1. Introduction
The substantially increasing prevalence of multi-drug resistant organisms (MDROs) especially the extended-spectrum B-lactamase (ESBL) producing Eenterobacteriaceae isolates and carbapenem resistant Acinetobacter baumanni and Pseudomonas aeruginosa were not only found in Taiwan but also in the other areas of word [1-3]. Clinicians face tremendous challenges in the treatment of those patients, especially in the healthcare-associated infections (HAI). They not only result in greater mortality and morbidity, but can also increase the length and cost of hospital stay. Moreover, it is important that immediate use of antimicrobial agent must be chosen appropriately. Otherwise, inadequate or delayed use of empiric antimicrobial therapy is known to be associated with higher mortality, longer duration of hospitalization, and increased prevalence of MDROs [1].
Tigecycline, a derivative of minocycline, is one of the glycylcycline classes of antibiotics. It has a broad spectrum of activity against a variety of Gram-positive and Gram-negative aerobic MDROs, anaerobic and atypical pathogens, including vancomycin-resistant enterococci, methicillin-resistant Staphylococcus aureus, penicillinresistant Streptococcus pneumoniae, Enterobacteriaceae, non- Enterobacteriaceae except Pseudomonas, Chlamydia pneumoniae, Mycoplasma pneumoniae, and Rapid growing Mycobacteria. The U.S. Food and Drug Administration (FDA) approved the use of tigecycline for the treatment of complicated intra-abdominal infections (cIAIs) [4] and skin and skin structure infections [5] in 2005, and for community-acquired pneumonia in 2009 [6]. Due to the growing number of MDROs with a lack of newly developed antimicrobial agent, tigecycline has been given high hopes and expectations as a candidate drug to treat infection with MDROs.
The purpose of this study is to assess the clinical efficacy of tigecycline in hospitalized patients.
2. Materials & Method
The study was conducted retrospectively at a medical center in Northern Taiwan. All hospitalized adult subjects who received treatment with tigecycline between May 2011 and January 2013 were enrolled. Age, sex, underlying diseases, admission settings (intensive care unit or general ward), clinical diagnosis, dosage, microbiological culture and sensitivity testing, indication for tigecycline use, duration of treatment, clinical response, adverse clinical outcomes, and mortality rate were all documented. Patients treated with tigecycline for 48 hours were excluded.
The evaluation of tigecycline’s clinical response was classified as positive response and negative response. Positive response was defined as either complete or partial improvement of symptoms/signs of infection and also included microbiological response, showing sterile culture results during or after the complete course of tigecycline therapy. Negative response was no improvement or deterioration of infection, including persistent positive culture results of the same organism identified after starting tigecycline therapy. Uncertain response was defined as no subsequent follow up of culture results.
3. Results and Discussion
A total of 357 patients were included in this study. Forty eight patients were excluded because their treatment durations were less than 48 hours. Therefore, 309 patients were analyzed in this study.
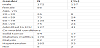
Clinical characteristics of the patients were analyzed and shown in Table 1. About 41% of patients were treated in the intensive care unit (ICU). Most were elderly patients and about 68% of patients were over 60 years old. 57% of the patients had the co-morbidity of diabetes.
All patients received a loading dose of 100mg of tigecycline. However, 76 patients (25%) weren’t given a loading dose initially. As a maintenance dose, 306 patients received 50mg of tigecycline q12h, 2 patients received 100mg q12h, and 1 patient received 75 mg q12h. The median duration of tigecycline therapy was 10 days (range 3-45).
The clinical efficacy of tigecycline and prognosis were shown in Table 2. Our study has shown that tigecycline was used mostly in the treatment of cSSTIs (44%) whereas other clinical studies showed its dominant use rather in IAIs (48%) [7].
Among our patients treated in the ICU, tigecycline was used predominantly for the treatment of hospital acquired pneumonia (HAP) (82/101; 81%) and mostly infected with multi-drug resistant Acinetobacter baumanni (MDRAB), followed by intra-abdominal infections (23/50; 46%).
In our study, improved clinical efficacy of tigecycline was observed in 49% (151/309) of patients, in which higher treatment success was further noted in its use for cSSTIs (101/137; 74%), followed by other types of infection (2/4; 50%) and IAIs (23/50; 46%). In the study of Eckmann C et al., the multicenter study included 656 severely ill patients with cSSTIs and cIAIs. The authors determined that the clinical cure rates of tigecycline for cSSTIs and cIAIs were 82% and 75% [8]. Bassetti and his colleagues reported 73% clinical success from tigecycline therapy, with the highest success rate of 82% recorded in IAIs followed by 73% success rate observed in cSSTIs [7]. A study showed that in vitro of tigecycline with 100% active against MRSA isolates from cSSTIs and the MIC90 for tigecycline, vancomycin and linezolid are 0.25, 2 and 2 mcg/mL separately [9]. It also revealed that good efficacy of tigecycline in the treatment of cSSTIs. In our study, 41% of patients receiving similarly tigecycline treatment were from the ICU but most of them belonged to severe HAI such as HAP or tertiary IAIs with carbapenem resistant MDRAB infection.
In the negative response group of 51% patients, treatment failure was mostly seen in HAP and pneumonias complicated with bloodstream infections (83/101; 82%), followed by UTIs (10/17; 59%) and cIAIs (27/50; 54%). In the study reported by Bassetti and his colleagues, 27% of clinical failure was observed, mostly seen in tigecycline’s empiric use in neutropenic patients (42%), followed by HAP (33%), pneumonia and bloodstream infections (34%), and other bloodstream infections (30%) [7]. In another study reported by Freire and colleagues, tigecycline had relatively lower efficacy in its use in VAP compared with imipenem (47.9% vs. 70.1%) [10]. In January of 2010, FDA issued a safety announcement regarding the increased mortality risk noted to be associated with the use of intravenous antibacterial tigecycline compared to other drugs used to treat a variety of serious infections. This was most clearly seen in patients treated for HAP. It was further revealed in another study that tigecycline had an overall clinical success rate of 30.3% with its efficacy most highly observed in the treatment of those indications approved by the FDA, compared with HAP (66.7% vs. 18.4%) [11]. Coming from these similar experiences, we can see that tigecycline is not recommended to be used in treating HAP and pneumonia with bloodstream infections. This is due to the pharmacokinetic property of tigecycline characterized by its extremely low concentration in the bloodstream, making it problematic for its use in the treatment of bacteremia especially when the MIC of the organism being treated is ≤1mg/L [12,13].
Monotherapy of tigecycline must be paid with great attention in treating cIAIs caused by perforation. In a Phase 3 clinical trial (n=1642) of tigecycline, sepsis/septic shock developed in 6 patients treated with tigecycline and 2 patients treated with imipenem/cilastatin caused by perforation. Due to the low subject size and the variation of APACHE II scores, no conclusive extrapolation has yet been made from these findings [14-16]. Our study found a clinical failure rate of 54% (27/50) from tigecycline use in IAIs, with 20% (10/50) of patients received tigecycline as monotherapy. Further analysis discovered this failure rate to be associated with disease severity, where 46% (23/50) of those treated for IAIs required ICU care. In the guidelines published in 2009 by the Surgical Infection Society and the Infectious Disease Society of America (SIS/IDSA) for the management of cIAIs in adults and children, tigecycline was categorized in its use in only mild to moderate IAIs [17].
Microbiological efficacy of tigecycline treatment was documented in Table 3. A total of 183 bacterial isolates were found and MDRAB was the most commonly isolated (106/183; 58%), followed by Enterococcus faecium (VRE) (26/183; 14%), and Enterococcus species (17/183; 9%).
Based on microbiological efficacy, successful clinical response of 18% (33/183) was recorded, 43% (79/183) failed, and 39% (71/183) was uncertain. If we excluded the uncertain cases, the eradication rate for totally bacterial isolates was only 30% (33/112). Among the cases of clinical failure, 29% (23/79) of patients had super-infection, as tigecycline therapy not only failed to eradicate their bacterial isolates, but also further resulted in the growth of other organisms being cultured, such as Pseudomonas aeruginosa, Prevotella species, and Burkholderia cepacia.
Regarding to tigecycline use in the treatment of UTIs, our study noted a clinical failure rate of 59% (10/17) where 13 VRE and 6 Acinetobacter baumannii bacterial isolates were cultured. Our study has shown that bacterial isolates treated with tigecycline were mainly Acinetobacter baumannii (58%),Enterococcus faecium (VRE) (14%), and Enterococcus species (9%). Regarding micrbiological response, eradication rate for Acinetobacter baumannii,Enterococcus faecium (VRE), and Enterococcus species was 13% (9/68), 58% (7/12), and 70% (7/10) separately. Although the tigecycline’s sensitivity testing for the isolated Acinetobacter baumannii,Enterococcus faecium (VRE), and Enterococcus species, sensitivity were 26%, 99%, and 98%, respectively (Table 3).
A research report has pointed out that due to the emergence of tigecycline resistant micoorganisms, a retrospective analysis of 51 patients treated with tigecycline was analyzed to assess the superinfection rate and the superinfection rate was 23.5% (12/51), in which 58.3% (7/12) was found to be Pseudomonas aeruginosa [18]. Aside from problems with superinfection, tigecycline cannot be used to treat Pseudomonas aeruginosa. Therefore, when it is cultured mostly from patients in the ICU, other broad-spectrum antibiotics should be used to expand the range of activity against Pseudomonas aeruginosa.
Four patients experienced from adverse events after the use of tigecycline. 3 patients discontinued the therapy due to the development of nausea and vomiting; while skin rash occurred in the other patient but continued on with tigecycline treatment as the rash subsided after being given with antihistamines.
Our study showed during the treatment period of tigecycline, mortality rate was 27% (84/309). The main cause of mortality (57%, 48/84) was noted from the treatment of pneumonia in which 48% (48/100) of these patients had HAP. Anthony and colleagues’ retrospective report analyzed 18 patients treated with tigecycline for infections caused multi-drug-resistant Gram-negative organisms. They noted of higher mortality associated with tigecycline’s use in treating Acinetobacter baumannii with MIC ≥2mg/L [19]. In our study, tigecycline was used for treating patients with pneumonia caused by 83 isolates of MDRAB with 63% (52/83) of these organisms’ MIC being ≥2mg/L, and another 39% (32/83) of these organisms’ MIC were even ≥4mg/L.
4. Conclusion
Our study show good efficacy of tigecycline in the treatment of cSSTIs but not in IAIs. This might be due to the greater severity of IAIs in this study and all these patients have more comorbidity that required further care in the intensive care unit. Regarding the treatment of pneumonia, ineffective response was seen as most patients with HAP and infected with MDRAB in our study. Its use in treating other infections not yet approved by the current guidelines such as HAP and UTI requires further research to obtain enough evidence for future approval.
Competing Interests
None of the authors has conflict of interest with the submission.