1. Introduction
Neck pain is a very common problem, second to low back pain in its frequency in the general population as seen in musculoskeletal practice [1].
Neck pain has a postural or mechanical basis affects about twothirds of people at some stage, especially in middle age. Acute neck pain resolves within days or weeks but may become chronic in about 10% of people [2].
Mechanical neck dysfunction (MND) can result from poor or faulty posture, overuse injuries, or trauma. Neck posture can be affected by sedentary lifestyles such as prolonged sitting in front of the computer, watching television, electronic games, and office work [3,4].
Mechanical neck dysfunction (MND) is a type of dysfunctional syndrome caused by mechanical deformation of structurally impaired tissues. When affecting articular structures, the dysfunction syndrome is characterized by intermittent pain and a restriction of endrange movement. When affecting contractile structures, functional impairment is demonstrated when the muscle or tendon is loaded at any or certain points during the physiological range, especially with resisted loads. Movements and positions consistently cause pain to be produced, but symptoms cease when the position or loading is ended [5].
Mechanical neck dysfunction affecting the cervical spine, characterized by intermittent cervical pain from the area between the superior nuchal line till the first thoracic vertebra [6].
Traditional treatment of mechanical non-specific neck pain includes patient education and physical exercises, primarily as preventive methods. In more acute or severe cases, spinal manipulation, physical therapy, or medicinal or injection therapies may be applied. However, additional treatment options are needed, especially for patients with more severe pain or with low expectations of conventional treatment alone [7].
Cervical traction is often used as a treatment choice by physical therapists for treating mechanical neck pain; however, there is a varying opinion about the methods of application and clinical results associated with traction [8].
Cervical traction is commonly used for treatment in outpatient rehabilitation. Although often used clinically, the therapeutic effect of cervical traction remains inconclusive for patients with chronic neck disorders [9,10].
Rath divided cervical traction application into three categories: manual, mechanical, and self-traction (home traction) [11].
Mechanical traction is applied as continuous and intermittent (rhythmic and progressive) forms [12].
Continuous traction pulls continuously for the desired length of each treatment session for about 10 to 60 minutes with a mean of 25 minutes continual sessions during the day with frequent rest (one hour pull and half an hour rest) intervals and no traction at night may be recommended in acute severe pain. This is accomplished with traction machines set up in the physical therapy department [12,13].
Intermittent traction involves traction and releases with a known amount of force applied. The advantages of this technique are the effect on circulation and stimulation of mechanoreceptors in the capsules, ligaments, tendons, and joints. It is ideal for the less acute and less critical cervical diseases and injuries. Intermittent traction allows a gradual, slow rate of pull and release of traction [14]. It has two forms, one form involves traction and releases with a known amount of force applied. This is called rhythmic intermittent traction. In the other form, the traction force is progressively increased and decreased in the repetitions of the on-off cycle [15].
Physical therapy modalities are increasing day after day. Looking for a safe, low cost and effective modality is one of the physical therapy research goals. Cervical traction therapy has been widely adopted in clinics and rehabilitation centers. Over the year, many studies have demonstrated its positive effects on cervical and lumbar spine-related pain (16). However, Harte, A. et al. [17], Daniel D.M. [18] and Wong L.K.F et al. [19], pointed out that further research is needed since there is not enough conclusive evidence to fully support the contribution of the therapy.
As Traction can be applied manually or by use of motorized units. Motorized traction can be applied intermittently or continuously. The current study aims to compare the efficacy of intermittent and continuous traction in the treatment of MND.
2. Subjects and Methods
2.1 Participants
Forty-five patients were diagnosed with MND referred from the orthopedic department to the physical therapy department of Derb-Nigm general hospital, Al Sharqia, Egypt in the period from September 2020 to February 2021. Patients were chosen based on inclusion criteria and exclusion criteria. All Patients received 3 sessions per week for 4 weeks. Written Informed consents were being received from all participants after a brief but detailed explanation about the aims, benefits, and risks involved with this study. This study was approved by the Ethics Committee for Scientific Research of the Faculty of Physical Therapy, Cairo University. Pan African Clinical Trial Registry number is (PACTR202102867579609).
2.2 Inclusion criteria
Forty-five patients of both sexes with age ranged from 20-40 years [8]. Referred from orthopedic consultants with acute mechanical neck dysfunction. The neck disability index (NDI) is above 5 [20]. Pain scale scores between 4 to 9 to ensure group homogeneity and Patients will be able to perform (ROM) test of the cervical spine.
2.3 Exclusion criteria
Subjects excluded were with neck pain that was not of mechanical origin, history of previous neck trauma or head injuries, Ankylosing spondylitis, osteoporosis, cervical rib syndrome, post-surgical neck conditions, open wound over the cervical region, internal fixation of cervical vertebrae, Cerebrovascular abnormalities, rheumatic arthritis.
2.4 Interventions
Group (A) Control Group: fifteen patients received a traditional physical therapy program (A- Infrared radiation for 15 minutes, B-Exercise consists of 1) Stretching exercises of the upper trapezius, sternocleidomastoid, Levator scapulae, and scalene (passive stretch withhold for 30sec. and relax 30sec. repeated 3 times.), 2) isometric exercises for Neck Flexors, extensors, side-binding muscles (patient hold 6sec. after maximum contraction against maximum manual resistance given by the therapist then relax 6sec. repeated 5 times) and C-Posture exercise program: The seated patient performed postural exercises to the maximum pain free ranges of motion, Combined movements were also performed to improve the neck posture. Each exercise was performed as 3 sets of 10 repetitions each, 3 times/ week for 4 weeks. The patients were instructed to continue the posture exercises as a home program to influence the self-correction kinesthetic awareness [20-23].
- Group (B) intermittent traction group: comprised of fifteen patients given intermittent traction in addition to the traditional physical therapy program.
- Traction parameters: intermittent traction was given while the patient supine on the treatment table with the body in a neutral position. the cervical spine was placed at an angle of approximately 15 degrees of flexion with traction force to be 10% of the subject's body weight for 15 min with a 60s hold time and 20s and the relaxation force of 50 percent of the pull force release time for a total time of treatment 15 min [24].
- Group (C) continuous traction group: comprised of fifteen patients given continuous traction in addition to the traditional physical therapy program.
- Traction parameters: continuous traction was given while the patient supine on the treatment table with the body in the neutral position the cervical spine was placed at an angle of approximately 15 degrees of flexion with traction force to be 10% of the subject's body weight for a total time of treatment 15 min with the static mode of traction [25].
Study duration: All groups received 3 sessions per week for 4 weeks.
Outcome measures: VAS, NDI, CROM
2.5 Instrumentation
2.5.1 Evaluative instrumentations
- Visual analogue scale.
- Bubble inclinometers.
- Neck Disability Index.
2.5.2 Treatment instrumentation
- Traction apparatus. (ITO TM 400) made in Japan
- Infrared radiation. Model is 4004/2N.
2.6 Procedures of the study
2.6.1 Measurement procedures
Subjects were referred from the orthopedic department with mechanical neck dysfunction achieving the inclusion criteria then all the methods of treatment and exercise treatment used in this study and treatment advices and the home program exercise were explained to the patients after they freely and voluntary accepted to participate in this research program.
- The patients were divided randomly by giving the patient numbers and putting them in a bowel, then pull the numbers and assign them to groups A, B, and C consequents.
- The Pain was assessed by a visual analog scale (VAS 10cm line with 0 (no pain) and 10 (worst pain) on the other end. Patients were asked to place a mark along the line to denote their level of pain [26].
- Then use the Neck Functional disability index by asking the patients to Read the questionnaire which was designed to enable us to understand how much neck pain has affected the ability to manage everyday activities. By answer each Section by circling the ONE CHOICE that most closely describes the problem. Then simply count up the points and plug the total in below: For each question, there is a possibility of 5 points: 0 for the first question, 1 for the second question, 2 for the third question, etc [27].
- Then measuring cervical ROM using the Bubble inclinometers Adapted from Norkin and White, (2003) [28], as follow:
- (ROTATION ) Lay subject supine, with head in neutral position • Place inclinometers on the forehead, set zero • Rotate neck • Read result
- (Side binding) Put head in neutral position • Place inclinometers on top of the head, set Zero • Abduct neck • Read result
- (neck flexion & extension) Put head in the neutral position, Place inclinometers on top of the head, set zero, Flex or extend the neck, Read result
2.6.2 Treatment procedures
All patients met the inclusion criteria and divided randomly into three equal groups. All groups received 3 sessions per week for 4 weeks. The physical therapist discussed the aims and methods of treatment for the patient at the beginning of the treatment. Three programs of treatment had been used in this study, 1) Traditional physical therapy program: was added for all groups (A and B and C). 2) Intermittent traction: was applied for group (B). 3) Continuous traction: was added for group (C) as described above.
2.7 Data collection
Data obtained from the three groups regarding neck disability index, visual analogue scale, and neck range of motion were calculated before starting the treatment and after 4 weeks of intervention. The measured variables were statistically analyzed and compared using SPSS for windows version 25 (SPSS, Inc., Chicago, IL).
2.8 Normality test
Data were screened for normality assumption, homogeneity of variance, and presence of extreme scores. Shapiro-Wilk test for normality showed that the measured variables were normally distributed (p >0.5).
3. Results
3.1 The baseline demographic characteristics of participants
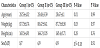
The baseline demographic characteristics of subjects are shown in Table 1. The mean and standard deviation (M±SD) of age, the body, weight. The results showed no statistically significant differences among groups regarding age, weight, height, and gender (P>0.05).
3.2 Results of Mixed design multivariate analysis of Variance (MANOVA)
Mixed design multivariate analysis was conducted to assess the difference between participants in the three groups in the amount of change in their scores on the outcome measures. Statistically Significant multivariate effects were found for the main effects of groups.
3.3 Results of Mixed design analysis of Variance (ANOVA)
Follow-up univariate ANOVAs reveal a significant change in the outcome of all variables (VAS, NDI, flexion ROM, extension ROM, right lateral flexion, left lateral flexion, right rotation ROM, and left rotation ROM).
3.4 The baseline clinical characteristics of participants
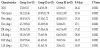
The baseline clinical characteristics of subjects are shown in Table 2 showed no statistically significant differences among groups regarding neck disability index, pain, and neck range of motion outcome measures (P>0.05).
3.5 Clinical characteristics of Subjects after 4 weeks of intervention
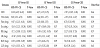
The clinical characteristics of subjects after 4 weeks of intervention are shown in Table 3 showed statistically significant differences among groups regarding neck disability index, pain, and neck range of motions outcomes (P<0.001).
3.6 Between-groups comparison
There were no statistically significant differences between the groups in neck disability index, pain, flexion, extension, right rotation, left rotation, right lateral flexion, and left lateral flexion outcome measures (p>0.5) at baseline. However, there were statistically significant differences between groups I and II in neck disability index, pain, flexion, extension, right rotation, left rotation, right lateral flexion, and left lateral flexion outcome measures (p< 0.001) after 4 weeks of interventions in favor of group II. Comparing groups, I and III, there were statistically significant differences in pain, flexion, extension, right rotation, and left rotation in favor of group III (p< 0.05), but not in neck disability index, right lateral flexion, and left lateral flexion outcome measures (p> 0.05) after 4 weeks of interventions. In addition, there were statistically significant differences between group II and III, in favor of group II, regarding neck disability index, pain, flexion, extension, right rotation, left rotation, right lateral flexion, and left lateral flexion outcome measures (p< 0.001) after 4 weeks of interventions, as in Table 2 and 4.
3.7 Within-group comparison
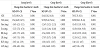
There were statistically significant differences in neck disability index, pain, flexion, extension, right rotation, left rotation, right lateral flexion, and left lateral flexion outcome measures (p< 0.001) after 4 weeks of treatment in each group when compared to the baseline data as in Table 5.
4. Discussion
This study was designed to investigate and compare the efficacy of intermittent versus continuous traction on pain, disability, and neck range of motion in patients with mechanical neck dysfunction (MND). It was found from the analysis that 4 weeks of interventions consisting of the application of Mechanical intermittent Cervical Traction with traditional physical therapy program for the subjects in Group B shown a statistically significant greater percentage of improvement in pain, functional disability, and cervical ROM than Group C who received Mechanical continuous Cervical Traction and Group A who received traditional physical therapy program.
4.1 Regarding the effect of exercise program on MND
Exercises therapy aimed to improve the performance of the cervical muscles, decrease pain, and improvement of functional disability associated with MND [29], in addition, to increase cervical ROM and head excursion [30].
The using of exercise program can relax the tense soft-tissues through stretching exercise which decreasing spasm of the muscles and improve the circulation which decrease the concentration of metabolites. Strengthening and stretching weakened or strained muscles is usually the first treatment that is advised [29].
The results of this study in agreement with Lars et al., (2014) who stated that strength training had high clinical relevance and led to marked prolonged relief in neck muscle pain [31].
Similarly, Ylinen et al. (2007) compared between stretching exercise and manual therapy on non-specific neck pain and disability. Measurements were done after 4 weeks and 12 weeks, and there were significant improvements in both groups in neck pain and disability with no difference between both groups. They concluded that stretching exercises can be recommended in the first instance as an appropriate therapy intervention to relieve pain, at least for the short-term treatment [32].
In particular, exercise is an evidence-based practice to not only relieve pain in individuals with nonspecific neck pain, but also to improve muscle strength, motor function, and quality of life [33].
4.2 Regarding the effect of cervical traction on MND
Both of intermittent and continuous traction are sharing in cervical joint distraction which may loosen adhesions within the dural sleeves, reduce compression and irritation of disks, and improve circulation within the epidural space [34,35]. The mechanism by which (ICT) reduces neck & arm pain is possibly by unloading the components of the spine by stretching muscles, ligaments & functional units [36].
In comparison of results of three groups, group B which using intermittent traction was better than in the group C which using continuous traction because of intermittent traction may be better tolerated than continuous traction in some patients [37].
For decades, cervical traction has been applied widely for pain relief of neck muscle spasm or nerve root compression. It is a technique in which a force is applied to a part of the body to reduce paravertebral muscle spasms by stretching soft tissues, and in certain circumstances separating facet joint surfaces or bony structures.
Some authors believe that traction, especially with a slight degree of neck flexion, could open the posterior articulations, widen the intervertebral foramen, disengage the facet surface, and elongate the posterior muscular tissues and ligaments [38].
Traction reduces the potential for damage decrease pain, improve function, and cervical ROM as it stretching numerous soft tissues that surrounding the nucleus pulposus as annulus fibrosus, ALL, and PLL, along with other segmental ligaments and muscles which help to stabilize the spine [39]. These soft tissues when overloaded lead to spinal instability which may, in turn, cause mechanical and chemical irritation of the surrounding structures [40].
The physiological effects of traction may include separation of vertebral bodies, distraction, and gliding of facet joints, widening of the intervertebral foramen, stretching of ligamentous structures, straightening of spinal curves, and stretching of spinal musculature. Traction has also been reported to decrease pain by providing muscle relaxation, stimulation of mechanoreceptors, and inhibition of reflex muscle guarding [41].
The therapeutic effects of traction are due to various mechanisms such as it causes unloading of the components of the spine, stretches the muscles and ligaments, reduces the adhesions in the dural sleeves, and nerve root decompression within the foramina, thereby reducing distal symptoms. It is suggested that it relieves tonic muscle contractions which improve vascular status within epidural space and perineural structures and decreases pain by providing muscle relaxation, stimulation of mechanoreceptors, and inhibition of reflex muscle guarding [41,42].
This also agrees with the results of Bid, D et al. [8] who concluded that even though conventional therapy is effective the addition of intermittent cervical traction gives better results in the management of mechanical neck pain as they investigate the effectiveness of mechanical cervical traction on patients with unilateral mechanical neck pain.
Claudio C et al. [43] Meta-analyses revealed a low quality of evidence: Traction seems to be superior to other conservative treatments when combined with those treatments in reducing pain in patients with CRS at a three- to four-week follow-up assessment, but the findings were not clinically relevant. The results of subgroup analyses were statistically significant only for mechanical and continuous, but caution in interpreting the results is warranted due to a widely adjusted confidence interval and lack of clinical relevance.
Graham N et al. [44], concluded that Inconclusive evidence for both continuous and intermittent traction exists due to trial methodological quality. Given the methodological quality limitations, 2 clinical conclusions may be drawn, as follows:
- Data analysis reveals moderate evidence of benefit for intermittent traction, which denotes findings in a single, high-quality RCT or consistent findings in multiple low-quality trials.
- There was moderate evidence of no benefit for continuous traction. Implications for research.
On the other hand, In a Cochrane review on mechanical traction for neck pain with or without radiculopathy, Graham et al. [9], concluded that the literature does not support or refute the efficacy or effectiveness of continuous or intermittent traction for pain reduction, improved function or global perceived effect when compared to placebo traction, tablet or heat or other conservative treatments in patients with chronic neck disorders. The authors stated that large, well-conducted RCTs are needed to first determine the efficacy of traction.
Also, our results disagree with Borman et al. [45], who examined the effectiveness of intermittent cervical traction in the treatment of chronic neck pain. The authors concluded that no specific effect of traction over standard physiotherapeutic interventions was observed in adults with chronic neck pain.
Himanshi et al. [46], stated that conservative treatments which include tens, neck strengthening exercises are more effective than the effectiveness of intermittent cervical traction for pain reduction; improve function in the management of cervical radiculopathy.
Thoomes et al. [47], found that cervical traction was not effective in the treatment of CRS whereas. Romeo et al. [48], reported an overall statistically significant effect of combining traction with other conservative treatments versus other conservative treatments individually.
Meta-analysis of randomized controlled trials (RCTs) by Yang JD et al. (2017) [49], assessed the neck pain-relieving effect of intermittent cervical traction (ICT). The results indicated that patients who received ICT for neck pain had significantly lower pain scores than those receiving placebos did immediately after treatment. The pain scores during the follow-up period and the neck disability index scores immediately after treatment and during the follow-up period did not differ significantly.
The reasons for the differences in the effects of intermittent and continuous traction may due to rhythmic cycling of traction and releases which occurred during intermittent traction result in increasing the frequency of myoelectric signals, improving blood flow in affected muscles, promotes neck muscles relaxation by reduces reflexive muscle guarding , and improving the imbibitions sign of disc nutrition [50]. Intermittent traction is preferable in improvement of cervical ROM consequently to pain reduction which is responsible for the improvement in muscle function.
5. Conclusions
Both traction methods intermittent and continuous are effective when used as an adjunct to a traditional physical therapy program in patients with mechanical neck dysfunction in favor of intermittent cervical traction (ICT).
Competing Interests
The authors declare that they have no competing interests.