1. Introduction
Nordic Pole Walking (NPW) is a popular recreational sport [1-4]. It incorporates two poles made of aluminum, or graphite and/or carbon fiber. These poles should be adjusted in length to be at the level of the navel or elbow. The two poles are gripped with the left and right hands and directed backward at an angle of about 30-40 degrees. They are pushed backwards as one walks, while swinging the arms. The arms swing like a pendulum as if one is reaching out to shake someone's hand. When one pushes downward on the poles this action thrusts the person upward and forward during walking, forcing the person to both straighten up (improving the posture) and speed up, because one uses a longer step and a faster gait with NPW than with normal walking.
NPW requires the use of the upper body including the muscles of the arms, shoulders, neck, chest, abdomen and entire back for pushing the poles backward, as opposed to ordinary walking that uses only the lower limbs. The result is a strengthening of these upper body muscles. This helps to straighten the spine, thus improving posture, which helps alleviate physical pain and stiffness. In addition, since the individual is required to push down on the poles, the upper body supports part of the body weight so that the spine, hips and legs are exposed to a much lower weight and therefore to much lower physical stress, which also helps relieve the pain [1-4]. NPW use as a form of therapy for back, hip, and knee pain from various causes has received only scant attention in the literature [1-4]. Indeed recent summaries of treatment of low back pain including professional guidelines of therapy by various specialty groups have not mentioned it at all [5-7]. However what little information is known about NPW for these conditions suggests that it might be useful in the treatment of pain and function in the shoulder, neck, low back, hips, and knees [1-4,8-16].
We report here our experience with NPW on pain on walking and on the distance walked in a community-based prospective study of 100 people aged 60 and over who had a history of low back, hip and/ or knee pain while walking for 0.5 or more years (mean duration of pain 11.7 ± 13.2 years) and who were started on NPW and who were assessed for severity of pain and distance walked before NPW and 1, 6 and 12 weeks after initiating the study.
2. Methods
2.1 Participants
Participants included a total of 100 individuals comprised of; 52 females and 48 males, who were recruited when an article was published by one of us (DSS) in a non-profit local community magazine in Israel describing the health benefits of NPW, including its possible effects on reducing low back, hip and/or knee pain (see the article in Google – Nordic Walking and Donald Silverberg and ESRA). All 100 people suffered from pain on walking in the low back, hips and/or knees for at least 6 months. 54 suffered from chronic low back pain (LBP) from lumbar disc disease, 51 from chronic knee pain from osteoarthritis, and 32 from chronic hip pain due to osteoarthritis. In 61 only one area was involved (e.g. knees) while in 39 more than one area was involved.
2.2 Procedures
The instruction on how to perform NPW was done individually by a certified NPW instructor (AP) at their home and free of charge, and took about one hour. All those interested in trying NPW (the 100 cases reported here) then purchased the poles and began using them. In some cases a second free visit was needed if the person still felt uncertain about how to walk with the poles.
2.3 Measurement protocol
Before the onset of NPW, and 1, 6 and 12 weeks after starting to use them each person was interviewed by telephone (by DSS) as to how long they had had pain, what they were told were the diagnoses of the pain, and how far they estimated that they could walk. The severity of pain on walking was assessed by a Visual Analogue Scale (VAS). In this measurement the patient was asked to visualize a 10 cm line with the number 10 at one end representing very severe pain and the number zero at the other end representing no pain. The patient was asked to estimate the severity of their pain on walking using this scale before NPW was started and at the end of the first, sixth and 12th week of performing NPW. They were also asked if any health professional had ever in the past suggested using NPW for their pain. Finally they were asked at 12 weeks whether they were planning to continue to use NPW in the future. They were informed that their findings would be included in a research study and all agreed.
2.4 Statistical analysis
Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS). The Mean and Standard Deviation were calculated for all parameters. Pain and distance walked before and 1, 6 and 12 weeks after NPW was started were compared using paired-samples T-tests and repeated measures analysis. Statistical significance was a p value <0.05.
2.5 Informed consent and ethical guidelines
All participants provided informed consent before involvement in the study. The study was conducted according to the Declaration of Helsinki (DoH) ethical principles regarding human experimentation developed for the medical community by the World Medical Association (WMA).
3. Results
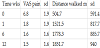
There were 52 females and 48 males. The mean age of the participants in the study was 75.4 ±7.7years (range 60-100). The pain on walking had been present for a mean of 11.7 ± 13.2 years (range 0.5-60 years) before starting NPW (Table 1, Figures 1 and Figure 2).
Nine people stopped using the poles within the first few weeks because they did not subjectively experience improvement in their level of pain while walking.
Over the 12 week period, in the 91 remaining participants, all 91 experienced a reduction in pain on walking (by the VAS scale) and an increase in distance walked compared to before using the poles. These participants continued using them for the entire 12 weeks and stated at this time that they would continue using the poles in the future.
The mean estimated walking distance (Table 1 and Figure 1) at baseline before NPW was 504.7±591.4 meters (m), was 1521.5±817.7 m after one week of NPW, 1778.3±885.7 m after 6 weeks and 1851.7±940.0 m after 12 weeks of NPW. The differences between estimated walking distances between 1, 6 and 12 weeks were all significantly different from baseline, p<0.001.
The mean VAS (Table 1 and Figure 2) at baseline was 6.8±1.9, 1.8±1.9 after 1 week, 1.6±1.6 after six weeks and 1.5±1.6 after 12 weeks. The differences in VAS scores between 1, 6 and 12 weeks were all significantly different from baseline, p<0.001.
During the study, in all the 91 participants who completed the 12 weeks of NPW, when the participants walked without the poles the pain and distance walked returned almost immediately to what it had been without the NPW.
In none of the cases had any physicians (including general practitioners, internists, orthopedic surgeons or chronic pain specialists), physiotherapists, or chiropractors ever recommended the use of NPW to them. They had all started using NPW because of the article they had read about it.
4. Discussion
NPW was associated with reduced low back, hip and/or knee pain on walking and increased estimated distance walked over a 12 week period. Ninety one percent of the participants used the poles regularly for the 3 month period while nine percent stopped them because of lack of improvement in the pain. The 91% that used them regularly had a marked reduction in pain on walking, the mean VAS scale falling rapidly and significantly within a week, and the VAS remaining at about this level for the whole 12 week period. In addition, the ninety one percent of the participants that continued to use them had a significantly marked increase in estimated distance walked, the average increase for the 91 participants being from 504.7± 591.4 meters (m) before NPW to 1851 ± 940.0 m after 12 weeks of NPW. This improvement started within the first week in most and was then maintained over the entire 12 weeks. This improvement occurred despite of the fact that they had had several years of chronic pain (mean duration 11.7±13.2 years).
Our results are similar to those found by others [1-4,8-19]. Relief of pain with NPW in the shoulder [8], neck [9], back [10-13], hips [14] and legs [15-19] (the latter occurring after trekking [15,16] or in people with intermittent claudication [17-19] has been reported. These studies, as well as our own, were done mostly with individuals from middle to old age, suggesting that this form of therapy may be suitable for a broad age range of people.
NPW has been demonstrated to cause an improvement in muscle strength in the upper arms, shoulders, neck, abdomen, chest, back, hips, knees and legs and to improve posture, flexibility, balance, endurance and gait parameters, including an increase in the length of each step and the number of steps taken per minute and therefore the walking speed [1-4]. The improvement in back, hip and knee pain seen by us and others [1-4,8-14] is, as mentioned earlier, partly because NPW reduces the impact of walking on the back, hips, knees and ankles, since the two poles and upper body carry part of the body weight and therefore there is less impact on these lower areas. In addition, the use of the poles requires the use of muscles of the arms, shoulders, neck, chest, abdomen and back which causes the strengthening of these muscles and the stabilization and straightening of the spine, thus improving posture and also reducing muscle spasms, thus alleviating the pain in all the areas [1-4].
Our results are very similar to those of Park et al. [13]. They performed NPW in 16 elderly women with chronic low back pain, evaluating its' severity by a VAS scale 6 and 12 weeks after starting NPW. Their VAS results for pain were very similar to ours with a steady reduction in back pain throughout the entire period , the VAS score falling from 5.67 at onset to 2.93 at 6 weeks and 0.77 at the end of the study at 12 weeks (10 being very severe pain and zero being no pain.
In another study of 151 patients with chronic low back pain of moderate to severe severity [10] the authors found no statistically significant differences between 8 weeks of a) supervised NPW, b) unsupervised NPW and c) advice to remain active. However the greatest average improvement tended to favor the supervised NPW group and people in this supervised group tended to use less pain medication and to seek less care for their back pain.
A recent randomized controlled study of 152 patients with osteoarthritis of the hip compared individuals using NPW as opposed to either strength training or unsupervised home-based exercise (HBE) over a period of 2, 4 and 12 months [8], NPW was found to be superior to either of these type of exercises in terms of functional performance, vigorous physical activity and mental health. NPW was also superior to the other modalities in distance walked. In addition, by two different pain scales, NPW was superior to unsupervised HBE.
Nordic Pole Walking (NPW) has also been used successfully as a mode of therapy in individuals suffering from illnesses such as Parkinsonism, to avoid falls in people with that tendency, chronic obstructive pulmonary disease (COPD), heart failure, peripheral vascular disease (intermittent claudication), Sjogren's Syndrome, rehabilitation after acute coronary syndrome, fibromyalgia, pain and stiffness in the shoulder after breast cancer surgery, obesity, diabetes, hyperlipidemia, hypertension, sports injuries, bone and joint injuries, and depression [1-4].
In NPW, the total body energy expenditure is increased by approximately 45 percent more when compared with normal walking, since normal walking requires the use of only about fifty percent of the body's muscles whereas NPW requires the use of the upper body as well as the lower body [1-4], so that a total of over ninety percentof all the body's muscles are utilized [1-4]. Thus NPW increases peak oxygen utilization, peak heart rate, endurance and caloric expenditure more than ordinary walking and can thus help decrease obesity, total fat mass, low density lipoproteins, triglycerides and HbA1C and increase high density lipoproteins [1-4].
Despite this greater energy expenditure due to the extra exertion in NPW, the individual, surprisingly, usually does not experience any additional feelings of increased exertion [1-4].5. Study Limitations
Major limitations of this prospective study are that it was both short and uncontrolled and only conducted by telephone interviews. Further studies should be prospective, controlled, and long-term, including a careful personal history and physical examination of the individuals participating in the study. Insofar as details of the pain experienced while walking and the distance walked, the patients were asked to estimate how far they could walk, while the causes of their pain and its' severity by VAS scale, were largely subjective. No precise measurement was performed of distance walked as for example by using a pedometer or by counting the number of steps walked. In future studies a more comprehensive medical history should be attained from pre-existing medical records and a physical examination should be given by a qualified clinician. In addition, a more accurate and standardized method of measurement of actual distance walked should be used as well.
Despite these limitations, the preliminary results are noteworthy considering that the majority reported marked, rapid and persistent reduction in pain from NPW and a statistically significant increased walking distance despite often suffering from many years of chronic pain and limitation of distance walked despite having received a broad range of pain treatments and alternative therapies for their pain and limited walking distance. Ninety one percent of the participants improved rapidly and maintained this improvement in both the pain parameters and overall distance walked over the twelve weeks of NPW, and only nine percent ceased participation in the initial stages of the study due to the lack of subjectively perceived beneficial effects on pain on walking.
Considering that only a handful of studies have investigated the effects of NPW on the low back, hips and knees and the significant and promising results of our pilot study, further research of this topic by other researchers utilizing more comprehensive longterm controlled studies could possibly confirm the importance of NPW as a practical and beneficial form of rehabilitation. This is especially relevant considering the rapidly growing elderly population throughout the world, the considerably low cost of the Nordic poles (ranging from $70-$130) and the ease and the simplicity of learning and implementing NPW (it can usually be learned from an instructor within a few minutes). If further studies confirm our findings of NPW 's utility, it is conceivable that NPW might become a widespread and commonly used form of therapy for lower back, hip and knee pain, all of which are so prevalent in society and often so resistant to various forms of other existing forms of therapy for the alleviation of chronic suffering of pain experienced by elderly populations[6,7,20-22]. It is widely known that lower back pain, compared to no low back pain causes overall lower health status, greater absenteeism, greater work impairment, larger direct and indirect costs, impairment of activity, depression, increased physician visits, and increased emergency room visits and hospitalizations [1-4,6,7,9,20-22]. Yet none of the individuals in our study had ever received a recommendation to try NPW from their physicians, physiotherapists or chiropractors. In addition, published orthopedic and other medical guidelines for diagnosis and treatment of low back pain do not mention NPW as a possible therapy at all [6,7]. Similarly recent studies of treatment of back pain by physiotherapists in America [23] and Sweden [24] also failed to mention NPW as a treatment modality for back pain.
6. Conclusions
NPW holds promise in the effective treatment of chronic back, hip and knee pain when walking, both in degree of pain relief and in distance walked, and is a relatively simple exercise to do which is easy to learn and perform and is safe, convenient, inexpensive, and can be a pleasant adjunct to the therapy for these conditions.
Competing Interests
The authors declare that they have no competing interests.
Acknowledgments
We wish to thank Dr. Tehilah Menes for statistical assistance.