1. Introduction
Prostate cancer represents the second most common cancer in men (14%) and is the sixth cause of cancer-related death (6%) in worldwide [1]. Death rates for prostate cancer have been decreasing in many developed countries, including Australia, Canada, the United Kingdom, the United States, Italy, and Norway in part because of the improved treatment with curative intent [2-4]. For men with advanced prostate cancer, testosterone suppression – most often achieved by the administration of a gonadotropin hormone-releasing hormone (GnRH) analog – remains the mainstay of treatment [5-8]. In fact, approximately 90% of prostate cancer tumors respond to initial androgen deprivation, thereby improving patients’ quality of life and longevity [9]. The administration of GnRH analogs, Leuprorelin and Triptorelin, is the preferred choice for the treatment of prostate cancer [10-13]. The injection of Leuprorelin or Triptorelin reduces testosterone serum level near surgically castrated [14-17]. For this two drugs have been demonstrated to have comparable tolerability as monthly such as quarterly administration [18,19]. The development of depot formulations, 1-3 and six months was made to improve the patient’s compliance with same drug safety and tolerability [20]. The loss of medication adherence is a global problem that affects the clinical outcome and economic health [21,22]. No studies in literature describe and estimate medication adherence and persistence of Leuprorelin and Triptorelin in the prostate cancer. Leuprorelin can be administrated monthly and quarterly at the concentration of 3.75mg - 11.25mg and 7.5mg and 22.5mg, respectively, while Triptorelin is available in dosage monthly of 3.75mg and quarterly of 11.25mg. In this study we took in consideration only Leuprorelin 3.75mg and 11.25mg and Triptorelin 3.75mg and 11.25mg, these two formulations regard the majority of patients with prostate cancer, Leuprorelin 7.5mg and 22.5mg is used by a limited number of patients, so little that our statistical analyses was impossible. Other formulations of Leuprorelin and Triptorelin (like 6 months depot) are unavailable in Italy. The aim of the study is to evaluate the medication adherence and persistence of patients with prostate cancer who used Leuprorelin and Triptorelin and, on the basis of adherence and real use in clinical practice; we have made an economic evaluation.
2. Medication Adherence
Patient adherence has been defined by the World Health Organization (WHO) before and by The International Society for Pharmacoeconomics and Outcomes Research (ISPOR) later as “the extent to which a person’s behavior in taking medication corresponds to recommendations given by a health care provider and which that individual has agreed upon”. [23,24] This definition was been completed as “the extent to which a patient participates in a treatment regimen after he or she agrees to that regimen.” [25,26] In publication several methods are reported to calculate the adherence to treatment such as Continuous Measure of Medication Acquisition (CMA) [27-29]; Medication Possession Ratio (MPR) [30-33]; Medication Refill Adherence (MRA) [34-36]; Proportion of Days Covered (PDC) [37- 39]; Refill Compliance Rate (RCR) [40-42]; Medication Possession Ratio, modified (MPRm) [43-45]; Dates Between Fills Adherence Rate (DBR); Compliance Rate (CR); Continuous Multiple Interval Measure of Oversupply (CMOS); Continuous Measure of Medication Gaps (CMG); Continuous, Single Interval Measure of Medication Acquisition (CSA) [46]; and Received Daily Dose/Prescribed Daily Dose [47]. Only the last method consider the Prescribed Dose and not the Defined Dose, approaching most of all to the WHO definition, that take in consideration the treatment regimen prescribed by physician. The medication adherence can be calculated efficiently by taking into account the intention-to-treat analysis of the physician (PDD) and the behavior of the patient (RDD) on the basis of the prescription.
3. Medication Persistence
The medication persistence can be defined as the length of time from initiation to discontinuation of the therapy, measured by time in days [48]. Practically the non-persistence is measured like the days that elapsing between the first and the last refill, plus the days of treatment supplied by the last refill, minus the days of non-persistence, that is the days of difference between the days of treatment prescribed and the days of treatment really made (between two next refill). Calculation of adherence and non-persistence is possible because the only centre of dispensation of GnRH is the hospital pharmacy, so every refill could be registered by hospital pharmacists and the data inserted in the software.
4. Materials and Methods
This retrospective observational and economical study was carried out from 1st January 2007 to 31st December 2012 in the Hospital Pharmacy of Pescara (Italy). The study design was approved by ethics committee of the Pescara Hospital. The written consents were not given by the patients for their personal information because this is an observational retrospective study as regulated by the Italian Drugs Agency with the "Guidelines for the classification and management of observational studies on drugs, as described in the guidelines available on the website "agenziafarmaco.gov.it". In the case of studies that do not involve a direct relationship with the patient, it is not necessary to give the privacy consent form to the patient. The analyzed data was related to the pharmacy refill: drug used and what it is used for (as prescribed by the physician), data and dose of every refill, Defined Daily Dose (when present) (DDD); all these data were inserted by pharmacists in the software produced ad hoc, this software is a simple Microsoft Access based software able to calculate the PDD and RDD from inserted data. Go to see the parameters we have considered: the DDD is the assumed average maintenance dose per day for a drug used for its main indication in adults. [49]; PDD is the intention to treat, the dose that physician prescribes, it is calculated automatically dividing the prescribed dose by physician for the days of treatment, in our example the software will calculate automatically the PDD dividing 3.75mg of Leuprorelin or Triptorelin for 28 days (0.134mg per day), for other medicines the PDD could change, for Triptorelin and Leuprorelin only 3.75mg every 28 days and 11.25mg every 90 days represent a labeled use, than PDD doesn’t change in time; RDD is the dose per day that patient has received in pharmacy refill, it’s calculated dividing the dose given by pharmacist in refill, for the days that elapses until the next refill, for example if patient back in pharmacy for refill 40 days after first refill, than RDD will be 3.75mg/40days (0.094 mg per day), well as if patient back after 20 days RDD will be 3.75mg/20days (0.18 mg per day), we calculate RDD like weighted average of all RDD for every interval of days between consecutive refills:
In this study we resort to weighted average because intervals between each refill could be different, while we want to reckon an exact value for the real use of the drug for each single patient, for each treatment day (i.e. a shorter interval, e.g. 5 days, cannot be regarded as a longer one of 40 days, they do have a different weight on the final result). It is very simple to reckon weighted average using Excel program, using sum product function.PDD and RDD correspond perfectly if patient back to refill precisely when prescribed by physician, in this case after 28 days for Leuprorelin and Triptorelin 3.75mg, 90 days for Leuprorelin and Triptorelin 11.25mg, for this situation the medication adherence is 1, the best value, the loss of medication adherence is indicated for values less than one; in fact the equation used for the calculation of the medication adherence is as follows:
All data was analyzed anonymously. Each patient was identified with a personal number. Patients were aware that their data was stored in a specific database, but were not informed that this data was used for research purposes. This procedure has been disclosed to the Ethics Committee who, in accordance with national legislation, approved it. Every patient in continuous therapy with Leuprorelin 3.75mg and 11.25mg and Triptorelin 3.75mg and 11.25mg for Prostate Cancer from 2007 to 2012 was included in the study.Drug persistence with therapy was calculated for single patient as the total days between first and last refill of drugs, plus the days of treatment supplied by the last refill, minus the days of non-persistence.We estimate the total days of treatment summing all the intervals of drug refills and adding also the days supplied by the last refill, obtained dividing the last dose refilled in the hospital pharmacy by the last prescribed dose.
For Persistence, we consider the effective days in which the patient has taken drug, deducting from persistence NPD (Non Persistence Days) on the basis of Prescribed Dose.
Interval 1: time in days that elapses between first and second refill. So the medication persistence is calculated as:
For the calculation of persistence with medication for 4 years only patients that have started the therapy before 31 December 2007; all the patients that have started after haven’t the possibility to make at least four years of therapy to 31 December 2011.The economic assessment is based on the cost per mg of Triptorelin and Leuprorelin for the hospital, and then multiplying this value to the RDD found for both drugs.
5. Results
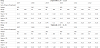
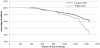
The number of patients and their age, as median and range, from 2007 to 2012 was summarized in table 1. The numbers of patients enrolled in the study varies from a minimum of 55 in the 2007 to a maximum of 206 in the 2012 for Leuprorelin 3.75-11.25 mg while for Triptorelin the numbers of patients was 52 in the 2007 and 150 in the 2012. The median age of patients was 80 years old for both drugs. The persistence of treatment describes the days in which the patients are covered by pharmacological therapy: it was of 360 days for Leuprorelin in each years of analysis, and it changed from a minimum of 270 to a maximum of 360 for Triptorelin. The medication adherence, calculated as ratio between RDD and PDD, changed from 0.92 to 0.97 for Leuprorelin describing a loss of adherence from 3% and 8% while for Triptorelin the values of adherence varied from a range of 0.93 to 1.00 with a loss of adherence of 7%. (Table 2) The medication persistence calculated for 4 years was of 79% for Leuprorelin and 62% for Triptorelin with a percentage of difference between the two drugs of 17%, (Figure 1). From statistic point of view, two curves are the same (p=0.05; ?2=3.086). The cost per day of the therapy (cost per RDD) for Leuprorelin was € 2.24 and € 2.84 for Triptorelin. According to this data, one year of treatment with Leuprorelin per patient costed € 744.30 and € 989.31 for Triptorelin.
6. Discussion
In the treatment of prostate cancer the use of GnRH analogues, as Leuprorelin and Triptorelin, it must be continued for a long time. In this way it is very important that the patients follow the indications of the physicians to became adherent to the treatment. The loss of adherence could be representing a cause of non-response to the therapy and a consequent increase of the cost for the economic healthy resource. In the case of treatment of prostate cancer with Leuprorelin and Triptorelin, the patients were adherent to treatment in all years studied, from 2007 to 2012. The analysis of persistence has shown a loss of patients of 21% for Leuprorelin and 38% for Triptorelin for a 4 years study. From an economic point of view it is important to carry out a study based on real-life to find out the real cost of drug in function of the real dose taken by the patient. In this study the RDD was calculated as the indicator of quality of drug-consumption and then to make a pharmacoeconomic analysis. From the cost per RDD the Leuprorelin has a minor cost per patient per years than Triptorelin. The medication adherence data were very good considering the old age of the patients: it shows that the age factor does not affect the therapy. Also the length of the treatment does not decrease the medication adherence. This evidence is supported by the constant check-up of the patient by the specialist that renew the treatment once per year, in fact in Italy this drugs can be annually prescribed only by a specialist in urology or oncology, with the redaction of a specific therapeutic plan, and, on this basis, the family doctor can prescribe.
7. Conclusion
The data collected during this study show that the two drugs are similar in terms of medication adherence and persistence; the cost per day for Leuprorelin is lower than the one for Triptorelin. It would be really interesting to correlate adherence, persistence and costs with clinical outcomes, in fact this study would be an introduction to a new kind of calculation adherence and related costs per RDD. With a greater number of patients and with a multicentric analysis it would be possible make economic evaluations on a large scale, and the results could be considered for health care decisions with economic data to renegotiate the drug price.