1. Introduction
Allergic disease become noticeable to be rise worldwide, and although an allergic family history is one of the strongest and important risk factors for childhood allergy [1], many international studies [2]. It focus on geographical differences in allergy prevalence, and suggest that environmental influences also play a causal role. Although pets are known to aggravate asthma, allergic rhinitis, and eczema in sensitized individuals [3], controversy remains about whether early life pet exposure is a risk factor or a protective factor in their development. Current guidelines issued in Australia [4], the United States [5], the United Kingdom, and by the Global Initiative for Asthma [6] all agree that there is currently insufficient evidence to provide any recommendations in relation to pet-keeping in early life, the development of asthma and allergic disease because systematic reviews [7], and a meta-analysis have reached different conclusions. Early reviews found pet-keeping increased the risk of sensitization and allergic disease [7] with later reviews finding no effect. A recent meta-analysis [8] reported less risk of childhood asthma associated with cats, but increased risk with dogs. Environmental exposures can either increase or decrease the risk of subsequent allergic disease development [9].
The higher prevalence of food sensitization and food allergy risk categories in participants with asthma, hay fever, and eczema is consistent with other national studies [13]. The link between food allergy and asthma appeared especially strong. There was increased prevalence of all food sensitization and food allergy risk categories in those with diagnosed asthma, as well as increased prevalence and likelihood of FA, those with current asthma [14].
The relationship between FA and asthma severity may or may not be causal in nature. In such as, severe asthma may be associated with greater atopy in general [14]. Moreover, the relationship between FA and asthma severity could be causal, noting that symptoms are induced by foods in people with food allergy up to 30% of the time, although usually with other allergy symptoms [15]. However, FA has been recently found to be a major risk factor for severe asthma and life threatening asthma episodes [14].
Several epidemiologic studies have shown that exposure to environmental factors like tobacco smoking or living in urban areas of industrialized regions, particularly among children living along busy roads and trucking routes are associated with poor respiratory health in children, adversely affect lung function and may increase the risk factor of development of bronchial asthma [16,17].
2. Methods
Design and setting: A cross- sectional study conducted in a random sample. ISAAC phase one (International Study of Asthma and Allergies in Childhood) was used in this study on students in the most polluted area at South of Cairo (Al Oba zone).
Total children aged 11-14 years old ( Range = 4(11-14), mean = 13 ± 0.8 ). Study was done on two different places at the same area with the same pollutions level.
- Number of students with asthma like symptoms = 142
- Number of students without asthma like symptoms = 166
Inclusion criteria: All children are eligible to be included in this study.
Exclusion criteria: No exclusion criteria accept a questionnaire that is not completed or if a questionnaire contains double answer for example the students answer by yes and no in the same question or refused to participate accordingly.
ISAAC questionnaire was adapted, translated into Arabic and it used to be included socio-demographic data and environmental exposure factors.
3. Statistics
All data in this study are collected, coded, tabulated and statistically analyzed using SPSS program for windows version 14 (SPSS Inc, Chicago II). Comparative studies were done for numerical data using student’s t-test and were done for categorical data by Chi-square test for comparison between variable, and it was done to estimate the relation between risk factors and development of asthma.
The level of significance was taken at p value < 0.05.
Asthma symptoms: In this study we estimated asthma like symptoms on basis of positive answers to written question (have you had wheezing or whistling in the chest in last 12 months?).
Allergic Rhinitis: In this study, allergic rhinitis was considered on the basis of positive answer to written question (have you had repeated attacks of sneezing, runny or blocked or itching in the nose when you did not have a cold of flu?).
Atopic Dermatitis: In the study, atopic dermatitis was considered on the basis of positive answers to written question (have you had repeated attacks of itchy rash ?).
4. Results
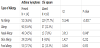
315 of children with mean age of 12.5 years were evaluated for asthma, allergic rhinitis and atopic eczema prevalence and their associated factors. Frequency distribution of children according to presence or absence of asthma symptoms were 142 and 166 respectively (Table 1).
:it shows the distribution of children with and without asthma symptoms as regard to presence and absence of allergy, where this table showed a statistical significant higher % of children with allergy in children with asthma symptoms compared to those with no asthma symptoms. Nasal allergy was the most predominant form of allergy ( P value = 0.05).
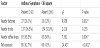
According to environmental exposure of children, higher percentage of children with asthma symptoms lives nearby factories, nearby coffee shop and higher percentage of them living nearby or exposed to pets as (table 2) showing below ( P value = 0.05).
There is a statistical significant different between children with and without asthma symptoms as regard family history. As higher percent of children with asthma symptoms has positive family history (Figure 1).
There was a significant association between risk factors like environmental factors or host factors and development of asthma symptoms and other allergic diseases like eczema or allergic rhinitis.
5. Discussion
This study was carried out to assess the risk factors and prevalence of asthma like symptoms and other allergic diseases like allergic rhinitis, and atopic dermatitis among Egyptian school children in the south of Cairo (Al Oba zone) on aged group range 11-14 years.
Exposure to allergens were significantly associated with sensitization of children with asthma symptoms rather than children without asthma symptoms (63.4% and 22.3% respectively, P value = < 0.001*). Nasal allergy was significant between them, whereas, there are not a statistical significant as regard to skin and food allergy (P value = 0.232 and 0.953 respectively).
This study found that the relation among exposure to nearby factories, nearby coffee shops and development of asthma symptoms were 26.1% and 65.5% respectively, and these percentage were a significant difference of children with asthma symptoms compared to others without asthma symptoms ( P value = 0.002* and 0.006*). Moreover, pets exposure are a significant difference between children with or without asthma symptoms (P value= < 0.001*). [18] found the prevalence of asthma symptoms was significantly more common in families with animal in their home compared to others with no exposure to animal.
In this study we followed the family history of the studied sample as regards atopy, where we found that 47.9% of children with asthma symptoms had positive a family history of atopic diseases compared to 52.1% with had negative a family history.[19], found that the presence of asthma cases aggregation among related individual may indicate either shared genes or a common household environment.
6. Conclusion
A significant association between allergy exposure and development of asthma symptoms and other allergic diseases especially early exposure to these factors during childhood. Despite advances in therapy, prevalence of like this allergy is still increasing.
Competing Interests
The authors have no competing interests with the work presented in this manuscript.