1. Introduction
It is estimated that there are approximately 350-400 million hepatitis B virus (HBV) carriers and 240 million patients chronically infected with HBV in the world. The spectrum of HBV infection ranges from asymptomatic carriers, acute hepatitis, chronic hepatitis, fulminant liver deficiency, cirrhosis to hepatocellular carcinoma (HCC) [1-3]. Various factors including age at the onset of infection, sex, immune status, ethnic origin, alcohol intake and dual infection with other viruses which affect the liver (HIV, HCV) may have a role in the progression to chronic hepatitis B (CHB) [1,3]; however, the question of how HBV infection affects the liver is still not clear.
Serum mannose binding lectin (MBL) is an important molecule in human innate immunity [4]. This protein is a calcium-dependent lectin that acts directly as an opsonin by binding to collectin receptors through its collagen domain [4-7]. Serum MBL levelsvary from < 20 ng/ml to 10,000 ng/ml [8], but it can arise to twofold or threefold in cases with infections [7]. Serum MBL may have an influence on disease progression via regulating the production of inflammatory cytokines such as IL-6, IL-1ß, and TNF-α by monocytes as a result of infection [9]. Low MBL level may confer a generalized sensibility to infection in children and adults [10]. The MBL gene was reported to play a significant role in the progression of HBV infection in adulthood [11]. Heterogeneity of the MBL gene was informed to be a significant factor in the assessment of the prognosis in chronic hepatitis C [12]. Low serum MBL levels were associated with the occurrence of poor prognosis in progressed carriers [2,5], however, other studies do not confirm these findings [13]. In this study, we investigated the association between MLB level and chronic hepatitis B disease.
2. Materials and Methods
2.1 Patients
A total of 71 subjects (male: 35 [49.3%], female: 36 [50.7%]) was enrolled from the outpatient clinic of the Gastroenterology Department of DışkapıYıldırımBeyazıt Training and Research Hospital. The patients were classified into three groups; Group1; active chronic hepatitis [n: 30, HBsAg (+), elevated transaminase ≥ 2 times the upper limit of normal at least once during the followup period]; Group 2; inactive chronic hepatitis [n:20, HBsAg (+), normal transaminase level, HBVDNA; negative]; Group 3; the healthy controls [n:21]. The diagnostic criteria for chronic HBV infection were; seropositivity for HBsAg more than 6 months and seronegativity for anti-HBs and presence of anti-HBc. Patients with chronic hepatitis and inactive carriers had no evidence of portal hypertension and/or liver cirrhosis and HCC. Stage of fibrosis is classified according to Ishak scoring system. The patients with chronic active hepatitis were divided into three groups according to the stage of fibrosis (Group 1F: stage 0,1; Group 2F: stage 2-3; Group 3F: stage 4-5. The study was approved by the Ethics Committee of DışkapıYıldırımBeyazıt Training and Research Hospital. Informed consent was obtained from all subjects.
2.2 Laboratory analysis
Fasting blood samples were obtained to measure serum levels of alanine aminotransferase (ALT), aspartate aminotransferase (AST), prothrombin time (PT), partial prothrombin time (PPT), HBsAg, Anti HBs, HBeAg, antiHBe, anti-HBc and HBVDNA. Serum ALT and AST levels were determined by spectrophotometric assay (modified IFCC method, Advia 2400, Siemens Healthcare Diagnostics Inc., TarrytownUSA). Plasma PT (Thromborel S reagent) and PTT (Dade Actin FSL Activated PTT Reagent) were measured using an automated coagulation analyzer (Siemens Dade Behring BCS XP, Tarrytown USA). HBsAg and anti-HBs antibody, HBeAg and anti- HBe antibody were measured using enzyme-linked immunosorbent assay (ELISA) (DiasorinEti-max 3000, Italy). AntiHBcIgM was determined by electrochemiluminescent assay (Roche Diagnostics GmbH, Mannheim, Germany). HBVDNA was measured using Real- Time PCR (Qiagene, Valencia; CA).
2.3 Serum mannose-binding lectin measurement
Fasting venous blood samples were obtained from all subjects after an overnight fasting for the assessment of serum level of MBL and stored at -80ºC until analysis. MBL oligomer level was measured by commercial ELISA kit (Bioporto diagnostic, Denmark). Calibrators, samples, and controls were incubated in micro-wells precoated with monoclonal MBL antibody. MBL present in the solutions binds to the antibody-coated wells. Biotinylated monoclonal detection antibody was added to incubate. Unbound detection antibody was removed by washing. HRP-conjugated streptavidin was added to each test well-unbound conjugate was removed by washing. After TMB (tetramethylbenzidine) was added, the enzymatic reaction was stopped chemically. The absorbance was read at 450 nm in an ELISA reader (EPOCH, USA). The interassay coefficient of variation for level 1 was 3.6%. The interassay coefficient of variation for level 2 was 3.8%. The interassay coefficient of variation for level 1 was 9.2%. The interassay coefficient of variation for level 2 was 4.3%.
2.4 Statistical analysis
Differences in age, ALT, AST, HBV-DNA, HBeAg, platelet count and MBL levels between patients and controls were assessed by Kruskal-Wallis and Mann-Whitney U-test. Pearson’s correlation test was used to determine the association between MBL, AST, ALT, HBeAg, HBV DNA and platelet count in active/inactive chronic hepatitis and controls. Pearson’s correlation test was used to determine the association between MBL level, stage of fibrosis and HAI in active chronic hepatitis. All statistical analyses were performed using the SPSS program, version 17.0 [SPSS Inc, Chicago, IL, USA]. Statistical significance was accepted at P < 0.05.
3. Results
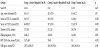
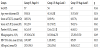
Clinical and viral backgrounds of patients in every three groups are depicted in Table 1. The mean ± SD of MBL level was as 2875.3 ± 2040.03 ng/ml in active HBV patients, 2463.9 ± 1915.4 ng/ml in inactive HBV patients, and 1865.04 ± 265.6 ng/ml in healthy controls (p = 0.344). MBL levels were higher in active hepatitis B group than inactive hepatitis B and control group. But, the difference did not reach statistical significance (Figure 1). The correlation analysis did not show any significant association of MBL levels with the stage of fibrosis (r: 0.077, p: 0.687) (Figure 2). No correlation was observed between MBL and HAI and between MBL and stage of fibrosis (r: -0.30, P: 0.876 and r: 0.077, P: 0.687, respectively). Comparison of the baseline parameters in term of the stage of fibrosis is depicted in Table 2. Statistically, the significant difference was observed in age between group 1 fibrosis (F) and group 2F (P = 0.014). Serum ALT level and HBVDNA were significantly lower in group 1F compared with group 2F (P = 0.041) and significantly lower in group 1F compared with group 3F (P = 0.039 and P = 0.013, respectively). Serum AST level was significantly lower in group 1F compared with 2F (P = 0.041) (Table 2).
4. Discussion
In this study, we examined the association between MBL levels with progression of chronic hepatitis B disease. Although MBL levels were higher in active hepatitis B group than in patients with inactive hepatitis B and control group, the difference did not reach statistical significance. MBL was not correlated with HAI and the stages of fibrosis. One of the major public health problems in the world is persistent HBV infection. Numerous factors including viral and host factors may play a role in the pathogenesis of viral hepatitis. The pathogenesis of progression from chronic liver disease to cirrhosis is a multistage process involving chronic liver cell injury, inflammation, fibrosis and hepatocyte regeneration [14,15]. Increased inflammatory cytokines may contribute to fibrogenesis and proliferation of hepatocytes leading to cirrhosis and HCC [14,15]. The extent of liver fibrosis is significantly related to prognosis and management of chronic viral hepatitis [16]. There are numerous non-invasive methods for the assessment of liver fibrosis which are fibroscore, AST/ ALT ratio (AAR), AST-to-platelet ratio index (APRI), sonography, Fibro-α score, King score, Biotechnology Research Center scores and transient elastography [17].
The MBL gene was reported to play an important role in determining the progression of HBV infection. MBL is known to be an acute phase reactant, rising up to threefold after infection or surgery [2,4-7,13]. The human MBL gene (mbl2) is located on chromosome 10q11.1–q21 [18]. The patients’ immune response which may partly depend on gene mutations of MBL is associated with the clinical result of HBV infection [19,20]. Homann et al. reported an increased serum MBL level in patients with decompensated alcoholic cirrhosis [21]. Hakozaki et al. studied serum MBL levels in 43 patients with fulminant hepatic failure (FHF) and 260 healthy controls and showed that high levels of serum MBL correlated with the survival of patients with FHF due to HBV infection. Therefore, they concluded that serum MBL may be useful as a predictive factor for the survival of patients with FHF caused by HBV [2]. Comparable results were shown in our study revealing higher MBL levels inactive HBV group than inactive HBV group. But, the difference did not reach statistical significance. In another study, Chong et.al reported lower MBL levels in progressed HBV carriers when compared with nonprogressed carriers. Also in this study, they showed that low MBL genotype was associated with the occurrence of cirrhosis and HCC in progressed HBsAg carriers [5]. Another study examined MBL2 polymorphisms in Chinese subjects classified as asymptomatic chronic (n: 64), cirrhotic (n: 45) and HCC (n: 37). They found that median MBL levels were lower in all groups than the control group but there was no difference in MBL levels between disease groups [20]. Various studies examined the potential effect of MBL polymorphisms in HBV disease; some studies find a relation between MBL polymorphisms that present low levels of protein and poor prognoses such as viral persistence [22], disease progression [5,20,23], HBV progression [23] and survival of fulminant hepatic failure [2]. Thio et al. found that MBL2 genotypes correlating with increased MBL levels are related to recovery from an HBV infection whereas those correlating with lower levels are associated with viral persistence [22]. In conclusion; the association between MBL levels and the progression of HBV infection is still not clear and this relation has not been studied in Turkish population previously. MBL may be beneficial as a noninvasive predictor of the survival of patients with hepatitis B virus infection. Therefore, we examined whether there was a relationship between MBL levels with progression of hepatitis B virus infection using liver fibrosis. However, we could not find any significant association between MBL levels and progress of HBV infection in our patients. Further prospective studies on large patient populations are needed to examine whether there was a clear relationship between MBL and progression of hepatitis B virus infection.
Competing Interests
The authors declare that they have no competing interests.