1. Background
Malaria remains a major public health problem instead of many strategies developed by WHO and his partners to control and eliminate this disease. In malaria endemic Sub-Saharan countries pregnant women and children under-fives years are a high risk of malaria and death. Malaria control programs currently comprise integrated interventions, including vector control with use of mosquito nets and spraying with insecticides, Intermittent Preventive Treatment in pregnancy (IPT), early diagnosis and effective treatment of clinical cases [1]. Artemisinin Combination Therapy (ACT) associated with others control and elimination strategies are contributed to reduced malaria morbidity and mortality. But emergence and extension of resistance to artemisinins derivatives in South East Asia could counteract these benefits [1]. Currently, Artemether + Lumefantrine (AL) and Artesunate + Amodiaquine (AS-AQ) are the widely available drugs, which are recommended by most malaria endemic countries in the treatment of uncomplicated falciparum malaria [2]. Monitoring of artemisinin-based combination therapy (ACT) becomes particularly important in the light of emergence of artemisinin resistance in South-East Asia [3,4].
The World Health Organization (WHO) recommends that the efficacy of the first and second-line antimalarial drugs be regularly assessed for early detection and prevention of spread of resistant parasite populations every two years [5].
Surveillance of artemisinin resistance to date has relied on in vivo studies to measure early clearance of peripheral parasitaemia by microscopy and k13 propeller gene mutations [6]. In Côte d’Ivoire, AS + AQ and AL have been recommended in the treatment of uncomplicated malaria since 2005. To detect early artemisinin resistance in the country National Malaria Control Program (NMCP) of Côte d’Ivoire conducted with the help of his Scientific Committee efficacy studies of ACTs recommended for uncomplicated falciparum malaria treatment in the country every two years since 2009. Twelve sentinels sites have been identified around the country and Abidjan and Man are among the first sites since several years. Previous study conducted in these two sites in 2013 demonstrated that both ACT was efficacious and well tolerated [7].
The main purpose of this study was to assess efficacy and safety of AS + AQ and AL the two recommended ATCs in the first line treatment of uncomplicated falciparum malaria in Côte d’Ivoire. Data from this study will help NMCP to update malaria treatment guidelines.
2. Materials & Method
2.1 Study design and sites
This study was an open label, non-inferiority, randomized trial conducted in patients older than 6 months at Man and Abidjan and was carried out according to current WHO protocol [5]. The study was conducted from January to May 2016 in the two sites.
Abidjan located in the south and Man in the west of the country are among the sentinels sites for antimalarial drugs efficacy monitoring since several years.
Malaria transmission is intense with recrudescence during the raining season in the two sites. The main vectors are Anopheles gambiae and Anopheles funestus. Plasmodium falciparum is the predominant malaria parasite, accounting for more than 95% of infections in children under five years of age [7]. The key malaria control interventions in the sites include use of LLNIs, malaria case management with ACTs, Intermittent Preventive Treatment during Pregnancy (IPTp).
2.2 Study population
Patients were enrolled in the study according to Who inclusion and exclusion criteria [5].Briefly patients older than 6 months with the following inclusion criteria were eligible for the study: monoinfection with P. falciparum detected by microscopy, parasite density between 2,000 and 200,000 asexual parasites/μl, axillary temperature ≥ 37.5 °C or history of fever during the 24 hours before recruitment.
Additional inclusion criteria were minimum body weight of 5 kg, ability to swallow oral medication, informed consent from the patient or from a parent or guardian in the case of children; and ability and willingness to comply with the protocol for the duration of the study and to comply with the study visit schedule.
Exclusion criteria included general danger signs in children under 5 years or signs of severe falciparum malaria according to the definitions of WHO [8]; severe malnutrition according to WHO child growth standards [9]; febrile condition due to diseases other than malaria (e.g. measles, acute lower respiratory tract infection, severe diarrhea with dehydration) or other known underlying chronic or severe diseases (e.g. cardiac, renal or hepatic diseases, HIV/AIDS).
2.3 Sample size
The sample size was calculated using the WHO guidelines on assessment of antimalarial drugs [5]. Population size was determined according to the following criteria: the proportion of probable clinical failures with the antimalarial combinations studied should not be higher than 10%, for a level of confidence (P) of 95% and a precision (p) of 10%, taking into account patients who were excluded or lost to follow-up. Using these criteria, a minimum of 50 patients was required in each treatment arm in each site.
2.4 Randomization and Drug administration
Patients were randomly assigned to receive either AS+AQ or AL. Both treatments were three-day oral regimens dosed by weight according to the manufacturer’s instructions: AS + AQ 5 to <9 kg: one tablet/day of artesunate (AS) 25 mg/amodiaquine (AQ) 67.5 mg; 9 to <18 kg: one tablet/day of AS 50 mg/AQ 135 mg; 18 to <36 kg: 1 tablet/ day of AS 100 mg/AQ 270 mg; ≥36 kg: 2 tablets/day of AS 100 mg/ AQ 270 mg. AS+AQ was administered once daily under observation by the research team.
AL tablet strength was 20 mg artemether/120 mg lumefantrine: 5 to <15 kg: 1 tablet/dose; 15 to <25 kg: 2 tablets/dose; 25 to <35 kg: 3 tablets/dose; ≥35 kg 4 tablets/dose. AL was administrated twice a day.
The first dose was taken at enrolment, the second dose eight hours later on day 0, and then two doses at 12-hourly intervals for the subsequent two days. The first dose was given at the site by the research team. The second dose was not directly observed and patients were precisely instructed how and when to take this second dose. All tablets were either swallowed whole or crushed with water and Yoghurt.
Patients who vomited during the observation period were retreated with the same dose of medicine and observed for an additional 30 minutes. Patients with repeated vomiting were excluded and were treated according to NMCP treatment guidelines and excluded from the study.
2.5 Clinical procedures
Physical examination, vital signs, body temperature, and clinical assessment were done at day 0 (screening), and at all follow-up visits (days 1, 2, 3, 7, 14, 21, 28, 35 and 42).
Medical history, demographic information and contact details were collected at screening. We recorded body weight at date 0 and Axillary, or rectal temperature was performed at baseline (day 0 before dosing) and on days 1, 2, 3, 7, 14, 21, 28, 35 and 42 or at any unscheduled visit.
3. Laboratory Procedures
3.1 Microscopy
Thick/thin blood smears were collected at the time of screening to confirm adherence to the inclusion and exclusion criteria. Thick blood films were also done at days 2, 3, 7, 14, 21, 28, (35 and 42) or on any other day if the patient returns spontaneously and parasitological reassessment is required. Blood smears were stained with Giemsa 10% and were examined at magnification100X (oil immersion). Parasitemia was measured by counting the number of asexual parasites against a number of leukocytes in the thick blood film, based on a putative count of 8000 leukocytes per microliter of blood.
The number of asexual parasites was counted against 200 leukocytes using a hand tally counter. If P. falciparum gametocytes were seen, a gametocyte count was performed against 1000 leukocytes. Counts were performed by two independent microscopists; discrepant readings were resolved by a third reader.
3.2 Parasite genotyping
Blood spots on Whatman® 3MM filter paper were prepared for PCR genotyping on screening and in the event of re-appearance of parasites, confirmed by microscopy, or on any other day if a patient returned with fever. Multiplicity of infection was assessed using three polymorphic loci (merozoite surface proteins 1 and 2 and glutamate-rich protein). Briefly, filter paper blood samples collected on the day of enrolment and on the day of failure were analysed for polymorphism of merozoite surface protein-1 (msp-1) and merozoite surface protein-2 (msp-2) using nested-PCR as previously described [10]. Possible outcomes were new infection or recrudescence. A “new infection” is a subsequent occurring parasitaemia in which all the alleles in parasites from the post-treatment sample are different from those in the admission sample, for one or more loci tested. In a “recrudescence,” at least one allele at each locus should be in common for both paired samples.
3.3 Statistical analysis
Data generated were recorded in individual participants Case Record form (CRF). Data were entered and analyzed with EPI-Info™ software (v 7.1; Centers for Disease Control and Prevention, Atlanta, GA). Analysis of treatment outcome was intention-to-treat (ITT) and per protocol. Per-protocol analysis included all patients who matched all inclusion criteria, were properly randomized, had received the study drugs according to the protocol, and for whom data were available on the study endpoint without protocol violation during the follow-up time. ITT analysis comprised all randomized patients fulfilling the inclusion criteria without repeated vomiting after the first study drug administration. Frequencies were compared by either chi-squared or Fisher’s exact tests, as appropriate, and continuous variables by Student’s t-tests when the data are normally distributed.
3.4 Ethical issues
The study was conducted according to the Declaration of Helsinki and national legal and regulatory requirements. Protocol, CRF and consent form were approved by the “Comité National d’Ethique de la Recherche” of Côte d’Ivoire.
4. Results
4.1 Study trial profile and baseline characteristics
A total of 1,188 patients have been screened for eligibility criteria in the two sites among them 120 and 121 were randomized respectively in AS+AQ and AL group.
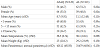
A total of 118 and 116 patients had available data for PP analysis at day 42 respectively in AS+AQ and AL group (Figure 1).The patient population had 56 (46.7%) male and 64 (53.3 %) female patients in AS+AQ group. In AL group patient population had 62 (51.2%) and 59 (48.8%) males and female respectively. The mean age was 8.7 and 11.1 years respectively in AS+AQ and AL group. Overall, both groups of patients were comparable at the inclusion regarding baseline characteristics (Table1).
4.2 Fever and parasite clearance
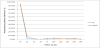
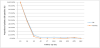
As shown in Figure 2, the proportion of participants without fever was similar on days 2 and 3. On day 2, the fever clearance rates was 99.2% and 98.3% in the AS +AQ and AL groups, respectively (p >0. 5), while on day 3, this rate was 100% in each group (Figure 2). Both treatments resulted in rapid clearance of parasites (Figure 3) as parasite clearance rates on day 2 was 95% and 90.7% in the AS + AQ and AL groups, respectively. At day 3 parasite clearance rate was 100% in AS+AQ group and 97.4% in AL group. 4 patients presented delayed parasite clearance at day 3 in AL group.
4.3 Therapeutic Response and tolerability of drugs
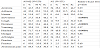
The PCR-corrected ACPR at day 42 in PP analysis was 99.2% and97.4 for AS+AQ and AL, respectively. In the ITT analysis, the irrespective ACPR was 97.5 % for AS + AQ and 93.4 % for AL (Table 2). Most treatment failure (10 patients) occurred in AL group at Abidjan site among them 9 patients have taken AL from the same Pharmaceutical lab.
AS + AQ, artesunate + amodiaquine; AL, artemether–lumefantrine. P values were obtained by Fisher’s exact test.
The most commonly reported and possibly drug-related adverse events to both combination therapies were effects of malaria infection. None of the patients presented with serious adverse events. Adverse effects such as anorexia (42.5% vs 28.1%), drowsiness ( 28% vs 0%), dizziness (30% vs 2.5%), Headache (77.7 % vs 48.8%) were more frequent in the AS+AQ group compared to the AL group (p < 0.05). All of these events were described as mild or moderate (Table 3).
5. Discussion
Malaria is still associated with high morbidity and mortality especially in children under five years of age in Sub-Saharan endemic countries.
Artemisinin-based combination therapies (ACTs) are recommended by most of National malaria control program as the first-line treatment for uncomplicated P. falciparum malaria. This strategy, has, produced a notable decrease in the mortality and in reducing the global malaria burden. However, Resistance of Plasmodium to artemisinins reported in several countries in South-East Asiais, therefore, of great concern [11,12,13]. The spread or independent emergence of artemisinin resistance in other parts of the world could pose a major public health problem as no alternative antimalarial medicine is available at present with the same level of efficacy and tolerability as ACTs.
The present study based on the in vivo efficacy using 42-follow up days protocol was conducted to provide supporting evidence for the clinical efficacy of AS + AQ and AL in the country. The two ACTs were adopted and implemented as anti-malarial drug policy in Côte d’Ivoire since 2005.Results from this study demonstrated high efficacy of the two ACTs as PCR adjusted ACPR for each ACT remains above the 95 % efficacy threshold recommended by the WHO [5].Both treatments proved to be efficacious but delayed parasite clearance time observed in AL group in Abidjan site raise concerns. In this study more than 3 trade name of artemether + lumefantrine have been used at Abidjan site. All these drugs have been provided by the NMCP. Among 10 patients with clinical failure 9 have received the AL drug from the same pharmaceutical lab. Administration of artemether-lumefantrine with food is important to achieve sufficient exposure to lumefantrine up to day 7, which is required for a high cure rate [14,15]. In this study only first doses of AL were observed. As absorption is fat dependent, patients were precisely instructed to give the second dose with fatty food at home. However, intake of this second dose was not directly controlled. Food is known to increase the bioavailability (BA) of lumefantrine by up to 16-fold and that of artemether by up to 3-fold.
General inter-individual variability for drug absorption and pharmacokinetic may be associated with changes in the bioavailability of a drug and consequently may affect the therapeutic efficacy.
A study conducted in Nigeria indicated an increase in parasite clearance time and high frequency of crude late parasitological failures among the patients, indicating reduction in the therapeutic efficacy of Artemether + lumefantrine [16].
In the same site (Abidjan) in 2013, three years ago ACPR after adjustment by PCR of AS + AQ and AL was 100% for each drug at day 42.The same result was obtained with the two ACTs in Man site in 2013 [7]. Others studies conducted in the country have demonstrated also good efficacy of AS+AQ and AL in the treatment of uncomplicated falciparum malaria [17,15,19-22].
Although most studies carried out in malaria endemic countries in Africa [23-26] had shown good efficacy and safety of ACTs for the treatment of uncomplicated malaria, the conditions of clinical trials do not fully reflect real field situation. Results from studies conducted with unsupervised malaria treatment showed low cure rate after adjustment by PCR at day 28 [27,28].
Some studies demonstrated that unsupervised intake of AL was highly efficacious despite the lumefantrine plasma levels concentrations being significantly lower than in patients whose treatment had been supervised [29-32].
Both treatments were generally well tolerated; the overall incidences of AEs were more frequent in the AS + AQ than AL treatment groups. The most commonly occurring AEs included anorexia, drowsiness, dizziness and Headache.
Our study has several limitations. The lack of sufficient sampling times for fever and parasite clearance time. We were not able to determine the levels of drugs concentration which may have been of interest for its contribution to the therapeutic efficacy of ACTs.
6. Conclusion
Although results from this study proved good efficacy of AS+AQ ad AL in the treatment of uncomplicated falciparum malaria in the two sites, constant monitoring of these two ACTs is needed.
Competing Interests
The authors have no competing interests with the work presented in this manuscript.
Author Contributions
All authors participated in the design, implementation, and analysis or data interpretation of the study. Offianan AT was involved in all phases of the study, N’guessan Tiacoh L, Kouame E, Kokora A., Amata Eric, Kinifo-Lawson V were responsible for conducting field studies and coordination of study procedures. Ira Bonouma, Djaman Jisephn Assi Serge B and Ronan jambou supervised the study. Data analysis was done by Adji Eric Gbessi. Coulibaly Baba and Ako Ako Aristide B performed PCR analysis. Yao Serge S and Albert Gnondjui undertook lab procedures. The manuscript was drafted by Offianan Andre Toure. All authors critically reviewed the report and approved the final version of the report for submission.
Acknowledgments
We are grateful to participants, medical staff and all health authorities in the study sites for collaboration. The authors would also like to acknowledge National malaria Control Program and WHO Global Fund.