1. Introduction
Several patients hospitalized in convalescent rehabilitation ward are elderly patients with cerebrovascular disease. Appropriate nutrition management is required as an intervention for these patients with underlying malnutrition or a fasting state following the cerebral infarction. There can be cases among these patients in which oral intake is impossible for various reasons, including dysphagia, anorexia, the inability to intake food because of cognitive disability caused by the disorder [1].This can result in malnutrition or the onset of various diseases such as infections or bedsores if the elderly patients are not able to intake essential nourishment. This may greatly influence a patient’s life prognosis.
Life prognosis is significantly poor for patients with no oral intake. In a study of elderly stroke patients, patients with no oral intake had a 43.9% 3-yearsurvival; however, patients with oral intake had a 71.9% 3-year survival [1].Therefore, whether a patient can resume oral intake is an important concern not only for medical staff but also for the patients themselves and their families [2].Immediately and safely resuming oral intake can be expected to decrease the hospitalization period, and it increases the likelihood of discharge home without moving to another hospital. Therefore, appropriate training and nutritional means are necessary [3],and in a convalescent rehabilitation ward, appropriate judgment regarding oral intake is of great importance in conjunction with the evaluation of limb movement and cognition disorders.
Although there is no oral intake at admission, several patients can resume oral intake during hospitalization in a convalescent rehabilitation ward. Past reports have presented prediction formulae for oral intake or case reports regarding patients who resumed oral intake [4-8]. However, there has not been a complete analysis of factors, such as laboratory results or oral medication, associated with whether individual patients continued with tube feeding. In this study, we retrospectively assessed patients with cerebrovascular disease in a convalescent rehabilitation ward from admission to discharge to investigate the clinical factors associated with continued tube feeding, to compare patients who resumed oral intake with those who continued tube feeding.
2. Materials and Methods
2.1 Selection of subjects
For this retrospective study, we defined two groups of patients. The switching group included patients with cerebrovascular disease who were able to switch from tube feeding to oral intake by the time of discharge and who then required no auxiliary nutrition such as tube feeding or intravenous drip. The continuation group included patients with cerebrovascular disease who continued tube feeding or parenteral nutrition, at least partially.
Figure 1 shows a flow chart of the selection of subjects. A total of 2701 patients were discharged from Tsurumaki-Onsen Hospital between January 2011 and November 2013. Of these, 1642 did not present with cerebrovascular disease and data were missing for a further 783. We also excluded 237 patients with oral intake at admission, and five patients who had been hospitalized for long periods in other facilities. We finally selected the remaining 64 patients for this study, 17 in the switching group and 47 in the continuation group.
2.2 Investigation item
We obtained the following items from the patients’ medical records. Background data included sex, age, body weight (BW), the change in BW (ΔBW), hospital days, days from onset to hospitalization, primary disease (e.g.,Cerebral hemorrhage, Cerebral infarction, or Subarachnoid hemorrhage), complications (e.g., Parkinson's disease, diabetes mellitus, or epilepsy), the number of oral medicines, drugs that can cause malnutrition [9](e.g., antibiotics, digitalis preparation, psychotropic drugs, anti-anxiety drug, anticoagulant drug, proton pump inhibitors, or H2-blockers). Laboratory data included aspartate aminotransferase (AST), alanine aminotransferase (ALT), serum creatinine (Scr), estimated glomerular filtration rate (eGFR), C-reactive protein (CRP), the change in CRP (ΔCRP), white blood cell count (WBC), albumin (Alb), the change in Alb (ΔAlb), total cholesterol (TC), Functional Independence Measure (FIM) score(including the total (T), motor (M), and cognition (C)items), and FIM gain score. To establish the changes in BW, FIM, and laboratory data we compared the patients’ admission and discharge data.
FIM is a scale for assessing disability in terms of 5items associated with cognition and 13 items associated with motor function in daily life, with each item scored from 1(requiring maximum assistance) to 7 (full independence). Thus, the highest total score is 126and the lowest is 18, with higher scores indicating greater autonomy [10].
The rehabilitation team was composed of a physician, experienced nurses, and the rehabilitation staff (physiotherapist, occupational therapist, and speech-language-hearing therapist) in charge of the convalescent rehabilitation ward. They discussed and evaluated the patients’ FIM as a team. We calculated FIM gain score (FIM score on discharge minus FIM score on admission).
3. Statistical Analysis
We compared the background data and laboratory data between patients in the switching group and those in the continuation group. The results are presented as mean ± standard deviation (S.D.). We tested data to be compared for normality and used the Student’s t-test when a normal distribution was confirmed, or the Mann–Whitney U test if not. We used the χ2 test or Fisher’s exact test to compare categorical data. We used Spearman’s rank-correlation coefficient to investigate the correlation between FIM-T gain and Alb.
Furthermore, we adjusted for confounders and performed multiple logistic regression analysis with continuation or non-continuation of tube feeding as the outcome variable to investigate how this associated with the patients’ background data and laboratory data. We selected the significant factors ΔBW and ΔCRP as independent variables on the basis of the results of univariate analysis. In addition, we compulsorily incorporated the configuration factors “Number of days from onset to hospitalization” and “FIM-C Score” into the regression equation. When we performed multiple logistic regression analysis, we confirmed that there was no multicollinearity between the factors using Spearman’s rank correlation coefficient. Furthermore, we used paired t-tests or Wilcoxon’s signed rank tests to compare the results obtained on admission and discharge for each group.
The significance level was considered to be 5% (p<0.05). Statistical analysis was performed using JMP® (Version 10, SAS Institute Inc., Cary, NC, USA).
4. Ethics Regulation
This study was conducted with the approval of the Tsurumaki- Onsen Hospital ethics committee (Approval number: 135). This was a retrospective study using medical records, which complied with the Declaration of Helsinki and the “Ethical Guidelines for Clinical Research.”
5. Results
5.1 Patients’ background data
Table 1 presents a comparison of the patients’ background data between the switching group (male, 11; female, 6) and the continuation group (male, 29; female, 18). ΔBW was significantly greater in the continuation group (−3.8±4.0 kg vs. −1.5±2.0 kg, p = 0.0367). However, there were no significant differences between the groups with regard to sex, age, BW, hospital days, number of days from onset to hospitalization, type of stroke, number of oral medicines, complications, or drugs that can cause malnutrition.
5.2 Comparisons of laboratory data and FIM scores
Table 2 presents a comparison of the laboratory data and FIM scores between the switching and continuation groups. ΔCRP was significantly improved in the switching group compared with the continuation group (−2.2±4.3 mg/dL vs. 2.2±6.9 mg/dL, p = 0.028). Similarly, the improvements in FIM gain scores were significantly higher in the switching group compared with the continuation group (FIM-T: 26.7±25.7 vs. 5.3±10.1, p = 0.0001; FIM-M: 21.7±19.8 vs. 4.4±9.5, p<0.0001; FIM-C: 8.4±8.3 vs. 0.8±2.3, p<0.0001). However, there were no significant differences inAST, ALT, Scr, eGFR, CRP, WBC, Alb, ΔAlb, TC, and the FIM scores themselves (FIM-T, FIM-M, and FIM-C).
5.3 Comparison of body weight and clinical laboratory data at admission and discharge
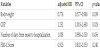
We compared BW, FIM scores, and laboratory data at admission and discharge within each group (Table 3). In the switching group, BW, AST, CRP, and WBC were significantly lower at discharge kg at admission, p = 0.0146; AST: 17.8±5.1 IU/L vs. 27.6±11.5 IU/L, p = 0.0033; CRP: 1.1±1.6 mg/dL vs. 3.4±4.3 mg/dL, p = 0.0493; WBC: 5076±1568 /μL vs. 7729±2908 /μL, p = 0.0004). The FIM scores were significantly higher at discharge compared with admission (FIM-T: 52.3±32.4 at dischargevs. 25.6±10.2 at admission, p<0.0001; FIM-M: score 39.6±25.3 vs. 17.9±10.9, p<0.0001; FIM-C: 18.9±12.7 vs. 10.5±6.0, p = 0.0002).There were no significant differences in ALT, Scr, eGFR, Alb, and TC.
In the continuation group, BW was significantly reduced at discharge compared with admission (45.8±10.0 kg at discharge vs. 49.1±10.6 kg at admission, p<0.0001). CRP was significantly increased at discharge (4.2±7.5 mg/dL vs. 1.7±1.9 mg/dL, p = 0.015). FIM scores significantly increased at discharge compared with admission (FIM-T: 29.0±18.9 vs. 24.5±14.3, p<0.0001; FIM-M: 20.4±14.9 vs. 14.7±7.2, p = 0.0001; FIM-C: 9.9±6.3 vs. 8.4±5.4, p = 0.026). There were no significant differences in ALT, AST, Scr, eGFR, WBC, Alb, and TC.
5.4 Multiple logistic regression analysis
We analyzedthe data for all 64 patients using multiple logistic regression analysis including various factors potentially associated with the continuation or non-continuation of tube feeding. Significant differences were observed forΔCRP and ΔBW (Table 4).
6. Discussion
Approximately 30–60% of patients with acute stroke suffers from dysphagia, although it has been reported that several of these patients improve for a few weeks [11-13]. However, even if there is no oral intake at admission, several patients will switch to oral intake during hospitalization in a convalescent rehabilitation ward. We therefore examined the clinical factors that may be associated with continued tube feeding by comparing patients with cerebrovascular disease who were able to switch to oral intake with the patients who continued tube feeding.
The most important finding of this study is that the continuation of tube feeding in patients with cerebrovascular disease is associated with ΔCRP and ΔBW, i.e., the changes in C-reactive protein level and BW between admission and discharge. This suggests that it is important to evaluate the onset of potential inflammatory diseases during hospitalization and control BW.
The results suggest that ΔCRP was the most relevant factor for the continuation of tube feeding. CRP significantly decreased between admission and discharge in the switching group, but significantly increased in the continuation group. Similarly, WBC also significantly decreased in the switching group but significantly increased in the continuation group. Romeo et al. reported that malnutrition or reduced levels of activity lead to reduced immunity and, in turn, to an increase in aspiration pneumonia [14]. It has also been reported that tube feeding itself is a risk factor for pneumonia in patients with acute cerebral vascular disease [15]. There is therefore a possibility that the onset of certain inflammatory diseases, such as aspiration pneumonia, during hospitalization may be associated with the continuation group in this study. The effects of oral care or swallowing rehabilitation as a preventive intervention for aspiration pneumonia have been reported [15-17]. In addition, increased activity and nutritional management have been reported as reducing compromise to the immune system [18]. Thus, we consider that it is possible to prevent aspiration pneumonia more effectively by a combination of weight loss and addressing infection through oral care and swallowing rehabilitation.
In this study, the change in BW was associated with factors for the continuation of tube feeding. We compared BW at admission and discharge; it was significantly reduced in both groups, but the reduction in the switching group was greater than that in the continuation group. The reason may be as follows. First, cerebrovascular disease is often accompanied by dysphagia; therefore, the energy deficiency associated with dysphagia may have been a factor. Second, the weight loss was likely to be associated with the invasiveness of underlying illness during hospitalization or the energy deficiency associated with it as the CRP level in the continuation group was high. Third, the rehabilitation load is increased in the convalescent rehabilitation ward. Some patients in convalescent rehabilitation wards participate in functional exercise such as resistance training and enduranceenhancing training for 2–3 h a day under circumstances of malnutrition or inappropriate nutritional management. Consumption of energy due to an increased level of rehabilitation load may then exceed energy intake. Therefore, it has been reported that malnutrition, loss of weight, and a reduction of muscular endurance become advanced, similar to catabolism. Furthermore, there is a possibility of a considerable reduction in BW. Once BW is reduced in elderly patients, they become malnourished because they cannot eat sufficient food to regain the lost BW. Being underweight and malnutrition at discharge are risk factors for readmission; [19] this is a concern because ΔBW was associated with the continuation of tube feeding in this study. We therefore investigated the association between nutritional status and activities of daily living (ADLs) and observed a significant positive correlation between FIM-T gain and Alb. This result supports the report of Usui et al. [20]., who suggested that there is a possibility of improving ADLs if the nutritional status is improved. We therefore consider it necessary to address not only ADLs but also rehabilitation and weight gain-based effective nutritional management with a view to life after discharge.
It has also been reported that drugs have been involved in malnutrition in the elderly [19]. Therefore, we investigated in this study drugs that have been reported to be associated with malnutrition, but we found no significant differences between the switching and continuation groups. However, several elderly people take a lot of types of medication to treat a range of chronic diseases. Side effects increase due to drug interactions when taking six or more types of oral medicine [18].It is necessary to give in-depth consideration to the association between oral drugs and malnutrition due to the possible effects on the ADLs of the elderly.
The present study had three limitations. First, it was a single-center cross-sectional study with only a small number of patients undergoing analysis. Second, this study did not consider other possible factors that may be associated with the incidence rate of pneumonia, such as the repetitive saliva swallowing test, the assessment of swallowing function by speech-language-hearing therapy, or information about hygiene of the oral cavity. Third, there were missing data items because this was a retrospective observational study. These limitations may potentially have influenced the results of this study and ideally the results should be confirmed by a prospective cohort study.
7. Conclusion
We showed in this study that continuation of tube feeding in patients with cerebrovascular disease was associated with the changesin BW and CRP between admission and discharge.To maintain and improve physical function, cognitive function, and ADL, we should therefore try to ensure improvement of weight loss and assessment of the onset of inflammatory disease. We believe that a comprehensive approach to oral intake needs to be taken to address these issues.
Competing Interests
The authors declare that they have no competing interests.
Author Contributions
Eiji Kose: conception and design; doing the field work and data
collection; data analysis and interpretation; preparation of draft
manuscript and doing revisions; overall scientific management.
Manabu Toyoshima: doing the data collection.
Hiroyuki Hayashi: giving scholarly input in field work; providing
critique; overall scientific management.
Acknowledgments
The data for subjects were obtained from medical record in Tsurumaki Onsen Hospital.