1. Introduction
Cardiovascular disease (CVD) is the single largest killer of women, [1] and more women than men die each year despite advancements in life-saving therapies [2]. In fact, patients with a total blood cholesterol level greater than 200 mg/dL have a two-fold risk of developing CVD [3]. 3-Hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase inhibitors (statins) are currently the most effective treatment for lowering total cholesterol (TC), calculated low density lipoprotein (LDL-C), and CVD risk [4].
Despite diagnosis and treatment in women, CVD death reduction has not matched that of men [5]. Women have less compliance to statin medication than men [6]. Poor adherence to statins may be related to medication costs and side effects. In randomized clinical trials, myalgias are reported in 1% to 5% of patients in statin and placebo groups; [7] however, observational data with non-selected patients show higher rates of myalgias up to 20% [8]. We tested a nurse practitioner (NP) guided protocol which is aimed at reducing TC and LDL-C in women with prior statin intolerance due to myalgias.
2. Methods
The Barbra Streisand Women’s Heart Center at the Cedars-Sinai Heart Institute is a tertiary chest pain center where we recruited 15 consecutive women with a medical indication for statin therapy and a history of myalgias. For patients with multiple baseline TC and LDL-C measurements in chart review, the highest prior LDL-C was selected. Myalgic pain was defined as benign, moderate to severe myopathic symptoms such as: myalgia, myositis and myopathy but not rhabdomyolysis, based on the ACC/AHA/NHLBI guidelines [8]. Clinician interview determined if the patient’s pain was myopathic pain related to statin use. Other etiologies of myopathic pain were ruled out at the patient’s clinical visit.The study was approved by the Cedars-Sinai Medical Center ethical review board.
We defined statin intolerance as the inability to tolerate daily dosing of at least one prior statin. Our novel NP protocol for alternate dosing statin regimen used pravastatin, atorvastatin or rosuvastatin for the reduction of TC and LDL-C, selected by individualized statin and dosing depending on the patient’s medication formulary, need for LDL reduction and the Cytochrome (CYP) pathway to avoid medication interactions.
Patients were initially started on twice weekly statin dosing on Mondays and Thursdays for 4 weeks then titrated up one additional dose per week as tolerated until either daily dosing was achieved or the patient experiences myalgic pain. If myalgias developed, the patient was taken back to the immediately prior tolerated dosing regimen. Fasting baseline and follow-up lipid levels were obtained by chart review.
2.1 Ethics statement
All patients were informed of the study and provided a written informed consent. The Cedars-Sinai Institutional Review Board (CSMC IRB) approved the study (CR00006479/Pro0019454). The investigation conforms to the principles outlined in the Declaration of Helsinki.
2.2 Statistical analysis
All statistical analysis was performed using SAS (ver. 9.2; The SAS Institute, Cary, NC). Means and standard deviations (SD) were reported for all continuous variables. Wilcoxon signed rank test was performed on the data.
3. Results
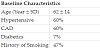
We evaluated and treated 15 consecutive female patients with a mean age of 62 ± 14 years (Table 1). Prior to initiating the alternate dosing NP protocol, 93% were intolerant to 2 or more statins (simvastatin, pravastatin, atorvastatin, or rosuvastatin) with associated myalgias.
In the NP alternate dosing statin protocol, the most common regimen was rosuvastatin 5 mg with twice weekly dosing, Mondays and Thursdays (Figure 1). These patients were not able to increase their days of the week after 4 weeks and maintained a twice weekly regimen. Three of fifteen (20%) patients needed to reduce their regimen to once weekly dosing. The remaining 6 patients were able to progress to 3-4 day per week dosing with either atorvastatin or rosuvastatin (Figure 1). One patient was taking rosuvastatin 5 mg with three days per week dosing which included Mondays, Wednesdays and Fridays. She needed to take an every-other week drug holiday to avoid severe myalgias. Patients were followed up 4-6 weeks after the initiation of the NP protocol.
Utilizing the alternate dosing NP protocol, we observed significant reductions in TC and LDL-C compared to their prior highest TC and LDL-C (Figure 2).
4. Discussion
Among women with a history of daily dose statin intolerance, an NP guided protocol is effective for reducing TC and LDL-C levels. This pilot study is the first to evaluate 3 different statins with multiple alternate dosing regimens. Although different statins have different LDL-C lowering capabilities, this study suggests that an alternate statin regimen may be superior to no statin for lowering TC and LDL-C. The data would further suggest that our NP alternate dosing protocol may be an effective strategy and should be considered before classifying a patient as statin intolerant.
Our results are consistent with previous studies and support the hypothesis that alternate statin dosing is a successful strategy for treating prior statin intolerant patients. Our most common regimen was rosuvastatin 5mg with twice weekly dosing, Mondays and Thursdays. Rosuvastatin alternate day dosing is desirable because of its generous half-life of 19 hours [9] and its potent LDL-C lowering capabilities. Gardarla, Kearns and Thompson [10] published similar results when they evaluated 40 patients with prior statin myalgias who were placed on twice weekly rosuvastatin (5 mg and 10 mg) either alone or in addition to other lipid-lowering agents. They showed an LDL-C reduction of 26% and TC reduction of 19%, which is similar to our results [10]. Backes et al performed a retrospective analysis on patients taking rosuvastatin (2.5 mg, 5 mg, 10 mg) in 51 patients. Their mean LDL-C decreased by 34.5% on an average dose of rosuvastatin 5.6 mg per mg/dl which also correlates with our findings [11]. In addition, once-a-week dosing using rosuvastatin (2.5 mg-20 mg) also appears to be beneficial. Ruisinger et al. demonstrated a 23% reduction in LDL-C and 17% reduction in TC during a mean follow up of 4 months [12]. Their results are also consistent with our data in which 3/15 (20%) tolerated only the once-weekly regimens.
The Alternate Day Versus Daily dosing of Atorvastatin Study showed similar results with atorvastatin (10-20 mg) alternate day dosing compared to daily dosing. This double blind, placebo-controlled design evaluated 35 patients who met National Cholesterol Education Program (NCEP) Adult Treatment Panel (ATP) III guidelines for statin therapy. Although higher doses were used on alternate day, their results suggest that alternate dosing can produce similar reduction in LDL-C comparable to that of daily administration of atorvastatin [13].
5. Limitations
There are several limitations to this pilot study. Our data is observational and not prospectively obtained, without placebo controls or blinding. Lipid levels were not standardized to timing and myalgias were based on patient report and/ or clinical chart review. Furthermore, the sample size is small. Nevertheless, there is association among the percentage of TC and LDL-C lipid lowering and statin dosing. There was also bias in the selection of the TC and LDL-C with selecting the prior highest result. A larger prospective and placebo controlled trial would be needed to evaluate if an NP guided alternate dosing protocol could truly alter cardiovascular outcomes through cholesterol lowering.
6. Conclusion
Among women with a history of daily dose statin intolerance, an NP alternate dosing protocol is effective in reducing TC and LDL-C levels. Further studies using this NP alternative statin dosing protocol are warranted in larger populations who are statin intolerant to determine whether an alternate dosing protocol leads to increased longer term statin adherence and whether this impacts the rates of cardiovascular disease outcomes in women.
7. Implications for Practice
This alternate statin dosing protocol for higher risk patients who are intolerant to normal statin dosing due to complications and sideeffects may:
- Lower TC and LDL-C
- Help to reduce myalgic pain in women with statin intolerance
- Provide an alternative treatment than not implementing any statin use.
Competing Interests
The authors declare that they have no competing interests.