1. Introduction
Students in health profession programs are traditionally educated in silos. Upon graduation, they are expected to function as part of a health care team, collaborating with others to care for patients from admission to discharge. It is hard to imagine a winning team composed of individuals with complementary and essential skills who have not practiced working together.
Communication problems among health care personnel have been implicated as a cause of most patient errors (American Association of Colleges of Nurses [1-4]. The Joint Commission [5,6] reported that communication breakdowns were the leading root cause of sentinel events between 1995 and 2006. To resolve this situation, the Joint Commission issued National Patient Safety Goals to improve the effectiveness of communication among caregivers and recommended creating a culture that encourages team training. The American Association for Critical Care Nurses [7] also recommends that team members have access to educational programs that develop critical communication skills.
According to the WHO [8], interprofessional education (IPE) involves teaching and training students how to learn about, from and with each other using interprofessional teams (Figure 1). IPE purportedly trains safe health care professionals who are ready to work in collaborative health care teams resulting in improved patient health outcomes [9]. Further, IPE is highly recommended by the American Speech-Language-Hearing Association [10] as well as the American Association of Colleges of Nursing. See figure 2 for additional benefits resulting from IPE [8].
Nurses and other disciplines are constantly faced with the challenge of handling providing care to patients with dysphagia. If not properly diagnosed, one major risk includes aspiration pneumonia which has an extensive impact on health with regard to morbidity, cost, and mortality [11-17]. Up to 15% -30% of pneumonia cases in hospitalized patients is due to aspiration [11-13]. According to the ICD-9 code based reviews, pneumonia is considered the second most common diagnosis in Medicare patients and is the leading cause of death in elderly patients [13]. Attempts to prevent aspiration may result in limiting patients’ oral intake, often resulting in malnutrition and dehydration. Therefore, it is crucial that we accurately detect and prevent aspiration especially of our highest risk groups, the growing geriatric population and those with neurologic injuries. Screening all hospitalized geriatric patients’ ability to swallow could help identify those at risk of aspiration. The 3-ounce water swallow screen challenge has been identified as a simple, quick and easy procedure that requires minimal training and can be done at the bedside by the nurse [16]. It is a non-invasive and reliable screening tool that allows for appropriate referral to speech-language pathology for further swallow evaluation and management.
Administering and interpreting the results of a swallow screen accurately is a critical skill for nursing students. Mastering this procedure will help to minimize the incidence of aspiration and enhance patient safety, and should be incorporated into the didactic and skills training that nursing students receive prior to providing patient care. This clinical competency will help nurses to identify patients who are at risk for aspiration, prevent the incidents of nonventilator associated pneumonias and decrease health care costs.
Currently, the inclusion of swallow screens in nursing instruction is being overlooked, as evidenced by a paucity in the literature and inconsistent discussions of the skill in nursing textbooks. Nurses are the first line of contact and responsible for coordinating the care of all acute patients. Clearly, nursing students should be taught how to properly perform a swallowing screening as an essential component of the curriculum. The literature supports the use of simulation as a co-curricular learning activity to promote the development of interprofessional communication and collaboration [18-21]. Therefore, interprofessional simulation integrating nursing and speech-language pathology students was chosen as the pedagogy of instruction for the nurse swallow screen.
The purpose of the study was to pilot the new IPE simulation training which focused on the identification and management of patients with swallowing difficulties and to assess the following learning outcomes: (a) Recognize the signs and symptoms of dysphagia and the importance of communication and teamwork in preventing aspiration, (b) Recall teamwork and communication strategies, (c) Recognize or restate team skills, (d) Put into practice those team skills that they have encountered during the course in a simulated clinical environment, and (e) Increase preparedness for working as part of a collaborative ready health workforce. The focus of this paper will report on the students’ self-reported learning experience to the piloted simulation scenario.
2. Methods
This is a mixed methods study that involved simulated teambased Interprofessional (STBIP) activities between pre-licensure nursing students in a baccalaureate and second year speechlanguage pathology graduate students at a four year state university in California. IRB approval was obtained, and purposeful sampling was used to recruit participants. All first semester nursing students (n=80) and third semester graduate SLP students (n=16) were eligible to participate, and invited via email to participate in the study. A total of 45 students volunteered to participate in the STBIPE study, including 16 SLP students (35%) and 29 nursing students (65%).
A simulation scenario using a two-phase unfolding case was created for nursing and SLP students. In Phase I, students from both disciplines received a case report and completed a chart review. The nursing students were instructed to perform a physical assessment and complete a nursing swallow screening. A retired educator who was a stroke survivor served as the standardized patient with aphasia, apraxia of speech, and left-sided hemiparesis. Phase I ended after the patient failed the swallow screen, and a debriefing session immediately followed. Phase II began with the nurses requesting an order for a swallowing evaluation. Once ordered, the SLP students administered a complete clinical bedside swallowing evaluation and determined the appropriate dysphagia diet for the patient. This clinical decision signaled the end of Phase II and a final debriefing session completed the scenario.
Quantitative data were collected using Likert scale surveys to evaluate student experiences at the end of the IPE simulation. Qualitative data were collected using reflective questions regarding student simulation experiences. The simulation debriefing sessions were recorded, transcribed and analyzed for emerging themes. The scenario was beta-tested twice, revised, and later published on the California Simulation Alliance site [22].
3. Results
Analysis included descriptive statistics for demographic data, and Spearman’s rho nonparametric correlation was used with both instruments. Cronbach’s alpha reliability coefficient for the instruments employed will also be presented. All analysis used the Statistical Package for the Social Sciences (SPSS) version 22.0.
Qualitative data including the participants’ comments regarding their IPE experience were recorded during the simulation debriefing session.
3.1 Participants Demographics
Data indicated that the majority of the participants were female (80%). The participants’ ages ranged from 20-55 years, with a mean age of 28 years. The majority of participants reported English as their primary language (80%), and 50% of the participants reported speaking other languages at home. Figure 3 represents data related to ethnic distribution of IPE participants.
3.2 Statistical analysis
To evaluate student satisfaction with the simulated IPE experience and student self-confidence with implementing the learned clinical skills. To that end, the participants completed two Likert-scale instruments including the Simulation Design Scale (SD) and the Student Satisfaction and Self Confidence in Learning (SSSC) instrument. The internal consistency of both instruments was determined using Cronbach’s alpha with the following results: SD (α = .911) and SSSC (α = .841).
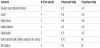
Spearman’s rho nonparametric correlation test for relationships between scores for both scales (SD and SSSC) were analyzed. The two instruments had multiple subscales using a 5 point Likert-type scale with 1 being “strongly disagree” to 5 being “strongly agree.” The SD scale also had two categories of questions; one asked for an assessment rating of satisfaction, the second asked the participant to rate the importance of each item (Table 1).
3.3 Simulation design (SD)
Spearman’s rho correlation coefficient was significant at the 0.01 level for the following student-reported items:
- Simulation cues were appropriate and geared to promote understanding
- Felt supported in the learning process
- Were encouraged to explore all possibilities of the simulation
- Simulation provided the opportunity to set patient goals
- Received constructive feedback
- Obtained instructor guidance/feedback that increased knowledge
3.4 Simulation design (SD)
Spearman’s rho correlation coefficient was significant at the 0.01 level of confidence for the following student-reported items:
- Teaching methods were helpful and effective
- Instructors’ teaching methods were suitable to their way of learning.
- Mastery of the content
- Simulation scenario covered critical content necessary for the mastery of curriculum.
- Instructors used helpful resources to teach the simulation
- The use of simulation as a method of teach critical aspects of nursing skills
3.5 Qualitative analysis
Recorded simulation debriefing sessions were transcribed and analyzed in search for recurrent themes. The resultant two themes included Valuing the simulation learning experience and The importance of interprofessional communication and teamwork (Figure 4).
Theme I: Valuing the Simulation learning experience
- SLP: “For me we had a lot of classroom teaching but not practical application. It is incredibly critical and important to see the practical side of it.”
- SLP: “Learning all the information in the case has meaning to us since we don’t study those details in class. Real life situations are really helpful for our learning.”
- N: “We highly recommend this to be part of the curriculum for nurses.”
Theme II: Importance of Interprofessional communication and team work
- SLP: “The communication is really great and critical. [There were] some things on the chart that we may not have known were explained to us by the nursing students.
- N: “The communication between both teams was really great!”
- SLP: “We felt that we had a team working together since the beginning and this is great!”
4. Discussion
This mixed-methods pilot study was well-received by students and faculty in both nursing and speech-language pathology which is consistent with statements in the literature that contends that “Interprofessional education (IPE) enables effective collaborative practice which . . . optimizes health-services, strengthens health systems and improves health outcomes” [8]. The increasing complexity and delivery of health care coupled with the aging population requires multiple health care professions to deliver collaborative patient care. Nurses are on the front line for identifying those patients who are at risk for aspiration, however, they are not consistently educated to identify and administer a swallow screen, nor is this education provided by SLPs who have the knowledge and expertise on this curriculum content to the healthcare team. This study supports the clarion call proclaimed by to from the Institute of Medicine [23-24], the WHO [8] and The Joint Commission [5,6,25] to develop innovated IPE education strategies that focus on improving patient safety and preparation for collaborative care practice.
Since identifying and managing swallowing difficulties in the acute care setting commonly involve nurses and speech-language pathologists, the authors created an original simulation training involving both disciplines. Although the quantitative results were statistically significant, there were several limitations including the small sample size, lack of randomization, and absence of a control group. In terms of the qualitative data, the use of faculty-led debriefing sessions may have resulted in a Hawthorne effect.
Nevertheless, the simulated IPE experience resulted in the participants’ self-reported satisfaction with the simulation design, education practices and satisfaction/self confidence in the student learning processes.
5. Conclusion
Interprofessional education simulation experiences are valued by students in terms of self-reported satisfaction with learning and increased self-confidence. IPE is endorsed by multiple national and international organizations as well as multidisciplinary accrediting agencies. Consequently, health care educators should consider integrating interprofessional activities such as simulation training to prepare future health care professionals to join the collaborative practice-ready health workforce.
The authors recommend replication of the study using a larger sample size and integrating additional health care disciplines. In addition, future research surveying nursing schools and SLP programs to elicit data regarding nurse swallow screen training and collaborative IPE education curriculum should be conducted.
Competing Interests
The authors have no competing interests with the work presented in this study.