1. Introduction
Asthma is a major public health problem and one of the most common chronic conditions in the world. According to the Global Burden of Disease Study, asthma caused more than 345,000 deaths worldwide in 2010 [1]. In Europe alone, asthma affects 30 million people and the cost of asthma care in Europe is estimated at £18 billion per year; lost productivity accounts for almost £10 billion of this [1]. The second half of the 20th century was marked by a disturbing increase in frequency of allergic diseases, affecting approximately 20 percent of the global population, and the rate of bronchial asthma amongst adults is 5.4 percent (4.9% in men and 5.8% in women) [2]. Epidemiological studies in Saudi Arabia revealed an increasing prevalence of asthma in the past three decades, which may be attributed to the rapid lifestyle changes related to the modernization of Saudi society, changes in dietary habits, and exposure to environmental factors such as indoor allergens, dust, sand storms, and tobacco [3]. Asthma, a common chronic disorder of the airways in Saudi Arabia affecting more than 2 million Saudis, ranks19th in terms of disability-adjusted life years [4].
Asthma had an enormous impact on patient's wellbeing [5], despite the availability of effective treatments and evidencebased management guidelines [6]. Asthma can result in physical, emotional, and social limitations that can impair patients’ quality oflife [7]. There is a growing burden of asthma in terms of morbidity, quality of life, and health care costs, therefore health care providers should play a pivotal role in improving quality of care for asthmatic patients [8].
Asthma, as an allergic disease, is characterized by airway hyperresponsiveness (AHR) that leads to intermittent and usually reversible airway obstruction [9]. Although new mechanisms of treatment have been discovered and the effects of bronchial asthma treatment have significantly improved, asthma control in clinical practice is suboptimal in many cases [10-12]. The concept of asthma control includes clinical and functional manifestations, such as symptoms, nocturnal awakenings, use of rescue medication, activity limitation, and pulmonary function [7].
The achievement and the maintenance of asthma control is currently considered the main goal of asthma treatment [13]. Al-Zahrani et al. [14]; Marchioro et al. [15] contended that in accordance with the established international criteria, asthma is uncontrolled in the vast majority of asthma patients. Consistently, a recent asthma control survey showed that only 5% of patients were controlled, 31% were partially controlled, and 64% were uncontrolled [16]. Al-Zahrani, et al. [14] have been attributed this to certain risk factors, which included: inappropriate use of the inhaler device, active smoking, passive smoking, unsealed mattress, and workplace triggers were also associated with uncontrolled asthma.
Poor asthma control is associated with increased risk of exacerbations, debilitation, impaired quality of life, increased healthcare utilization and reduced productivity [10,11,17]. The degree of asthma control appears to have a significant impact on health-related quality of life [7]. Therefore, in clinical practice, correct assessment of asthma control facilitates the clinical management of patients, given that asthma treatment progression is based primarily on the level of asthma control [18].
On the other hand, progress in understanding mechanisms and effective treatment, there are still therapeutic failures in patients treated for bronchial asthma. Many observations have shown that the effects will not improve unless patient education and cooperation become the element of the treatment process [12]. Al-Muhsen et al. [19] reported that most patients had poor knowledge about asthma and were using medications improperly, suggesting inefficient application of management plan. Yun and Cho [20] added that factors hampering patients’ efforts to reduce the burden of asthma include lack of information, under-use of self-management, over-reliance on acute care and use of alternative unproven therapies.
Denial of having a chronic condition, insufficient knowledge of the disease process [21] and lack of adherence to standard treatment [15,22] are often considered to be important factors that increase morbidity in asthma [23]. Marchioro et al. [15] revealed that poor treatment compliance was related to the fact that most patients were not informed of or did not understand the importance of maintenance treatment of asthma and this demonstrates that greater educational intervention is needed to resolve patient uncertainties about the safety of the medication, it’s possible side effects, and long-term benefits.
Therefore education is vital in the therapeutic process and patient education has become a key component of asthma management for patients at all age groups [24]. It improves the control of the disease at the individual level by influencing the adherence and compliance [25]. Asthma education is among key-recommendations of all recent guidelines on asthma management but it is still too infrequently provided. Although, numerous studies worldwide have evaluated the impact of patient education, there is still a lack of well designed, theory and evidence based interventions that focus on improving asthmatic patients’ control of their disease process. Specifically, patient selfregulation training is getting a momentum for increasing patients' knowledge among patients with chronic illnesses.
Management of chronic health problems through lifestyle changes often requires evidence-based, intensive interventions to set up new health behaviors through successive self-regulation skills so that conditions are reversed and the behaviors are sustained [26]. Asthma care based on guideline recommendations leads to well-controlled asthma in the majority of patients.
Self management requires that the person understands the illness and actively participate in the treatment process, including taking medications, participating in decision-making regarding their illness to manage the impact of the chronic illness on their daily life, maintain their general health and avoid risk factors for other illnesses [27]. The latest findings suggest that health providers-patient partnership, mutual understanding and well-discussed treatment plan that is evidence-based significantly improves the course and control of the disease [12]. However, international publications revealed that many patients actually do not receive evidence-based care [28].
Warwick et al. [29] contended that as self-management and symptom monitoring ensure better outcomes; health professionals should encourage these behaviours. Self-regulation is the means by which people learn how to manage disease utilizing internal resources and external factors. Self-regulation as it relates to asthma entails the ability to observe, make judgments about the observations, try out change strategies to improve management, and react appropriately to the change effort [30]. Clearly; physical and clinical manifestations of asthma must be understood to allow the patient to make sense of how to manage them. Effective interventions need to widen the patients' perspective regarding these influences and build their skills of selfregulation as they relate to effectively completing a range of varied and complex management tasks [31].
Very few data however are available to assess self-regulation interventions focused on asthmatic patients, therefore current study sought to test the hypothesis that patient self-regulation training would increase patients' knowledge of asthma, which in turn will result in better control of asthma. Consequently; the researchers initiated this research study to develop and evaluate such an intervention.
2. Conceptual Framework: Self-regulation Model of Illness
Effectively treating chronic diseases through health behavior changes often require intensive theory- and evidence-based intervention [31]. Hustad et al. [32] viewed self-regulation (SR) as the effortful ability to plan and achieve delayed adaptive outcomes through goal-directed behavior, and this skill may play a role in adaptive behavioral change. According to SR theory, individuals use a goal-guidance process, wherein, self-regulation cognitions (e.g. selfefficacy expectations), emotions and skills (e.g. self-monitoring and feedback), play an important role in goal setting, active goal pursuit and goal attainment [33,34]. Maes and Karoly [34] emphasized a set of guidelines for interventions based on their review of a number of selfregulation strategies associated with behavior change. Among these self-regulation core processes are: realistic outcome expectations; illness representations; goal setting; planning; progress evaluation and feedback; efficacy support; attention and emotion control; selfmonitoring; goal reformulation; relapse prevention and anticipatory coping.
Intrapersonal factors, as beliefs and feelings, are less important in control of asthma than having self-regulation skills. One of the main intervention techniques using self-regulation principles is motivational interviewing. Cornforth [35] emphasized that the most important principle for effective care and promotion of selfmanagement is the ongoing collaboration, education and patientcentered support through a partnership with health professionals who have specialist disease knowledge and training. Cornforth [35] also contended that health professionals need to be aware of the many diverse and unpredictable complexities of the disease, and of the many internal and external factors that may affect a patient’s ability to regulate their own health and well being. The author further added that the attitude, behaviour and skills of health professionals can have a significant effect on the extent to which patients feel engaged and supported in their self management. This could facilitate a fuller understanding of the challenges faced by patients and their significant others, and encourage clinicians to make time to learn about patients’ circumstances, experiences and interpretations in order to encourage unity in goal setting, which should improve the overall patient experience.
Self-regulation Model of Illness (SRMI) provides a framework for understanding how individual symptoms and emotions experienced during a health threat or diagnosis influence perception of illness and guide subsequent coping behavior. The SRMI theory suggests that individuals search to understand their illness threat by developing an understanding of what the illness is, its causes, its consequences, and whether it can be cured or controlled [36]. This understanding formulated from personal experience (physical symptoms and emotions), social influences, and/or interaction with healthcare providers. Individuals are thought to reduce their health risk or change their health behavior in ways consistent with their own illness representation [36].
Finally, SR theory holds that individuals with low generalized selfregulatory capacity will be less capable of developing adaptive goals and monitoring their current status toward those goals than individuals with higher self-regulatory capacities. Furthermore, individuals with lower self-regulatory capacities will prefer activities that provide immediate gratification [32]. It holds promise for enabling individuals to make optimum their control of chronic disease.
There is a lack of well designed, theory and evidence based interventions that focus on asthma control among adults. Such an intervention should be able to reach a large group of adult patients and has to take the large differences between people in their behaviours, preferences and capabilities into account. Therefore, individualized intervention approaches are needed to successfully modify illness behaviours. Although based on the empirical literature, research on SRT in the domain of asthma control is still in its early stages and more research is clearly needed hence, there was a pressing need for conducting an intervention study to provide evidence for its impact among asthmatic patients.
We initiated the current study in an effort to develop and evaluate a comprehensive self-regulation program for Saudi patients suffering from chronic asthma that addresses their particular needs and cultural context, with the main objective of evaluating the efficacy of the program in improving asthma knowledge and symptom control.
3. Material and Methods
3.1 Aim of the study
The aim of the present study was three- folds: the first was to assess patients' knowledge related to managing their asthma condition. The second was to develop an evidence based self-regulation intervention that is based on the patients’ assessed educational needs, and finally implementation of the intervention and evaluation of its impact on patients’ knowledge as well as asthma control.
3.2 Subjects and methods
Research design: A quasi- experimental research design was utilized in the current study. The study group participants acted as their own control where their posttests compared to the pretest scores.
The study variables: The independent variable in this study was the designed evidence-based self-regulation program while the dependent variables were: the patients’ knowledge and asthma control.
Setting: The study was conducted at King Fahd Hospital, Kingdom of Saudi Arabia.
Study Participants: A convenient sample of 30 patients with a main complaint of uncontrolled asthma diagnosed as moderate to severe condition by a physician of at least six months duration were recruited for the study. Inclusion criteria were: meeting the operationalized criteria for uncontrolled asthma; had to be 18 years and older were on an inhaler for managing asthma, willing to attend the training.
In order to be included in the analyses, patients had to complete all assessment time points (pre, immediate and 2-month follow up) and the attendance of all program training sessions.
Patients excluded if they had: (1) previously attended asthma counseling and (2) complained a significant co-morbidity (e.g. heart disease, diabetes mellitus with complications, stroke and renal problems).
Study tools: Data pertinent to the study were collected utilizing the following three tools:
Tool I: Socio-demographic data sheet. This was developed by the researchers to collect data pertinent to patient’s age, marital status, gender, education occupation and previous training on asthma management.
Tool II: Pre/post asthma knowledge test, developed by Baez Saldaña et al. [37], was used to evaluate patients’ knowledge about asthma self regulation at baseline, immediately after implementation of the intervention protocol and at 2-month follow up. It consists of 20 multiple choice type questions offered to patients through structured interview by the researchers.
Scoring system for Pre/post knowledge test (tool II): the questionnaire included 20 questions in three domains: nature of the disease and triggering factors (3 questions), asthma treatment (9 questions) asthma self-regulation (8 questions). All questions had trichotomous response options (true/false/do not knows). The total score was the number of items in the total instrument that were correctly scored (each right answer was given a score of 1; the total score was 20 scores).
The face and content validity of these questions was established by consensus of a panel of asthma expert. The questionnaire is reliable and is very sensitive to change. This instrument is useful for measuring the knowledge that asthmatic patients have of their disease in clinical practice and investigation [37]. A median sensitivity, measured as percentage change of 67% is reported which could indirectly, assess the extent of learning that happened.
Tool III: Asthma control questionnaire (ACQ) developed by Juniper, et al. [38] was specifically prepared to measure asthma control in adults aged 17 or older. It has already been translated and culturally adapted to several languages; including Arabic language. The permission to use the Arabic translated version of the questionnaire was obtained from Juniper being the primary author. The ACQ comprises six questions. Five questions refer to asthma symptoms (nocturnal symptoms, morning symptoms, limitations to daily activities, dyspnea and wheezing) with one question about daily rescue therapy use (β2agonist). Patients were asked to recall how their symptoms and bronchodilator use had been during the previous week and to respond to questions on a 7-point scale (0=no impairment, 6= maximum impairment). The final score of the questionnaire is the average score of the answers chosen by the patient, which can range from 0 (totally controlled) to 6 points (not controlled)[23].
The ACQ is able to identify the adequacy of asthma control in individual patients. In general, patients with a score below 1.0 will have adequately controlled asthma and above 1.0 their asthma will not be well controlled. On the 7-point scale of the ACQ, a change or difference in score of 0.5 is the smallest that can be considered clinically important [23].
It is a widely available and validated instrument with strong evaluative properties to measure asthma control in patients [23]. Reliability using Cronbach’s alpha in patients with asthma was 0.82 [39]. ACQ has great capability to discriminate individuals with uncontrolled asthma from those with controlled asthma, and therefore presents good reproducibility and responsiveness [40].
4. Procedure
Preparatory Phase: This stage focused primarily on the development of the study program and adoption of the study tools.
Based on the empirical literature on the self regulation (SR) theory of behaviour change, we developed the study program for patients suffering from chronic uncontrolled asthma with a main focus on the training of self-regulation skills. The program aimed at improving patients’ knowledge of the disease process and promoting their asthma control through self regulation training. The self regulation covered the following topics: knowledge of asthma disease, its pathophysiology, asthma triggers, and methods of control and avoidance of triggers, medications, types of inhalers, inhalator technique, and spirometry, self-management of asthma symptoms. Program also included extensive training on effective use of inhalers and its accessories, storage and precautions.
Self regulation is viewed as an important dimension of the social cognitive theory which comprised three elements including observation (warning signs and symptom improvement), judgment (potential triggers in environment, changes in environment) and reaction (keep symptoms from getting worse, follow the selfregulation program).
Implementation and Evaluation Phase: An official permission was obtained from the director of King Fahd Hospital to conduct the study. Consent was thereafter granted from the patients before proceeding with the study. Study participants were informed of the purpose of the study, and they were ensured about their right to withdraw, right for protecting their data and protection from harm.
Following recruitment and provision of informed consent, patients were then interviewed and baseline data were collected. The interviews usually lasted 30 min. Participants socio-demographic as well as baseline data for knowledge and asthma control were obtained. Patients were then divided into small groups of 2-3 participants for explanation of the protocol and discussion of how the self-regulation intervention will be implemented. The intervention was carried out over 6 sessions, for each group of patients. The duration of each session ranged from 20- 30 minutes.
The researcher relied extensively on instilling motives on the study group to ensure that they strive to achieve desired objectives and avoid unpleasant states. This approach adopted from selfregulation theories which target at enlightening participants of the discrepancy between a desired future state and present state to ensure their adherence to the self-management as well as treatment plans. According to self-regulation, motivation should precede planning and execution of efforts to achieve the goal. Moreover, cognitive and emotional processes are considered magnificent yet interrelated mechanisms contributing to human motivation. Therefore the program basically depends on promoting knowledge and instilling motivation for achieving control of the disease process. Participants were also involved in cyclical appraisal of outcomes feeds back to previous state/condition.
Training was further individualized according to patients needs to ensure their understanding and facilitate discussion and reflections from their experiences. Lecturing, discussion, demonstration and re-demonstration were the main teaching methods throughout the program.
A booklet which covers main theoretical background information on asthma was developed for the purpose of the study. This booklet was used as teaching aids and a reminder for patients to facilitate internalization of learning.
Since the main objective of the study was to evaluate the efficacy of the program in promoting knowledge and control of asthmatic patients, the impact of the program was evaluated immediately after program implementation as well as at 2 months follow-up.
Data Management Phase: Data were analyzed using SPSS version 20. The following tests were carried out: frequency and percentage distributions, means and standard deviations, correlation coefficient, ANOVA for comparison of means.
5. Results
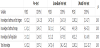
Table 1 shows the socio-demographic profile of the 30 subjects in the study. The highest percentage of participants had age range between 31 to 40 years (70%), were females (70%), illiterate (46.7%). Majority of participants were married (66.7%). Almost all participants were insured and did not receive any previous training on asthma.
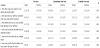
Participants baseline knowledge was not satisfactory as revealed by multivariate ANOVA analysis (table 2). Total knowledge score, knowledge of the disease and its triggers, therapy as well as selfregulation has significantly improved immediately post program. There was also a significant retention of knowledge after 2 months of the program implementation (table 2).
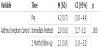
Asthmatic participants have shown significant satisfactory disease control immediately as well as at 2-months follow up after selfregulation program. Asthma control questions were presented in order of highest improvement to the least improvement (table 3).
Multivariate analysis of variance for change in patients' asthma control over time was significant. As shown participants had significant improvement in asthma control immediately post program and this improvement was maintained at 2-months follow up as well (table 4).
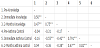
Pearson product moment correlations among outcome variables were shown in table 5. It should be noted since the control scoring shows that the highest the score the less control over asthma, a significant negative correlation was seen among knowledge and asthma control. Therefore highest knowledge score was associated with lower control scores meaning patient have improvement in asthma control with improvement of their knowledge of the disease and skills for self-regulation management.
Univariate analysis of variance for mean differences in study outcomes across the different levels of each of the socio-demographic variables are shown in table 6. As the results reveal only a significant difference was found in knowledge scores among patients with different levels of education at pre test. University degree had the best knowledge of asthma and its management. Concerning asthma control, both age and gender exerted a difference among patients in their symptom control at two months follow-up. Patients above thirties as well as females had better asthma control.
Finally, repeated-measures ANOVA was carried out for determining significant differences in knowledge and asthma control mean scores for the different levels of the given sociodemographic variables across the three time points of study (Table 6). Therefore, the main effects of each of time alone, group alone and the interaction effects for the product of group and time were all studied with the repeated measure ANOVA. None of these analyses showed any significant differences.
6. Discussion
This study explored the effects of a developed evidence-based self-regulation training program on asthmatic patients’ outcome. The fact that majority of the study participants were females could be attributed to the existing high prevalence of the disease among females worldwide. According to Center for Disease Control and Prevention (CDC) [41] prevalence of asthma among women is nearly double that among men (9.7 vs. 5.5%). Janevic et al. [42] further contended that the greater asthma prevalence observed among women has been related to multiple issues including for example, hormonally-linked biological differences, greater effects of smoking and obesity, moreover certain risk factors for poor asthma outcomes such as depression and medication non-adherence may also be more common among women.
This is the first article to integrate an evidence-based self-regulation intervention within the context of asthma self-management among Saudis and generally in Arab world for the purpose of achieving patients’ disease control and knowledge improvement and to describe outcome changes over time. The SRMI provided a framework to help guide our intervention and understanding of effect of facilitating asthmatic patients understanding the complexity of illness representation and management and control strategies on their improved outcomes.
The knowledge of asthma, treatment self-management and asthma control, were found to significantly change over time. This intervention resulted in a marked improvement of asthma control, and a progressive increase in knowledge of asthma. The improvement observed in asthma outcomes, however, may be explained by a better understanding of the management of asthma. Browning, et al. [36] explained that according to self-regulation Model of Illness (SRMI), theory suggests that individuals search to understand their illness or disease threat by developing an understanding of what the illness is, what it means, its causes, its consequences, how long it will last, and whether it can be cured or controlled. Browning, et al. [36] further added that individuals are thought to reduce their health risk or change their health behavior in ways consistent with their own illness representation that is most commonly formulated from personal experience (physical symptoms and emotions), social influences, and/ or interaction with healthcare providers.
Self-regulation, as it relates to asthma, entails the ability to observe, make judgments about the observations, try out change strategies to improve management, and react appropriately to the change effort [30], which have been emphasized throughout the study conduction. In a similar study, Genugten, et al. [43] developed a self-regulation intervention for the prevention of obesity among overweight adults over a period of three weeks. Their intervention showed positive results in preventing weight gain at the population level, at relatively low costs. So, self-regulation training was proven effective over a variety of patients’ diagnoses [43,44].
In a similar study, Mahootti, et al. [45] found that self-care education promotes awareness, attitudes and behaviour of patients and also to reduce the number of asthma attacks. This study further showed that behavioural factors of the intervention group rather than the control group after training had a significant and positive association and patient’s behaviour can be promoted. The vital relationship between knowledge and attitudes was also evident in this study. Kotwani and Chhabra [23] reported that educational intervention led to better adherence to medication for a brief period of time and that reinforcement of the educational intervention with written self-management programme may be required for continuous and sustained asthma control.
Wang, et al. [46] study was designed to determine the effectiveness of an asthma education program on asthma general knowledge and HRQOL. Authors indicate that a 4-hour group structured education program improved patients’ knowledge about asthma and that differences in asthma knowledge scores at follow-up likely reflect an effect of the educational program, the goal of which was to enable patients to monitor, to control, and to manage their disease.
In a similar study, Kuo, et al. [47] studied physiological and psychological efficacy of a self-regulation protocol in lowering acute exacerbation symptoms in patients with chronic obstructive pulmonary disease after a four-week self-regulation protocol. The results of this study revealed that the self regulation program had improved symptom distress, pulmonary functional status, and that cases of unscheduled physician visits of acute exacerbation in the intervention group were significantly lower than those in the comparison group.
Asthma education program, however, yielded variable results in previous studies. Choi and Chung [48] conducted study to examine the effect of an individualized education programme on asthma control, inhaler use skill, asthma knowledge and health-related QoL (HRQoL) among poorly compliant adult Korean patients with asthma. Their study results showed that peak expiratory flow rate, inhaler using skill scores and health-related quality of life scores improved following the intervention, whereas knowledge score did not. The effect on the PEFR score was sustained, with that of inhaler use skill increased over time from 4-8 weeks, however, the healthrelated quality of life effect was not sustained for 4-8 weeks after the intervention. They therefore recommended that innovative education methods may be needed to improve and to maintain pulmonary function, symptom control, asthma knowledge and health-related quality of life of poorly compliant adult patients with asthma.
The reason for current study findings could therefore partly explained in light of the self regulation theory by the role of motivation as important component of self regulation. Psychological needs determine the regulation of the person's behavior through a continuum of self-determination that include internalizing behavior, which can range from a motivation through the extrinsic motivation (external regulation) to intrinsic motivation [49]. Teixeira, et al. [50] suggests that if individuals fully endorse behavioral goals and feel not just competent but also autonomous about reaching them, as suggested by self-determination theory, their efforts are more likely to result in long lasting behavior change.
Moreover, current study findings could further be explained in light of Kuo, et al. [47] view. The authors explained that the self-regulation protocol is patient centered and emphasizes the patient’s own observation of his/her acute exacerbation situations in daily life allows him/her to discover their individual physiological and environmental factors that trigger acute exacerbation and, based on their own triggers, to learn to control situations that might lead to episodes. Through the self-regulation cycle, the subjects learned to adjust their own lifestyles to effectively prevent episodes from happening in the long run.
The research findings by Kavut and Kalpaklioglu [51] of the important role of education in achieving asthma, further supported that fact that despite the observed percentage change in studied patients' asthma control, their achievement would only be explained by each person’s ability to perception that vary because of their willingness, mind skills, and training level. On the other hand, Chen et al. [52] study found that patients with high self-efficacy have better control over their ailment. In contrast, patients with low self-efficacy are often pessimistic and depressed and tend to develop complications that worsen extant conditions. They further added that providing patients with positive recognition of self-care behaviors and promoting willpower and confidence through various information sources to achieve an expected result appear to improve healthcare behaviors effectively.
In addition, therapeutic patient education, particularly when including written instructions in disease self-management, enhances the outcomes in patients with asthma [53]. This could also heightened results achieved in our study. Moreover, current findings similarly to Wang, et al. [46], found that patients with higher levels of education may have better asthma knowledge than their less educated peers. This was attributed to increased cognitive ability and motivation to seek health-related information, which, in turn, can help facilitate knowledge about disease self-management, reduce restrictions on daily activities, and improve quality of life.
On the other hand, contrary to Gallagher, et al. [28], patients older than 33 years had better control of disease at 2 months follow up. Gallagher, et al. [28]. They demonstrated that younger patients with a more recent chronic illness diagnosis are particularly in need of support for self-management.
Furthermore, there was a strong correlation shown between improvement in knowledge and asthma outcomes in current study, suggesting that knowledge developed through strong evidence based theory driven behavioural self-regulation intervention does translate into positive behavior changes. Previous research have however shown that patients with more intensive treatment, and poor symptom control had slightly more difficulties in executive functions and selfregulation [45,54]. Health care professionals should therefore be motivated to incorporate self-regulation elements into their practice, to support asthma patients to identify problems from their own point of view and to learn problem-solving skills to find solutions [53]. The important concept of self-regulation is not sufficiently implemented in daily practice, health care providers especially nurses convey information about asthma and technical skills following traditional patient education disregarding that the link between knowledge and behaviour is weak [53]. Zarei, et al. [39] reported that educational and modifying intervention to prevent asthma triggers was effective in the improvement of asthma control in adolescents. This current finding could also be explained in light of Wagner [55] who contended that patients and families suffering from chronic illness require planned, regular interactions with their caregivers, with goal of improving on function and preventing exacerbations and complications. This interaction should therefore include systematic assessments, attention to treatment plans, and sophisticated behavioral support for the patient’s role as self-manager.
Another plausible reason for the current findings was the well reported sensitivity to change for the instruments used in the study. Both Knowledge and asthma control questionnaire are reliable, have face and content validity, and are very sensitive to change. Finally, the great emphasis that had been given in the program to effectively develop patients’ capability of effectively using the inhalers through the group and individual session also contributed to the positive outcome in the current study. This was consistent with Yildiz [56] findings that proper education and training in correct inhalation technique has been reported to have a substantial role in the achievement of optimal therapeutic benefit and asthma control. Yildiz, [56] found that close follow-up with repeated checking of the patient’s inhaler technique and correction of errors each time seem to be associated with a significant decrease in the percent of patients who make basic errors in inhalation maneuvers and device-independent errors, and with better control of persistent asthma.
In conclusion, evidence from our findings indicated that intervention based on self-regulation theory could enhance patients’abilities to manage their chronic conditions. This evidence make explicit how a theory-based intervention promotes evidence-based nursing practice and advances nursing knowledge by integrating theory, research and practice [47].
7. Conclusion and Recommendations
This was a fourteen-week pre-post intervention study which included strategies aimed at promoting adoption of individual self regulation skills. After an initial encounter with study participants, assessment of educational needs and asthma control were done, followed by a six-session asthma-self regulation intervention each for minutes and follow-up immediately post program and at 2 months. Asthma control criteria, knowledge about asthma were assessed at each scheduled follow-up.
Data from 30 asthma patients, showed a progressive increase in asthma knowledge and an improvement in asthma control. The results of the study proved the efficacy and effectiveness of the selfregulation intervention for promoting knowledge and symptoms control in patients with uncontrolled asthma.
On the basis of this study, we conclude that current findings hold important implications for effect of self-regulation in building patients’ capacity to manage asthma more effectively. This program should therefore be considered as an adjunctive treatment for these patients.
Research to investigate the barriers for implementation and to evaluate which approaches and strategies are needed and most successful to overcome the barriers in implementing evidence based patient self-regulation education into clinical practice is warranted [53]. Future research should also focus on measuring self-efficacy change and more examination of the relationship between selfregulation and self-efficacy, especially in the area of their directionality or reciprocality at longer follow up periods.
8. Limitations of the Study
Current study has several limitations. Larger clinical groups are needed to confirm current results. Adherence to medical treatment should be precisely monitored and studied, using well-established measures. There is also a need to investigate the long-term effects of asthma self-regulation programs in extended longitudinal research.