
Implications for practice reveal that enabling, empowering and embracing NP maximal scope of practice contributions as the MRP can be valuable across the continuum of hospital experiences. NP care to meet complex senior care is a timely, safe and an innovative quality caring solution. Full implementation and sustainability for the model of care is a research rich area for exploration
Nurse Practitioners functioning in the MRP role strive for patient centered care, quality, experience and favorable outcomes. Enabling and empowering NPs to be champions of change for optimal patient and organizational success leverages their knowledge and leadership capacity. This is not about NP trailblazing; rather that it is paving the health path for seniors and capitalizing on NPs as health human resource champions. This is not about the transference of power, namely important prescriptive, diagnostic and admission privileges and authorities. It is about the power to deliver safe quality care and optimize care accountabilities. Care should not be defined by geography or boundaries of hospital practices. Nurse Practitioner competence and population needs should be the driver of meaningful change.
Strengthening the survey tools further would be ideal. Although the Flesch Kincaid Readability Score improved from the adopted pilot surveys in 2005 from a Grade 12 level to a Grade 10, gearing to a Grade 5 level would be ideal for health literacy comprehension and communication considerations. Also including senior friendly considerations such as larger font size for future research would be ideal. Staff education levels were surveyed, but patient and family participants were not. Adding this to future research would be informing.
The volumes of deaths expirations are low given the aging complex continuing care population with advance chronic disease. The majority of deaths occurred on the fourth floor as expected with ALC/ CCC populations including palliative care. This is related to advanced frailty syndromes including a plethora of moderate to severe dementia, multiple comorbidities, and polypharmacy experience by the seniors. Respecting advance directive care planning choices must also be realized. Advance directive opportunities to include a no emergency transfer option should be further explored. Future research ability to capture complexity of disease would be advantageous.
In terms of discharge potential, third floor patients comprised of rehabilitation/restorative care populations, and were more likely to be discharged home. The fourth floor patient’s composition included the ALC/CCC. Accordingly, fourth floor patients were more likely to be frail with progressive disease and faced long discharge times related to lengthy long term care placements lists, or care acuity and severity exceeded the resources capacity that LTC homes could deliver. These patients faced long term chronic hospital care.
The characteristic of staff warrants explanation. During the study period, the NP workforce demographics changed significantly. One seasoned expert NP retired and the second expert veteran NP was off for an extended period for a health related matter. To compensate for the NP staffing changes, two NPs were hired. Orientation and mentoring to building confidence in their competence to function in the MRP role was required.
In terms of the study patient sample, a greater percentage of fourth floor patients responded to the survey (77.8%) compared with the third floor (22.2%). This may be attributed to a seasoned NP and researcher working on the floor.
Family representation and lower response rate reasons may be attributed to patients needing assistance to complete the forms. The POAs wanted to include the seniors in decision making; but may not understand or appreciate the patient’s true capacity. This could be a potential future area for further research to capture capacity comprehension.
Patient survey response raises opportunities for improvements, especially for NP communication enhancements. There is a thirst for patient and family communication in terms of care updates and navigating the complex hospital system. Role overlap can synergize with NP role clarification to raise awareness and care expectations in terms of the NP comment and the interprofessional team contributions such as delineating the role overlap and differences between the NP to accepting MRP, RN to RN transfers of accountability during duration of stay and at time of discharge. The NPs meets with patients and families, a family conference is scheduled within a couple weeks of admission, and when required during treatment and changes in condition, to facilitate discharge planning.
Family opportunities identified for improving communication and role clarity and understanding are required in terms of the role of NP as MRP, scope of practice and model of care with interprofessional team compliments. On admission this is communicated to patients and families. The model of NP care is describe in the patient handbook prior to transfer and is available on the unit. A whiteboard for communication is utilized Including the NPs name.
22. Recommendations for Future Research
Future research opportunities are rich. A focus on capturing the extent that hospital NPs function as both the formal and informal MRP is needed to further explore the advance practice role contributions as the Most Responsible Provider for seniors hospitalized. A focus on merging both NP employees and NP privileged staff to enable hospital care for seniors would be strategic.
Highlighting the barriers and facilitators for role functioning, for both NP staff employees and NP non-employee privileged staff would be informing. Studying from the lens of both academic and community hospital nuances, models of care, clinical subspecialties, role domains, levels of specialist consultatation, NP leadership enablement, CNE & NP governance, fiscal considerations, NP mentorship, satisfaction (patient, staff, NP), hospital and LHIN outcome indicators and lastly NP recruitment and retention.
23. Conclusion
Nurse Practitioners are able to function as most responsible provider providing hospital care from admission through discharge with high patient, family and staff satisfaction and quality caring. A critical research opportunity exists to fully explore NP role contributions further as the MRP for hospitalized populations in both community and academic hospitals and for diverse population across the age span. Enabling, empowering and embracing NP maximal scope of practice contributions as the MRP can be valuable across the continuum of hospital experiences. NP care to meet complex senior care is a timely, safe and an innovative quality caring solution.
Competing Interests
The author declare that they have no competing interests.