1. Background
According to the World Health Organization (WHO), the proportion of older adults, over the age of 60, in the total global population will move from 12% to 22% in 2050 [1]. In Japan, the percentage of individuals aged 65 or older will be almost 40% of the total population by 2065 [2]. In old age, physical function, such as the ability to balance and muscle strength, declines, and is related to disability and dependency in daily life [3-5]. Therefore, it is important to adequately and quickly understand older adults’ physical function and prevent a decline in their ability to carry out activities of daily living (ADL).
The short physical performance battery (SPPB) comprises the following tests: standing balance (side-by-side stand, semi-tandem stand, and tandem stand), comfortable 4-m gait speed, and fiverepetition chair-stand tests [6]. SPPB can be used to assess multiple physical functions, such as balance, gait, strength, and endurance in older adults [7]. SPPB has been recognized as a standard assessment tool used in clinical trials [7,8]. A lower SPPB score is associated with ADL difficulty in community-dwelling older adults [9].
The ability to carry out ADL declines with age in older adults, and there is a particularly higher incidence of a decrease in ADL ability in older adults requiring care [10-12]. There is a strong possibility that the number of older adults requiring care will increase with an increasing proportion of older adults. However, little is known regarding the cut-off value of SPPB in the explanator of independence or dependence in carrying out ADL in older adults requiring care. Clarifying the cut-off value for SPPB could be a useful screening test for the detection of participants requiring care in whom the ability to carry out ADL may decline.
The purpose of this cross-sectional study was to clarify the cut-off value for SPPB with respect to the ability to carry out ADL in older adults requiring care. We expected that the cut-off value for the SPPB score should be able to discriminate the older adults requiring care who need even more assistance in doing ADL from those who don’t need more assistance in carrying out ADL.
2. Materials and Method
2.1 Participants
In the present cross-sectional study, we recruited 37 participants aged 60 years or older who are adult day care facilities users or geriatric health services facility residents [12 men, 25 women, average age (standard deviation: SD): 84.0 (7.3) years] using long-term care insurance in Japan. Participants were excluded if they: 1) could not provide complete measurements, 2) had difficulty walking alone (except with supervision), 3) had fractures and/or stroke within the past 3 and 6 months, respectively. The level of long-term care insurance is divided as 7 grades (support levels 1 and 2, and care levels 1, 2, 3, 4 and 5) in Japan, and care level 5 is judged as most severe. The level of longterm care is generally judged by converting the time and effort it takes to care in time. The criterion time for support levels 1 and care level 5 is from more than 25 min to less than 32 min, and more than 110 min, respectively. The number of our participants in each category was as follows: support levels 1 (n = 2) and 2 (n = 3); care levels 1 (n = 16), 2 (n = 9), 3 (n = 3), 4 (n = 3) and 5 (n = 1). Frailty is defined as a previous stage of the conditions requiring care in Japan [13]. All participants read and signed an informed consent form, and this study was approved by the Ethics Committee of the Health Science University.
2.2 Short physical performance battery (SPPB)
Physical function was measured using the SPPB which consists of standing balance (side-by-side stand, semi-tandem stand and tandem stand), 4-m gait speed and five-repetition chair-stand tests [6]. Each individual test was scored from 0 to 4 points, with a larger score indicating a better physical function; the total (overall) score ranged from 0 to 12 points. Gait speed was measured twice, and the higher speed was used as a representative value.
2.3 Barthel index (BI)
BI was used to measure the ability to carry out ADL [14], and was based on 10 items [total score ranged from 0 to 100 points]: moving from a wheelchair to a bed and back (0, 5, 10, or 15 points), walking (0, 5, 10, or 15 points), eating (0, 5, or 10 points), getting on and off the toilet (0, 5, or 10 points), ascending and descending stairs (0, 5, or 10 points), dressing (0, 5, or 10 points), bowel control (0, 5, or 10 points), bladder control (0, 5, or 10 points), grooming activity (0 or 5 points), and bathing (0 or 5 points). The higher point values indicate less need for assistance in ADL. The total BI score of ≥85 points indicates that a subject is able to the ability to carry out ADL with minimum help [15-17].
2.4 Statistical analysis
Statistical evaluation was carried out using the JMP 11 software (SAS Institute Inc., Cary, NC, USA). The values were expressed as the mean ± standard deviation (SD) or median [interquartile range (IQR)]. Minimal sample sizes were 8.8 (cases) and 26.3 (controls) [area under the curve (AUC) = 0.80, significant level = 0.05, power 0.80, kappa 3] and 9.8 (cases) and 19.5 (controls) (AUC = 0.80, significant level = 0.05, power 0.80, kappa 2) using the R Package “pROC” (version 1.16.2), respectively. The participants were divided into 2 groups: Group 1 (BI ≥85) and Group 2 (BI <85). According to a shapiro-wilk test, an unpaired t-test (both parametric data), Wilcoxon ran sum test (either or both nonparametric data) and a chi-squared test were conducted to compare gender, age, height, weight, BMI, SPPB score, and BI between the 2 groups. The relationship between BI and SPPB was evaluated using multiple logistic regression analysis adjusted for confounding factors. Moreover, a receiver operating characteristic curve (ROC curve) was used to define the cut-off value for the division into 2 groups [Group 1 (BI ≥85) and Group 2 (BI < 85)]. The significance was set at p< 0.05.
3. Results
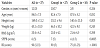
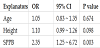
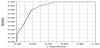
The characteristics of 2 groups are shown in Table 1. There were significant differences in height (Group 1 152.1 ± 9.6 cm vs Group 2 140.4 ± 11.0 cm, p <0.05) and central tendency for age (Group 1 82.6 ± 7.5 years vs Group 2 87.8 ± 5.2 years, p = 0.052), but no differences in gender, weight and BMI between 2 groups (weight: Group 1 46.3 ± 10.2 kg vs Group 2 42.0 ± 9.0 kg ; BMI: Group 1 20.0 ± 4.1 kg/m2 vs Group 2 21.4 ± 4.5 kg/m2, p >0.05). The SPPB score were significantly lower in Group 2 than in Group 1 [Group 1 7(5) vs Group 2 4(1.5), p <0.05]. In multiple logistic regression analysis [Group 1 (BI ≥85) and Group 2 (BI < 85)] adjusted for height and age, BI was independently explained by SPPB score [Odds ratio (OR) 2.35, 95% confidence interval (95% CI) 1.25 - 6.72, p < 0.05, Table 2), but no age and height (age: OR 1.05, 95% CI 0.83-1.35 ; height: OR 1.10, 95% CI 0.99-1.26, all p >0.05, Table 2). Furthermore, using a ROC curve for BI, the cutoff value for the SPPB score was 4 points (sensitivity 0.80, specificity 0.81, and AUC 0.88) (Figure 1).
4. Discussion
The SPPB score in Group 1 (BI <85) was significantly lower compared with that in Group 2 (BI ≥85). The SPPB score was also an independent explanator of BI, and the cut-off value for the SPPB score was 4 points. These findings suggest that the cut-off value of the SPPB with respect to the ability to carry out ADL could be useful in the detection of participants requiring care who will need to be even more assisted in daily basis.
In the present study, the value of AUC using ROC curve is 0.88. The values of AUC that ranged from 0.7 to 0.9 and from 0.9 to 1.0 are classified as a moderate and high accuracy, respectively [18]. In addition, Shimada et al. (2013) in a study involving 6791 participants aged 65 years or older requiring personal care (age; 82.6 ± 6.7 years) have reported that average comfortable gait speed is 0.7 ± 0.3 m/sec [19]. The average age and comfortable gait speed of our participants in this study were 84.0 ± 7.3 years and 0.63 ± 0.23 m/s, respectively. Therefore, we relatively recruited the general population, and the cutoff value for the SPPB score in the present study could be a suitable indicator for the ability to carry out ADL in older adults requiring care.
Using the BI, the cut-off value of the SPPB score in the present study was calculated to be 4 points. The total score in SPPB is 12 points and larger score indicate a better physical function [6]. A score of 4-6 points in SPPB is classified as low performance individuals, and the ratio of mobility-related disability in participants who score 4-6 points is approximately 3-5-times higher than in high performance individuals (10-12 points) [11]. The participants in this study acquired some assistance in carry out the ADL using long-term care insurances. Besides, if the total score of the BI was more than 85 points, a subject is deemed to have the ability to carry out ADL with minimum help [15-17]. Hence, the cut-off value (4 points) of the SPPB score in the present study is a useful indicator of the ability to carry out ADL in older adults requiring care.
One limitation of the present study is the small number of participants. Minimal sample sizes were 8.8 (cases) and 26.3 (controls) (AUC = 0.80, significant level = 0.05, power 0.80, kappa 3) and 9.8 (cases) and 19.5 (controls) (AUC = 0.80, significant level = 0.05, power 0.80, kappa 2) using the R Package “pROC” (version 1.16.2), respectively, but we need to recruit more participants in future studies. Besides, an association between cause and effect could not be revealed due to the cross-sectional design of the present study. Future studies are needed to investigate the manner in which physical function affects the ability to carry out ADL in older adults requiring care in a prospective cohort. Cognitive function is related to the ability to carry out ADL in older adults [20] and we need to clarify the effect of cognitive function on SPPB and the ability to carry out ADL in future studies. Moreover, the functional independence measure (FIM), which is an evaluation method of ADL is divided into 7 scales (1-7) for each item [21], and it can evaluate the ability to carry out ADL in detail. The relationship between FIM and SPPB need to be considered in future studies.
5. Conclusions
Through the use of the BI, we determined that the SPPB score in the group that had lesser ability to carry out ADL was significantly lower than that in the group that had higher ability to carry out ADL. The SPPB was also extracted as an independent explanator of BI, and the cut-off value for the SPPB score was 4 points. Our results suggest that SPPB could be useful in explaining the ability to carry out ADL in older adults requiring care.
Competing Interests
The authors declare that they have no competing interests.