1. Introduction
Traumatic brain injury (TBI) remains a significant cause of death and permanent disability worldwide. The Centers for Disease Control and Prevention (CDC) estimates that 1.7 million people in the United States sustain a TBI each year [1]. In the United States, sports-related TBIs estimated by 1.6-3.8 million annually, including those not treated by a health care provider [2,3].
TBI may be an acute and chronic process. Although the immediate consequences of brain injury can be devastating, long-term health disorders associated with TBI include posttraumatic stress disorder (PTSD), neurocognitive deficits, neurodegenerative diseases (Alzheimer's disease or Parkinsonism), psychosocial health problems (e.g. major depression, impairment of social functioning and ability to work and suicide), epilepsy, pain and other alterations in personality or behavior [4-6]. TBI is a multifaceted disease with prolonged secondary pathogenesis and long-lasting adverse neurological sequelae that remains a clinical challenge to manage.
Natural products and their active nutrients/components often cause possible improvement in most of the brain-related damages [7]. Omega-3 FAs are polyunsaturated fatty acids (PUFAs) having a double bond at the third position from the end of the FA chain. They are highly essential for maintaining the membrane fluidity and are present in all tissues, but are rich particularly in retina, brain, and spermatozoa. There are three important physiological omega-3 FAs available, including alpha-linolenic acid (ALA), eicosapentaenoic acid (EPA), and docosahexaenoic acid (DHA). Dietary omega-3 FAs are the precursors for the FA components of the neuronal membrane and are essential for maintaining the structural balance of cell membranes, signaling, neurotransmission, and modulation of enzymatic activity [8].
A growing body of preclinical data has shown that nutritional intervention, such as dietary supplementation with omega-3 (also known as n-3) FAs, may be of therapeutic benefit in acute injury to the brain [9-12]. Omega-3 FAs have long been known to play a restorative role in several pathways implicated in traumatic insult to the brain [11,13-16]. Emerging clinical evidence from both animal models and human studies of other brain injuries continue to suggest that they may provide benefits [16-18].
The most important n-3 FAs for human health and nutrition are docosahexaenoic acid (DHA), eicosapentaenoic acid (EPA), and alpha-linolenic acid (ALA). Omega-3 FAs must be obtained from diet, and are highly enriched in algal oil, krill, and cold water fish [19-21]. Poultry and eggs also provide small quantities of EPA and DHA, [22] while nuts, soybean, canola, and flax seed oils are major dietary sources of ALA [23]. Humans can also convert a limited amount of ALA into EPA and DHA, but a synthesis of EPA and especially DHA from ALA isinsufficient to supplant dietary intake [24].
The human brain consists of 60% lipid by dry weight, and docosahexaenoic acid is one of the most abundant fatty acids found in the solid matter of the brain [25]. DHA is aprimary structural component of the mammalian cerebral cortex and comprises 50% of neuronal membrane phospholipids [26]. Omega-3 FAs are essential for maintaining membrane fluidity [27], which in turn impacts neuronal cell adhesion, axon guidance, synapse maintenance, dendritic formation, and the speed of neurotransmission [28-30] DHA, for instance, is the longest and most unsaturated fatty acid found in biological membranes, with a structure that is tremendously flexible and therefore versatile [31]. It is capable of undergoing rapid interconversions between multiple torsional states and is unique in its ability to significantly alter membrane order and fluidity, phase behavior, elastic compressibility, ion permeability, and fusion [32-39].
Omega-3 FAs are so essential to and enriched in the brain due to their unique transformation into neuroprotective metabolites, which are critical in the defense against oxidative stress, tissue inflammation, and maintenance of synaptic integrity [40-42]. For example, during tissue stress, both EPA and DHA are thought to be released from membrane phospholipids and converted into compounds called “resolvins,” which actively promote resolution of inflammatory processes, such as via down-regulation of NF-κB and clearance of neutrophils [43-45].
Chronic dietary deprivation of n-3 FAs in animals leads to (1) decreased mean cell body size in neurons of the hippocampus, hypothalamus, and parietal cortex; (2) reduced the complexity of dendritic arborizations on cortical neurons; and (3) significant deficits in spatial learning and memory [46-50]. In contrast, increased brain levels of DHA in adult mice enhances hippocampal neurogenesis as evidenced by an increased number of proliferating neurons, increased neurite outgrowth, and increased density of dendritic spines, all of which correlate with markedly improved performance in spatial learning tasks [51]. In addition to serving as building blocks for membrane synthesis and modulating gene expression during neurogenesis, n-3 FAs are also involved in regulating neurotransmitter receptor levels and activity [47,48]. Performance of memory tasks was improved by increase intake of n-3 FAs in rats [52]. Impaired attention and poor performance were reported in rodents subjected to chronic omega-3 FAs deficiency [53-56]. Through mechanisms that are still incompletely understood, dietary supplementation with omega-3 FAs has been shown to significantly decrease the production of reactive oxygen species (ROS) and improve cognitive function in vivo [57-58]. Polyunsaturated fatty acids in humans, particularly DHA, serve an essential role in nervous system development and are required for proper synaptogenesis, neural membrane synthesis, and the building of functionally critical circuits within the brain [59]. DHA deficiency is associated with aging and neurodegenerative conditions such as Alzheimer’s disease [59], while DHA adequate consumption has been shown to improve performance on visuospatial learning and memory tasks in patients with age-related cognitive decline [60]. There is additional evidence in humans that dietary supplementation with omega-3 FAs improves functional recovery in subarachnoid hemorrhage and stroke [61-64]. DHA also has antioxidant activity and mitigates peroxidative damage of lipids and proteins in the brain [23], in addition to that DHA can attenuate neuronal death and cognitive and locomotor impairments in animal models of ischemiareperfusion injury to the brain [65-67], so it can be reasonably hypothesized that accumulation of omega-3 FAs in the brain might also be neuroprotective in TBI. The aim of this study is to investigate the adequacy of omega -3 FAs intake in post-traumatic brain injury patients.
2. Methodology
The ethics committee of our institution approved this study andpatients’ written informed consent was obtained (MERC/11/03). This study was conducted in an outpatient neurosurgery clinic at Khoula Hospital (National Trauma Center)–Muscat–Sultanate of Oman. 71 TBI adultpatients, aged 18-65 years, males and females participated in this study. Patients were invited to participate in an anonymous survey. This invitation was extended during routine outpatient visits. The exclusion criterion included: pre-injury psychiatric orneurological history other than those resulting from a TBI, non-Omanipatients and those who were known to have cognitive impairments that would preclude completion of the protracted assessment.
3. Demographic and Anthropometric Measurements
Demographic information, including age, sex, and education level, marital and smoking status were collected using a structured questionnaire. Weight was measured in kilogram to the nearest 0.1 kg using a digital weighing scale (Seca 208, Vogal and Halke, Germany). Height was measured to the nearest 0.5 cm by using a stadiometer protocol adapted from Lohman et al. [68] with a vertical measuring scale fixed to a metal bar connected to weighing scale.
Body Weight (BW) change was calculated as: (current BW in kilograms - ideal BW in kilograms)/ideal BW × 100. For patients who were unable to stand, height was estimated by using knee height equation as “height =85.10+1.73 x knee height-0.11 x age” for males, “height =91.45+1.53 x knee height-0.16 x age” for females [46], and by ulna length for males, height (cm)=4.605U+1.308A+28.003, and for females, height (cm)=4.459U+1.315A+31.485 [47], and by demispan for Males: height (cm)= (1.40 × demi-span in cm)+57.8 and for Females: height (cm) = (1.35 × demi-span in cm)+60.0 [48]. The mean height of the three measurements was considered incalculations. Body Mass Index (BMI) was calculated as wt. (kg)/ ht. (m2), and the cutoff points of the World health organization were used [69]. Glasgow Coma Scale is a neurological scale which aims to give a reliable and objective way of recording the conscious state of a person for initial as well as subsequent assessment. GCS is, a valid, reliable, and highly objective instrument used all over the world in multi clinical settings, conditions, especially in the emergencies' situations. GCS is considered the gold standard instrument for health care providers, including nurses to assess the level of consciousness [81].
Traumatic brain injury was classified into three categories based on Glasgow Coma Scale (GCS): mild if GCS scores ≥ 13, moderate If GCS between (9-12), and severe head injury if GCS score ≤ 8 [82].
4. Food Intake
Omega -3 FAs intake was assessed from daily food intake only (no supplementation) by using the 24- hour recall method [70]. Through face-to-face interview with each subject. Household utensils with the different portion size of common foods were used to assist the patients to report the accurate amount of food consumed. Omega -3 adequacies were assessed by comparing the actual intake with the recommended daily allowance (RDA) [71]. After analysis of daily food intake using electronic program (super - tracker) [72]. No Estimated Average Requirements (EARs) have been established. An Adequate Intake (AI) for alpha-linolenic acid, based on the average daily intake by apparently healthy people that are therefore assumed to be adequate, has been set at 1.6 g/day for adult men and 1.1 g/day for adult women [73]. Any intake of EPA and DHA, which normally accounts for about 10 percent of total n-3 FAs in the diet, is considered to contribute to the AI for ALA. The most effective way to increase body stores of EPA and DHA is through the increased dietary intake of oil from cold-water fishspecies and from krill.
5. Statistical Analysis
Graph Pad Prism (version 6.0) was used for statistical analysis. Means and standard deviations (using t-tests for two means, one way Anova was used to compare between groups), two sided statistical significance was set at α≤0.05 and proportions were compared by using chi-square test.
6. Result
71 patients in the age group 18-65, with a mean age of 27.3 years that fulfilled the eligibility criteria were enrolled in the study. The majority of patients were males (85.9%) and (14.1%) were females, with 6.1:1 male to female ratio. Most of the patients (75%) were aged between 18-30. 46.5% of subjects were classified as mild TBI while 12.7% and 40.8% were classified as moderate and severe TBI respectively using the Glasgow Coma Scale. Motor vehicle accidents were the most common cause of TBI (91.7%), followed by falls from height (8.3%) , (28.1%) of patients were underweight BMI <18.5 kg/m² while (16.9%) and (7.1%) were overweight and obese respectively table 1.
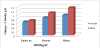
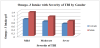
The Average intake of omega-3FAs in both males (1.1±0.3654 gm/d) and females (0.65±0.826 gm/d) was significantly inadequate compared with the RDA (1.6 gm/d and 1.1 gm/d) among males and females respectively P < 0.05 figure 1. Omega -3FAs deficiency rates were higher among females (40.9%) than in males (31.2%) TBI patients. This deficiency was positively correlated with body mass index (BMI) in both genders figure 2. The severity of Traumatic brain injury as measured by GCS has a negative effect on the intake of omega -3FAs, the intake was decreased from (1.35 gm/d) among mild TBI to (0.85 gm/d) among severe TBI male patients, While the intake was reduced from (0.95 gm/d) among mild to (0.69 gm/d) among severe TBI female patients figure 3.
7. Discussion
Omega-3 FAs are polyunsaturated fats found in both plants and fish play varied role in the CNS, providing a substrate for neuronal membrane phospholipids, modulating neuropterans- mission, and protecting cells from oxidative stress and inflammation through metabolites [74]. These acids have been subject of interest in the field of TBI for several years, particularly with regard to their use as a prophylactic treatment. Multiple recent reviews have emphasized the potential for these in TBI [75,76]. DHA deficiency is associated with aging and neurodegenerative conditions such as Alzheimer’s disease, [59] while DHA consumption has been shown to improve performance on visuospatial learning and memory tasks in patients with age-related cognitive decline [77]. DHA also has antioxidant activity and mitigates the peroxidative damage of lipids and proteins in the brain [23]. Given that the same inflammatory, apoptotic, and oxidative stress mechanisms are implicated in traumatic injury to the brain, it can be reasonably hypothesized that accumulation of omega-3 FAs in the brain might also be neuroprotective in TBI.
The overall intake of omega-3 FAs in the diet of our study (0.85 g/ day) is lower than in most of the Western countries. For example, the average intake of omega-3 FAs was 1.2 g/day in the United States [78].
Inadequacy intake of omega -3 FAs may be due to several reasons such as low food intake because of loss of appetite, a decrease in sensation, and loss of motor control post-TBI. In addition to these cases, it may be due to lack of omega-3FAs content in their diet as a result of knowledge deficit about the importance of such nutrients for TBI patient among the caregiver individuals and family members. Our study finds that there is a positive association between the severity of TBI, body mass index and omega -3FAs intakes, this association may be related to the worse complications post TBI including psychological, behavioral, biochemical, metabolic and food intake. These findings are supported of other studies findings of the role of omega-3 FAs to enhancing the neuronal repair process after TBI [79].
Recent evidence, however, strongly indicates that nutritional intervention may provide a unique opportunity to enhance the neuronal repair process after TBI. To date, two omega-3 FAs, docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA) have the most promising laboratory evidence for their neuro-restorative capacities in TBI. Although both animal models and human studies of brain injuries suggest they may provide benefits. [79]. The America Society for Parenteral and Enteral Nutrition and the Society of Critical Care Medicine, state that immune-enhancing enteral formulations with n-3FAs should be used in critically ill surgical patients (including trauma) [80].
8. Conclusion
Traumatic brain injury patients are at the severe deficiency of omega -3FAs intake through their daily dietary intake. The role of omega -3FAs in the neuronal growth and maintenance is well documented. Its intake could lessen the secondary effects of the trauma in the brain. The beneficial effects of n-3 FAs insist the clinical dietitians and neurologists work for the hand by hand to prescribe, supply, monitor and assess the dietary intake of such nutrients as well as the importance of considering their supplementation as a therapeutic option for TBI survivors. Further studies are warranted to determine the adequacy of omega- 3FAs and the effective dose for positive effects against TBI.
Competing Interests
The authors declare that they have no competing interests.