1. Introduction
The scapula plays an important function in the shoulder position, movement, stability, muscle performance and motor control. So that, for an efficient movement of the arm and alignment of the glenohumeral joint, a coordinated scapulohumeral rhythm is required [1]. Alterations in the positioning and movement of the scapula have been recognized as clinical indication of dysfunction and termed scapular dyskinesis [2].
Among the dysfunction that characterizes the scapular dyskinesis, a winged scapula, characterized by prominence of the medial scapular border, has been associated with some disorders or diseases that affect the shoulder joint complex, such as impingement syndrome, joint instability and inflammatory processes involving the rotator cuff tendons [2-5]. The measurement of the medial scapular border prominence in clinical practice is potentially difficult and it can lead to misdiagnosis. Therefore, defining a precise method for evaluating posterior scapular displacement is essential to assist in diagnosis of scapular dyskinesis.
Current literature has discussed and emphasized the importance of developing instruments to assess quantitatively the scapular dyskinesis [6-8]. It is through this need that new techniques and tools have been developed with the aim of analyzing the different scapular movements in a simple and reproducible manner. However, there are few studies that assess the reliability of the instruments [6,8-13].
Seeking an objective and practical technique to evaluate the posterior scapular displacement, Plafcan et al. [5] developed the Perry Tool, an instrument that measured angle between the transverse plane and the line joining the inferior angle of the scapula and the spinous process of the corresponding vertebra. This tool showed an intratester within day reliability ranged from 0.97 to 0.98 and intertester within day reliability ranged from 0.92 to 0.97. However, Weon et al.[14] contested the validity of the measurement taken by the Perry Tool seen that this value could be influenced by the scapular abduction and proposed a tool that was able to measure the scapular displacement in centimeters, called scapulommeter.
According to Weon et al. [14] data, the scapulommeter showed an excellent reliability coefficient (ICC - 0.97), but the value proposed by the researches to determine scapular dyskinesis were randomly and arbitrarily established by researchers. Thus, a validation study for this toll is still needed. This study was designed to evaluate the reliability, sensitivity and specificity of the linear scapulommeter in order to validate it as a tool for objective evaluation of posterior scapular displacement. In addition, we aimed to determine a cut-off value and compare it with the value set by Weon et al. [14].
2. Materials and Methods
2.1 Participants
Fifty subjects (42 men and 8 women, with a mean and standard deviation age of 21.92 ± 2.38 years, body mass 67.49 ± 11.2 kg, height 1.71 ± 0.07 m) took part in this study. In this study, were included subjects who met the inclusion criteria: classified as physically active by the short version of the International Physical Activity Questionnaire (IPAQ)[15], between 18 and 35 years, without history of fractures and surgeries on the shoulder girdle and neck, peripheral nerve injury, degenerative joint disease, and glenohumeral and acromioclavicular instability. This study was approved by a Research Ethics Committee (Protocol number: 078/12 CEP-UPE) and all participants signed a consent form.
2.2 Observational method for assessing scapular dyskinesis
Video recording was used for clinical evaluation of the scapular movement. Each volunteer remained in an orthostatic position, and executed three repetitions of bilateral movement of shoulder abduction in the scapular plane, from 0° to 120° angle. Execution of the movement was recorded in posterior view by a digital video camera with a 60 Hz sampling rate (SONY DCR - SX21), positioned on a 1.00 meters height tripod, and 2.85 meters far from the subject. Floor markings were used to standardize the positioning of the camera and subject in all sessions, as well as markings on the wall were used to define the limit of movement (120° abduction) of the upper limbs, according to previous goniometer measurement. All recordings were performed in an environment with adequate lighting and without any shadows that might compromise the video quality. In addition, a metronome was used to control the movement speed (three seconds for the each concentric and eccentric phases)[3].
Evaluation and categorization of the type of scapular dyskinesis was taken following Kibler et al.[2] guidelines: type I dyskinesis is the prominence of the inferior medial scapular angle, representing loss of scapular control about a horizontal axis parallel to the scapular spine; type II is the prominence of the medial scapular border, representing loss of scapular control about a vertical axis parallel to the spine; type III is the prominence of the superior scapular border, representing excessive upward movement of the scapula and loss of control around a sagittal axis through the scapula; type IV is considered to be the symmetric scapulohumeral motion, with no prominence or excessive motion relative to the uninvolved shoulder. Once asymmetry was identified, the evaluators were asked to classify the dyskinesis in one of these four types, based on the predominant pattern [16]. In a second step, all individuals classified with scapular dyskinesis (type I, II or III) were grouped into a single category: "with posterior scapular displacement" and subjects classified as type IV were included in the category "without posterior scapular displacement".
Two physiotherapists performed the video evaluation of the scapular dyskinesis independently. When there was disagreement on the evaluator’s classification, a third assessor was asked for a consensus.
2.3 Scapulommeter method for assessing scapular dyskinesis
A replica for the scapulommeter as proposed by Weon et al. [14] was built, to measure in millimeters the scapular inferior angle posterior displacement. The instrument consists of a vertical plate 14 cm height, 14 cm of width and 1.5 cm thick. The circular pads (2 cm of diameter and 2 cm height), attached near each scapulommeter end, allows for be comfortably placed on the body. A hand support was positioned on the back surface of scapulommeter allowing it to be easily handled. There is a flat sliding plate with two parallel guides on the upper surface of the equipment, which allows the anteroposterior displacement between them (Figure 1).
For measurement, the examiner stayed behind the subject, the four pads were placed on the thorax wall and the sliding plate at the level of the inferior angle of the scapula. The examiner held the scapulommeter, and slid the plate forward to touch the inferior angle of the scapula. The scale attached to the upper surface of the tool (Figure 1B) indicates mm posterior displacement of the inferior angle of the scapular in relation to the thorax wall (Figure 2). During the test, the subjects remained on standing position, with the shoulder in neutral position, elbow flexed to 90° and the forearm in neutral. A weight of approximately 5% of subject’s body weight was placed on his wrist and maintained by the subjects during the test to induce the winged scapula movement [14,17]. The assessment was bilateral; three alternate measures were taken in each scapula. Two blind evaluators carried out the assessment on the same day, with an interval of five minutes each. To assess the intrarater reliability, the same evaluations were performed with a three days interval (retest). Two experienced and trained evaluators performed the evaluation of the scapular dyskinesis with the scapulommeter.
2.4 Statistical methods
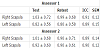
The evaluation of the scapular dyskinesis through observational method showed a concordance rate of 94%, with a Kappa coefficient = 0.88 (IC95%: 0.74 - 1.00). In absolute terms, it was observed classification disagreement only for three subjects, and in these cases, a third assessor was required to reach the final consensus. After all assessments, 26 subjects (52%) were classified with scapular dyskinesis (type I or II) and 24 categorized as control, with no posterior scapular displacement (48%). There were no subjects with type III. Regarding the analysis of the scapulommeter reliability indexes, the results clearly indicated excellent levels of intrarater reliability for both assessors (Table 1).
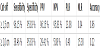
Regarding the interrater reliability of the first evaluation, excellent levels were found for both right and left scapula. Using the method of highest sum of sensitivity and specificity to establish the best cut-off, we found a value of 1.5 cm of posterior displacement as the best cutoff for identifying the presence of posterior scapular displacement, which presented a sum of sensitivity and specificity of 191,98, with area under the ROC curve = 0.98 [95% CI: 0.94 -1.00; p <0.001]. By contrast, the 2.0 cm cut-off pre-set on the literature showed a sum of sensitivity and specificity of 134.29 (Figure 3).
Table 2 shows values of sensitivity, specificity, PPV, NPV, PLR, NLR, and accuracy of each cut-off. There was a substantial improvement of all characteristics using the cut-off suggested by the present study.
3. Discussion
The present study aimed to evaluate the different psychometric characteristics (reliability, sensitivity and specificity) of the linear scapulommeter in order to validate it as an objective tool for assessing of posterior scapular displacement. We also sought to evaluate the cut-off value obtained in this study and then compare it with the value previously defined by Weon et al. [14]. Our data shows that the scapulommeter has excellent reliability values, and the 1.5 cm cut-off showed better sum of sensitivity and specificity and better diagnostic performance than the value used by Weon et al. [14].
Regarding reliability, the scapulommeter reached ICC levels considered excellent, with values above 0.90 and a standard error between 0.12 and 0.15 cm, these results are indicative of good reliability and a low probability of systematic error. Previous studies that analyzed tools that quantify the posterior displacement of the scapula also showed reliability values ranging from good to excellent. Hong et al. [8], for example, found ICC values close to or above 0.90, with a standard error of measurements from 0.15cm to 0.16cm. Strufy et al.[10] found ICC values of 0.72 and standard error measures of 1.7cm. And the scapulommeter proposed by Weon et al.[14] presented values of 0.97 and 0.1cm for reliability and standard error, respectively. However, this study tried to minimize the effects of memory by performing the measurements with a bigger test-retest interval, which was not observed in previous studies. And according to our results, even with a larger interval between measurements, it was possible to achieve excellent reliability values, giving consistency and accuracy for the instrument.
Reliability by itself is not sufficient to assign validity for an instrument. Because it is a tool to determine the presence or absence of scapular dyskinesis, the sensitivity and specificity analysis are both essential for validation [21]. The sensitivity and specificity values may indicate, by calculating the ROC curve, a cut-off point that best represents the value from which we should classify posterior displacement as scapular dyskinesis. According Weon et al.[14], for scapulommeter, a value equal to or greater than 2 cm is able to determine the presence of scapular dyskinesis, however, the study does not mention the criteria for establishing this value. The present study found that the cut-off of 1.5 cm was the best for diagnosing scapular dyskinesis, and on this cut-off we found a better sum of sensitivity and specificity than the one adopted by Weon et al.[14]. Considering that Weon et al.[14] evaluated subjects with anthropometric characteristics similar to the present study, we can say that their classification suggests a falsenegative diagnosis interpretation.
One way to compare the diagnostic ability of these cut-offs is based on the calculation of the positive and negative predictive value, and the positive and negative likelihood ratio. When comparing the values proposed by the two studies, it can be seen that by using the 1.5 cm cut-off, we can diagnose more accurately people who have scapular dyskinesis. The new cut-off demonstrates its potential to minimize the risk of false diagnoses.
Even with great values for reliability, sensitivity and specificity of linear scapulommeter, we have to consider that comparing this tool with an observational technique is a limitation of the study. Although we have tried to minimize the possible assessment errors, by undertaking the tests by expert physiotherapists, the technique remains limited, once it is still a subjective measure. Thus, it is suggested for future studies to replace the observational method for kinematic analysis techniques that can assign better comparisons to the results, like those that describes scapular kinematics in three dimensions [22-25].
In clinical terms, it is important to consider that the current tool, even providing analysis of a single dimension, brings advantages by not requiring costly equipment, maintenance and software for data interpretation. Additionally, this tool does not require the identification of various anatomical points, which reduce the precision, accuracy and reliability of the measures.
4. Conclusion
Scapulommeter is a reliable, valid and easy tool to measure objectively the posterior displacement of the scapula that can serve as an additional technique in the study, diagnosis and monitoring of subjects with scapular dyskinesis, specifically when the 1.5 cm is used as the cut-off value.
Competing Interests
The authors declare that they have no competing interests exists.
Author Contributions
Valéria Mayaly Alves de Oliveira: Acquisition of data, analysis of data
and drafting the manuscript.
Natália Barros Beltrão: Interpretation of data, drafting of manuscript.
Muana Hiandra Pereira dos Passos: Acquisition of data and analysis
of data.
Juliana Pereira da Silva: Acquisition of data and analysis of data.
Ana Carolina Rodarti Pitangui: study conception and design,
interpretation of data, drafting and revising manuscript.
Rodrigo Cappato de Araújo: study conception and design,
interpretation of data, drafting and revising manuscript.