1. Background
Shift work disturbs the natural circadian rhythms, and nurses suffer from an unfavorable condition known as shift lag and desynchrony [1]. Factors influencing fatigue of nurses have been studied extensively and work-related factors, psychological factors, and demographic factors have been recognized as contributing to nurse fatigue [2,3,4]. It is important for night shift workers not to perturb biological rhythms. Sleepiness and fatigue among shift workers are known as potential risks for occupational safety and health in many industries [5]. Taking a nap during the night shift has been suggested as an effective way to prevent fatigue or other complaints related to shift work [6]. Nursing is a profession that typically involves shift work as nurses are required to provide continuous health care for the patients [7].
Especially, female nurses having family has extra burden of home responsibilities and sleep changes strongly affects menstrual cycle [8,9]. Night shift with attention-demanding has been acknowledged as a serious risk factor for female nurse’s health [10]. Physical, emotional, and social stress are exposed by sleep disturbances in shift-work [7]. Female nurses are affected by environmental factors, including family commitments and work strain, which can cause difficulty falling sleep, frequent awaking, and premature awakening [11].
Recently, life style after night shift for recovering from work-induced fatigue has been brought to attention [12]. Exercise or social behavior with physical activity helps to recover from work-related fatigue and to decrease work-related complications. Active and fulfilling nonwork- time behaviors are more significant in maximizing recovery from work strain than is commonly recognized. High mental and emotional strain has been shown to recover better through active exercise, to levels over and above the simple rest afforded by being removed from the stressful work environment [13]. Regular exercise can lead to a healthy lifestyle, reduce stress, and reduce feelings of chronic fatigue [7].
However, there has been no comprehensive study for improving that tried to prove the interrelationship among occupational factors, life-related factors including family environment of nurses with night shift. We hypothesized that age, clinical experience years as nurse, and clinical experience years of night shift including the above-mentioned factors may associate with the accumulation of fatigue at night shift and the recovery from fatigue. Also, nurses with higher physical activity level after night shift (at holiday) may effectively recover from fatigue after night shift. Therefore, this study would contribute to improve fatigue at night shift in medical-surgical female nurses.
2. Materials and Method
2.1 Participants
97 Japanese medical-surgical female nurses were recruited from two regional private hospitals in Nagasaki prefecture, Japan. We divided the subjects into two groups; recovery group and non-recovery group based on improvements in fatigue feelings (total points of drowsiness, instability, uneasiness, dullness, and eyestrain) between pre night shift and post-holiday. Recovery group was defined by the minus point from post-holiday to pre night shift. If the value was zero, this subject was defined as recovery group.
2.2 Instruments
The demographics data (age, body mass index (BMI), clinical experience years as nurse, clinical experience years of night shift, and daily life styles) and occupational data (nap time length and steps during night shift) in medical-surgical female nurses were collected by questionnaire. Drowsiness, instability, uneasiness, dullness, and eyestrain as the subjective fatigue symptoms from pre night shift to post holiday were evaluated. These subjective fatigue symptoms were assessed by a questionnaire that asked about work-related feelings of fatigue Jikaku-sho sirabe, which was proposed by the Industrial Fatigue Research Committee of Japanese Occupational Health [14]. Physical activity levels (steps and energy expenditure (EE)) from pre night shift to post holiday were examined by three dimensions speed sensor. Physical activity levels were measured by Actimaker (EW4800, Panasonic, Japan).
2.3 Data collection
Data collection took place from April 2012 to February 2013. All nurses were recruited from two private hospitals in Nagasaki, Japan. The subjective symptoms were evaluated at four points; pre- and post-night shift, and pre- and post- holiday using JSL recommended questionnaire. Responses for each component range from 0 to 5, with higher scores signifying poorer condition [14]. Recovery occurs when an individual’s functioning returns to its pre-stressor level and when strain caused by the stressor is reduced [15]. Thus, the criteria of measurement point of fatigue in this study were from pre night shift to post holiday.
2.4 Ethical considerations
This project was reviewed and approved by the ethics committee of the University of Nagasaki. In addition, the purpose procedure of this study was explained to director of each hospital. Informed consent was obtained from all nurses.
2.5 Data analysis
Chi-square test and Mantel-Haenszel test for trend were conducted to examine the association between fatigue feelings and the demographics data. Differences of five fatigue symptoms at four measurement points between recovery group and non-recovery group were using Mann-Whitney test. The change of five subjective symptoms at four measurements points were confirmed by Friedman’s test. Logistic regression analysis was utilized to prove the factors of fatigue at night shift nurses. Models were adjusted for clinical experience years as nurse, BMI, breakfast consumption habit, smoking habit, daily physical exercise habit, living with family, nap time length, variations of drowsiness, instability, uneasiness, dullness, and eyestrain from pre night shift to post holiday. Goodness of fit test was confirmed by Hosmer-Lemeshow. The variance inflation factor (VIF) is used as an indicator of multicollinearity. Probability values less than 0.05 were considered indicative of statistical significance. All statistical analyses were performed using SPSS ver 19.0 software (SPSS Japan, Tokyo, Japan). All data were expressed as median based on Kolmogorov-Sminov test.
3. Results
3.1 Participant demographics
Among the 97 shift-working female nurses participants, 39.2% (n=38) were 20-29 years old, 34.0% (n=33) were 30-39 years old, 14.4% (n=14) were 40-49 years old,9.3% (n=9) were 50-59 years old, and 3.1% (n=3) were more than 60 years old. Median age was 31.6 years old (range: 21.6-61.3). Median clinical experience years as nurse was9.0 years. Mean clinical experience years of night shift was9.0 years. The majority (72.2 %, n=70) had family. 8.2% (n=8) has smoking habit and 19.6% (n=19) has regularly exercise habit more than two times per week. 66.0% (n=64) has breakfast consumption habit. All participant demographic data between recover group and non-recovery group were not significantly different using Chi-square test and Mantel-Haenszel test for trend (Table 1).
3.2 Physical activity data from pre-night shift to post-holiday
Table 1also shows physical activity data at the hospital and at home in recovery group and non-recovery group. In the total of 97 nurses, median BMI was 21.2 kg/m2. The range of BMI was from 17.1 to 32.9kg/m2. 9.3% (n=9) was BMI>25. In the total of 97 nurses, median total steps and EE were 14363steps and 1958 kcalat night shift. At holiday after night shift, median total steps and EE were 3467steps and 864 kcal. Total steps and EE were significantly different between at night shift and at holiday (P<0.001). Median nap time length during night shift was 75 minutes.
3.3 The variations of five subjective symptoms from pre night shift to post-holiday
Drowsiness, instability, uneasiness, dullness, and eyestrain from pre night shift to post night shift were not significantly different between recovery group and non-recovery group excluding eyestrain at postnight shift. Five subjective symptoms from pre-holiday to postholiday in non-recovery group were statistically higher than those in non-recovery group (P<0.05) (Table 2). Five subjective symptoms were significantly different at four measurement points in both groups (P<0.001).
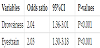
3.4 Odds ratio for fatigue factors in Japanese night shift female nurses
Factors that influence the recovery from night shift fatigue in Japanese female nurses were clarified by logistic regression analysis. Logistic regression models using step-wise were used to adjust for clinical experience years of night shift, BMI, breakfast consumption, smoking habit, daily physical exercise habit, living with family, nap time length, total steps at night shift, total steps at holiday, the variation of drowsiness, instability, uneasiness, dullness, and eyestrain from pre-night shift to post holiday. The correlations among age, clinical experience years as nurse, and clinical experience years of night shift were quietly high (R>0.8); we thus cannot jointly analyze these variables at logistic regression models. Adjusted odds ratio (95% confidence interval) for fatigue in medical-surgical female night shift nurses were 2.04(1.36-3.01) in drowsiness and 2.03(1.30-3.18) in eyestrain (P<0.001) (Table 3).
4. Discussion
Work-related fatigue and recovery from fatigue are associated with age [16]. Fatigue from night shift can be effectively treated by aggressive life style as sports activity at day off [17]. Sports and related activities have positive effect on individual health and well-being [18]. However, people spend relatively little time on exercise and sport [19]. In this study, total steps and EE at holiday actually decreased compared to at night shift both recovery group and non-recovery group. Age, clinical experience years as nurse, and clinical experience years of night shift were not different between recovery group and non-recovery group. Also, physical activity level between two groups also did not differ. We suggested that these results have been shown to function as psychological detachment. Psychological detachment from work environment is recognized as important factor that helps to recover from job-stressors [20]. Our data clearly showed that drowsiness, instability, uneasiness, dullness, and eyestrain at post night shift were quietly high; however, these five subjective symptoms stupidly decreased at post night shift in both groups. These changes of subjective symptoms may reflect psychological relief from high work demands and high work stress at night shift. The exposure to workplace related stressors is a predictor of cardiovascular diseases and higher systolic blood pressure, and psychological detachment from work environment of nurse who engaged in night shift contributes to recover from subjective symptoms [21].
Our research indicated that drowsiness and eyestrain were significantly risk factor for fatigue at night shift in female nurses. Drowsiness was 2.04 folds higher risk for recovering from night time shift’s fatigue compared to recovery group. Eyestrain was 2.03 folds increased risk for recovering from fatigue at night shift. Recently, eyestrain has been brought to public attention. Eyestrain as well as sleep deprivation, especially in night shift nurses, is related to fatigue under the factors including mental-psychological state, occupational and social factors, and environmental factors [22].Preventing sleep deprivation among health care provider could be an extremely means of reducing medical errors and sleeping during night shift could be viewed as a strategy towards the reduction of errors [23]. Sleep deprivation, compounded by the circadian rhythms, is a profound health problem for nurse [21]. Fatigue is a critical problem for nurses that it leads to medication error, degradation in performance, personal health problem, job dissatisfaction, and frequent requests to quit from night shift [24]. Sleeping for 2-3 hours during night shifts is related to a better recovery from fatigue at night shift [25]. Taking a nap is an effective tool for improving working conditions during night shift [5].
In Japan, aging has been stupidly proceeding in the world. The burden, the quantity, and the quality of nursing care in Japanese nurses, especially medical-surgical female nurses, have been increasing. Untrained Japanese young nurses who are short clinical experience of night shift cannot avoid engaging in two-shift rotation system with nap. Nursing care and health services have to be offered on twentyfour hour basis. Nursing, with long work hours, is both physically and mentally demanding, which may lead to acute and fatigue [4]. Thus, we need to positively manage work environment formedicalsurgical female nurses. Work-related factors, such as job demands, job control, support at work including support from supervisor and co-workers, physical work environments, and shift work were confirmed to contribute to fatigue in nurses[26]. Fatigue and recovery problems from fatigue strongly associated with partnership among nurses[24].Younger nurses in particular, need more support than is currently recognized if they are to be retained within the profession [16]. Psychological contributors like mood disorders (anxiety and depression) and sleep quality were also found to predict fatigue [27]. An important point to emphasize is that nursing managers should not only take consideration of psychological fatigue such as dullness and eyestrain in relation to nap during night shift but also pay attention to recovery process considered psychological detachment form stressful work environment when designing program to decrease female nurses’fatigue at night shift.
5. Conclusions
Our results suggest that psychological detachment for medicalsurgical female nurses form work environment is recognized as important factor that helps to recover from subjective symptoms. Moreover, the fact that drowsiness and eyestrain are the risk factor for fatigue at night time suggests the important of nursing management at hospital. Taking a rest with a nap, job control, partnership among nurses, and support at work, especially in younger nurse and untrained nurse, is the key issue when discussing nursing management in night shift female nurses, preventing medical error, and protecting nurses’ health.
Competing Interests
The authors declare that they have no competing interests.
Author Contributions
Kazuo Minematsu, Tae Yamaguchi, Mitsuyo Nakashima, Noriaki Tsunawake, and Narumi Ooshige were responsible for the study conception and design, and made critical revisions to the paper for important intellectual content. Tae Yamaguchi performed the data collection. Kazuo Minematsu, Mitsuyo Nakashima, Noriaki Tsunawake, and Narumi Ooshige were responsible for the drafting of the manuscript and for providing statistical expertise. Narumi Ooshige obtained funding and supervised the study.
Acknowledgments
We would like to thank all the participants, staff, and investigators who volunteered and were not financially compensated for their contributions to this study.