1. Introduction
In 2012, the Japanese population of older adults with dementia requiring nursing care was 4.62 million people [1]. With a rapidly aging population and greater life expectancy [2], it is estimated that by 2025, 25% of the population over the age of 65 will have dementia [3]. The Ministry of Health, Labour and Welfare in Japan [4] has stated that the aim of society should be that someone with dementia should be able to continue to live in a good-quality environment to which are they accustomed, and where they are respected.
In 2000, public nursing care insurance programs were implemented in Japan. There are, however, widely varying needs and families can provide different levels of care, so the care services provided were insufficient to meet needs [5,6]. Extra care is required for people with dementia because of the associated behavioral and psychological symptoms, which places a burden on caregivers and may damage their psychological health [7].
Nuclear families accounted for just 6% of the total number of households in 2012, because of a change in family structure and an increase in family size [8]. At the same time, views on the role of women in society have changed. Women are no longer seen as the sole providers of long-term care, and many older adults live in smaller two-person households [9]. The number of male caregivers of people living at home with dementia has therefore quadrupled from 8.2% in 1981 to 32.2% in 2010. Three-quarters of male caregivers of people with dementia are husbands, and 25% are sons [4,10].
Male caregivers have been reported to have health problems and social issues [9]. They often suffer from depression [11], stress [12], and dissatisfaction [13], and their needs are not represented [9,14-15]. Male caregivers tend not to seek counseling or support from friends and other people [16] and can easily become isolated [17]. Their caring duties often take up so much time that they cannot work or pursue personal interests [18]. These problems can also cause others, reducing quality of life (QOL) and affecting psychological well-being [19].
In this study, we focus on the coping problems experienced by male caregivers of people with dementia living at home. The Care Problems Coping Scale has already been used for family caregivers [18]. However, much of the development of this scale has focused on female caregivers. To assess the status of male caregivers, who often do not seek help even when they have a problem, it is important to develop a coping scale that assesses care problems based on the characteristics of men who care for people with dementia at home. Where care is required on a daily basis, family support is essential for someone with dementia to continue living at home. Nurses can help to provide the necessary support for caregivers, and support them in dealing with long-term care problems.
2. Materials and Methods
2.1 Study subjects
The subjects were 759 male caregivers recruited from four places:
(1) Caregivers of outpatients with dementia at Fukuoka University
Hospital Department of Psychiatry Medicine and Department of
Neurology;
(2) Caregivers of inpatients at the Special Hospital for Dementia in
Fukuoka, Japan;
(3) Members of the Male Caregivers Association in Japan; and
(4) Members of the Dementia Family Association in Japan.
The subjects completed a self-administered questionnaire at some
point between September 2013 and January 2014.
3. Procedure
3.1 Previous studies
Development of the 21-item Care Problems Coping Scale was based on previous studies [12,14,15,20-24]. The results of previous studies were checked against the Sakata Coping Scale, and the results suggested that several statements should not be used. We added two new ones: “I think that needing nursing care is seen as shameful” and “I think that I should be able to manage better than this”. A Care Problems Coping Scale was developed with 21 items in total, and three choices for each response. Cronbach’s alpha coefficient was used to assess reliability. Validity was examined by criterion-related validity [25]. A self-administered, written questionnaire was sent to male caregivers for people with dementia living at home from across Japan (in total 25 prefectures).
3.2 Item analysis
Principal component analysis: items were selected by exploratory factor analysis using Promax rotation.
3.3 Reliability
Reliability was assessed by conducting principal component analysis using Promax rotation. The fixed value factor was 1 or more and factor loadings of items were confirmed to be 0.45 or more. The Cronbach’s alpha coefficient was determined for the total and for each factor.
3.4 Content validity
3.4.1 Concurrent validity
The coefficient of each factor score was examined for significance.
3.4.2 Criterion-related validity
Criterion-related validity was determined using three selfadministered scales: the Japanese version of the Zarit Caregiver Burden Scale (J-ZBI) [26], the Depressive Symptoms and Self-Esteem emotional Scale (SDS) [27], and Rosenberg Self-Esteem Scale- Japanese version (RSES-J) [28,29]. These scales relate to Pearlin’s stress process model of family caregivers for people with dementia [30]. The Pearlin model postulates that coping with the burden of a care situation is perceived subjectively. Self-esteem and self-control are lowered if there is a conflict in the performance of care. If caregivers’ burden is decreased, they may experience physical and psychological changes affecting any symptoms of depression [18].
The J-ZBI scale consists of 22 items. It is a care burden scale that was translated into Japanese by Arai et al. [28]. Its reliability and validity have been verified and it has been used in many previous studies in Japan. Its main focus is the burden arising from care, the burden caused by having to start caring, and the overall care burden. There are five response choices: “Never”, “Rarely”, “Sometimes”, “Quite often”, and “Nearly always”. The maximum score is 84 points.
The SDS scale consists of 20 items. It is also used to assess symptoms of depression and correlates withHamilton's Rating Scale for Depression, often called HAM-D). There are four answer options: “Infrequently”, “Sometimes”, “Often”, “Almost always”. The maximum score is 80 points. Scores in the 20–40 range indicate no or slight depression, the 40–49 range indicates mild depression, and scores over 50 indicate moderate depression.
The RSES-J scale consists of 10 items. It has been used most often in foreign countries. The reliability and validity of the Japanese version were established in 2007. It has four answer options: “Strongly agree”, “Agree”, “Disagree”, “Strongly disagree”. Its maximum score is 40 points.
3.4.3 External criterion by comparison between groups
The participants were divided into three groups based on test scores, and depending on whether their preferred coping methods were considered to be passive, aggressive or other. Comparisons between the groups used the Mann–Whitney U-test. All statistical analyses were performed using the Japanese version of SPSS 22.0 for Windows. The level of statistical significance was set at 0.05 (two-tailed).
3.4.4 Demographic information
Demographic information requested about the caregiver included age, presence or absence of a housemate, household composition, relationship with the care recipient, employment situation, financial situation, subjective judgment of health state, and amount of nursing care provided by time.
The questionnaire also included information about the care recipient, including age, diagnosis of dementia, certification of longterm care need, and degree of autonomy criteria [29].
3.4.5 Ethical approval
We obtained ethical approval for this study from the Kyushu University Hospital Ethics Committee (Approval code: 13-7-07) and the study conforms to the provisions of the Declaration of Helsinki in 1995 (as revised in Tokyo 2004). Consent was obtained from the hospitals, the care facility, the Male Caregivers Association and the Dementia Family Association. The purpose of the study was explained orally and in writing to the relevant parties. Subjects were informed that all information would be treated confidentially. Subjects who returned their completed questionnaires were considered to have consented to inclusion.
4. Results
4.1 Demographic data
4.1.1 Subjects
The mean (± standard deviation) subject age was 69.9 (± 11.1) years (see Table 1). Of the subjects, 89 (32.4%) were 70–79 years old, 78 (27.6%) were 60–69 years old, and 54 (19.7%) were 80–89 years old. Around one third, 91 (33.2%) indicated they had a housemate (other than the care recipient) and the remaining two thirds did not. Almost half, 131 (47.8%) were a single-generation household, 80 (29.2%) were a three-generation household, and 55 (20.1%) were a twogeneration household. The majority of care recipients, 176 (62.4%), had their husband as the caregiver, 105 (37.2%) had a child, and 1 (0.3%) another relative.
Of the caregivers, 99 (36.2%) were employed, 37 (37.4%) were farmers, 28 (28.3%) were company employees, and 22 (22.2%) worked in a family-operated business. The majority, 216 (78.8%), reported that their economic situation was not a hindrance to life. More than half, 162 (59.1%), reported themselves as healthy. The mean amount of nursing care provided was 11.6 (± 8.4) hours; 113 (67.3%) provided 1–9 hours of nursing care, 48 (17.5%) provided 20 hours or more, and 47 (17.1%) provided 10–19 hours. The J-ZBI mean score was 32.8 (± 17.4) and the SDS mean score was 43.3(± 9.6). Results from the SDS for the Three-stage Evaluation showed that 95 (34.7%) subjects were not depressed or only slightly depressed, 89 (32.5%) were mildly depressed, and 80 (29.2%) were moderately depressed. The RSES-J means score was 17.62 (± 4.4).
4.1.2 Overview of people with dementia
The mean age of the people with dementia was 78.3 (± 9.6) years. The largest group, 94 (33.2%), were 80–89 years, 89 (31.2%) were 70– 79 years, and 48 (16.9%) were 60–69 years. By far the largest group were suffering from Alzheimer’s-type dementia, 239 (84.6%), with 26 (9.2%) having cerebrovascular type, and 14 (4.8%) frontotemporal lobar degeneration. Sixty (21.2%) had a care need rating of 1, 53 (18.7%) had a rating of 5, and 45 (15.9%) had a rating of 2 (Table 2).
4.1.3 Day to day functioning and degree of autonomy criteria for older adults with dementia
Sixty-three (22.3%) patients with dementia were rated as “IV: Frequently demonstrates difficulties with communication, symptoms and behaviors that interfere with daily life. Needs continuous nursing care”. Fifty-six (20.0%) were rated as “I: Have some dementia, but home, daily life and social life are almost independent”. Forty-nine (17.4%) were scored as “III: Sometimes demonstrates difficulties with communication, symptoms and behaviors that interfere with daily life. Needs nursing care”. Thirty-eight (13.5%) were considered as “II: Demonstrates a few difficulties with communication, symptoms and behaviors that interfere with daily life. Can be self-supporting if someone is there to guide them”. Thirty-one (11.0%) were rated as “II b: As II. Subcategory: in the home” (Table 3).
4.2 Item analysis
Factor loadings were excluded for “I tend to avoid nursing by distracting or diverting myself ” and “I think that nursing care is not my responsibility” because their loading was less than 0.4. This reduced the scale to 19 items and six factors. The exploratory factor analysis with Promax rotation factor loadings suggested that a further item should also be excluded “I need to encourage myself to provide nursing care” because again, the loading was less than 0.4.
4.3 Reliability
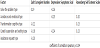
Cronbach’s alpha for all five factors was 0.76. The values for individual factors were 0.79, 0.65, 0.68, 0.67, and 0.67. The factors “I do not think very much about providing nursing care” and “I do not think much about the future” were excluded because their trust factor was less than 0.65. “I have resigned myself to the fact that nursing care is unavoidable” was also excluded, resulting in a 15-item five-factor scale. The contribution rate of each factor was 23.79%, 14.5%, 10.50%, 8.46%, and 7.15%. The cumulative contribution rate is 64.3%(see Table 4 and Table 5).
4.3.1 Labelling the five factors
We identified five types, which we named “Solve the problem type”, “Avoidance and emotional type”, “Transformation cognitive type”, “Careful supervision and waiting type” and “Assistance request type”. The “Solve the problem type” carefully considers the causes of any care problems, collects the necessary information, and then establishes goals. The “Avoidance and emotional type” thinks “I am a caregiver. Dementia is embarrassing”. He does not concentrate on solving care problems, but tends to react emotionally. The “Transformation cognitive type” views care giving as a challenge, and manages it by working harder. The “Careful supervision and waiting type” expects that all will be well if he just waits calmly. The “Assistance request type” is happy to ask for help from others.
4.4 Validity: criterion-related validity
There were significant correlations (P < 0.04) between the Care Problems Coping Scale and total scores on the Japanese version of the Zarit Caregiver Burden Scale, Depressive Symptoms and Self-Esteem Emotional Scale, and Rosenberg Self-Esteem Scale (Table 6). The comparison between the aggressive and passive coping groups showed that they had significantly different levels of depressive symptoms and self-esteem.
There were significant correlations between four factors of the Care Problems Coping Scale and the J-ZBI (r = −0.22 to 0.19), between three factors of the Care Problems Coping Scale and the SDS Threestage Evaluation (r = −0.26 to −0.24), and between three factors of the Care Problems Coping Scale and the RSES-J (r = 0.20 to 0.23). There was no difference in the ZBI as external criteria for the two coping strategy groups, but significant differences were seen with the SDS and RSES-J (P < 0.05) (Table 7).
5. Discussion
We developed the Care Problems Coping Scale for male caregivers to help them to continue caring for someone with dementia at home. This study has tested its reliability and validity.
5.1 Reliability
We examined the reliability by measuring internal consistency.
The Cronbach’s alpha coefficient for the whole scale was 0.76 and for each individual factor is 0.79, 0.65, 0.68, 0.67, and 0.67. This provides sufficient reliability and internal consistency for use. The contribution rates of each factor showed that they were not equally weighted. However, this needs further examination. This scale is designed for use in clinical practice.
5.2 Label and Validity
We identified five factors or types, including “Solve the problem”, “Avoidance and emotional”, “Transformation cognitive”, “Careful supervision and waiting” and “Assistance request” types. The “Solve the problem” type considers that if care cannot be implemented as intended, he can collect the necessary information for planning and then implementing the plan, and believes this is a reason to take positive action. The “Avoidance and emotional type” struggles not to abandon care giving through frustration, and also feels embarrassment and wishes to avoid the situation. The “Transformation cognitive type” faces the challenges of providing care, and works in good faith to do so. These three relate to the categories of Pearlin et al [30], described as “problem-solving”, “cognitive”, and “emotional” types. We have added a further two. The “careful supervision and waiting type” is also thought to be optimistic, as they remain calm despite problems. The “Assistance request type” is happy to ask for help from those around. To assess criterion-related validity, we measured our scale against several proven tools. These included a care burden scale, and a depressive symptoms scale. In-scale scores of self-esteem feelings showed a significant correlation. There was a significant difference between positive and negative coping groups. These suggest that the new scale will operate effectively to assess the coping status of male caregivers for people with dementia living at home.
6. Feasibility and Significance
The National Livelihood Survey of 2010 [31] showed that the proportion of men acting as the “principal caregiver” was 32.8%.The population in Japan is aging; in 2014, it was estimated that, on average, women live approximately 7 years longer than men. The number of one-generation households is increasing, while the number of threegeneration households is decreasing [4]. This means that there will be an increasing need to provide support specifically for men who provide care at home.
7. Limitations and Challenges
This study had several limitations. For example, there were some regional characteristics of the subjects. The study was based on a survey across Japan [32], but members of organizations such as the Family Association accounted for about 50% of the sample. Family members may have shared information and concerns with each other and may have encouraged each other [33,34]. Men may choose not to share their difficulties, and do not always want to receive support, which may have affected responses.
Another limitation is that the average age of the subjects was 69.9 years; these were all older adults who may respond differently from younger people. More than half the subjects were not working. According to employment status research from 2007 [4], many caregivers have to leave or change their jobs to provide care. Future investigations should test whether differences such as employment status affect the experiences of care giving. We wanted to ensure the stability of the Care Problems Coping Scale, and therefore selected items that overlapped with other studies. This means that our scale can be used to easily evaluate care problems of male caregivers [35-40].
8. Conclusion
We have developed and tested a scale to measure Nursing Care Problems with Coping for Male Caregivers for People with Dementia Living at Home. This scale has demonstrated validity and reliability, resulting in a scale of 15 items and five factors. The five factors were divided into “Solve the problem”, “Avoidance and emotional”, “Transformation cognitive”, “Careful supervision and waiting” and “Assistance request” types.
Competing Interests
The authors declare that they have no competing interests exists.
Author Contributions
All the authors substantially contributed to the study conception and design as well as the acquisition and interpretation of the data and drafting the manuscript.
Acknowledgments
We are very grateful to the doctors who cooperated with us at Takita Memory Mental Health Clinic and Monowasure Mental Health Clinic, and to Masanobu Yamaguchi, who explained associate family support groups to us.