1. Introduction
In recent years, the number of uninsured and underinsured patients has grown dramatically in large midwestern cities, as it has in many cities around the country [1]. The cost of caring for these patients at local hospitals/health systems has increased significantly [2-4]. As a result, in 2003, a large metropolitan county hospital system in the midwest revisedits copayment policies. On October 1, 2003, the hospital system implemented a patient financial responsibility policy that levied copayments for certain patient populations depending on the services rendered/received.This policy’s goal was to develop a limited cost sharing with patients on the indigent care program as well as to encourage self pay patients to undergo screening for financial assistance programs. In 2004, a revision of this policydecreased the amount of up front (time of service) copay required by self pay patients, but the intent of the policy remained constant.
Measuring the impact of the policy implementationof increased copays on vulnerable patients with chronic diseases and the health systems that care for those patients is an important public health and policy concern. Although onereason for cost sharing policies, such as this, is to reduce hospital costs, other unintented results may occur.Reductions in services at a safety net hospital, could shift patients to other facilities and placesignificant financial strain on other area hospitals, while increasing the long-term cost of care for patients at the hospital itself [5]. Poor patients, now facing higher out-of-pocket costs, may also avoid seeking needed care. Because of decreased access to care, patients could suffer lower quality of healthcare [6-8]. One especially vulnerable population are those with diabetes mellitus (DM), who require frequent access to primary care to adequately control their diseaseUncotrolled DM can lead to poor health outcomes including increased hospitalization [9].
This safety net hospital systemimplemention of policy changes provided a unique opportunity to examine the effects of costsharing among this vulnerable DM population. We hypothesized that a gradient of risk exists for vulnerable patients with DM based on insurance status and perceived financial cost sharing [10,11]. This gradient depends upon the direct financial burden that falls upon patients. These include patients with minimal financial impact from the policy change, including pateints with third party payors such as private insurance or Medicaid, to self pay patients, who bear the entire financial burden of the health care and, after the policy change, faced significant time of service copayments as well.As a result of that gradient of risk, we predicted that a greater financial burden will correspond to: reduced primary care visits,increased emergency department visits, increased hospitalization with increased cost,and worsening quality of care measures such as hemoglobin A1c(HbA1c).
2. Materials and Method
2.1 Study population
The study cohort was drawn from a state-of-the-art electronic medical record system for a public hospital in a large midwestern city. The clinics primarily serve an inner-city population. A large majority of the patients in this system have publicly-financed healthcare coverage including Medicare, Medicaid, and a local indigent assistance insurance program, which covers county residents up to 200% of the Federal Poverty Limit.
Patients with a diagnosis of diabetes mellitus who had activity of at least one visit in the system in each one year period in the county hospital system between October 1, 2000 and September 30, 2003 were included in the initial cohort of study patients. Because of the hypothesized gradient of risk associated with pay or status, determining the insurance status of a patient, over time, was critical to our analysis. Patients with no payment information, gaps in their insurance information, or only one single data record of insurance stored in the system were excluded from the study.
6179 patients were identified in the initial cohort (Figure 1). 13 patients were excluded because they had no insurance information stored in the system during the entire study period. 2636 patients had the same insurance information throughout the study period and were attributed to their respective insurance groups.4 patients had only one single report of insurance information during the study period and were excluded. 3526 patients had different insurances throughout the study period. For these patients, we determined two “sentinel” dates related to the policy changes to group the patients. August 1, 2003 and January 1, 2004 were chosen because of their juxtaposition to the period around co-payment policy changes. 1655 patients had the same insurance on both 8/1/03 and 1/1/04. These patients were added to their respective third party pay or groups. 517 patients were missing insurance data around both sentinel dates and were excluded from the study. 1411 patients had a missing insurance value around one of the two sentinel dates. Because of the co-payment policies explicit intent of encouraging patients to apply for financial assistance programs, patients with either self pay or indigent insurance reported one of the two dates were added to those respective groups. 459 of these patients did not have self pay or indigent as one of their insurance types and were excluded. Lastly, 460 patients had two different insurance statuses on the two sentinel dates. These patients were attributed to their insurance status at the 8/1/2003 sentinel date. An additional 8 patients were excluded because their insurance type on both sentinel dates was “other”, which included workers compensation and subrogation insurance types. 5178 patients remained in the cohort based on this insurance attribution methodology. We then validated the insurance status using two other data fields in the electronic systems that were collected at various points of the revenue stream process. 1162 patients were excluded due to inability to validate the insurance status.
Because patients with co-morbid diabetes mellitus and congestive heart failure have different quality of care and utilization patterns compared to patients with diabetes mellitus alone [12], 1655patients with documentation of congestive heart failure, at some point during the six year study period, were also excluded from the study. The final cohort size for our study includes 2394 adult patients with diabetes mellitus and reliable insurance status during the 5 years of the study period.
Each healthcare delivery entity whose data is included in the combined metropolitan health information exchange has the option to include or not include their data in each study. One of the twenty hospitals elected not to include their data in this study. Thus, county hospital patients who went to this hospital for admission and/ or emergency department visits have missing data for visits to that system, as that visit data is not included in our data set. This study was approved by the Indiana University and Purdue University Indianapolis institutional review board.
2.2 Data Collection
The electronic system captures data on all healthcare encounters (e.g. inpatient, outpatient, and emergency department), diagnoses, pharmacy transactions (for prescriptions filled at pharmacies within the system), laboratory results, vital signs, and text reports occurring at both the reference county hospital system as well as hospital admission and emergency department visit information from other hospitals in the metropolitan area. Data from the system were extractedto monitor heatlhcare quality and utilization measures for three years before and two years after the effective date of the changes [13].
2.3 Methods of Measurement
Several variables for healthcare quality, healthcare costs and utilization were measured. For quality of care, three different indicators, hemoglobin A1c (HbA1c), systolic blood pressure (SBP) and low density lipoprotein(LDL) cholesterol values, were collected and examined by insurance type to determine whether or not a relationship with the policy implementation could be discerned. For healthcare costs, the mean annual charge (monthly) was calculated for each patient in the cohort throughout the study period. Then, utilizing the hospital’s cost to charge ratio, the mean annual cost (monthly) was calculated for each patient throughout the study period. Four measures of healthcare utilization, emergency department visits, hospital admissions, length of hospital stay, and primary care physician visits, were also collected. Data for each study variable was collected 3 years before and 2 years after the policy implementation for the entire cohort and separated by insurance types of commercial/ private, Medicare, Medicaid, indigent, and self-pay.
2.4 Data Analysis
Data were analyzed using SAS (SAS Institute Inc., Cary, North Carolina).Descriptive statistics (e.g., mean, standard deviation for continuous variable, and percentage for categorical variable) were computed for the cohort. Normality checking was performed prior to the modeling and necessary data transformation was applied whenever the normality assumption was not valid. To examine relationships of the policy implementation to the outcomes measures, linear mixed-effects modeling (PROC MIXED) was used for the longitudinal measures in quality of care and healthcare costs. Because the utilization data demonstrated a Poisson distribution, generalized estimation equation modeling (PROC GEE) was used.
3. Results and Discussion
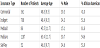
A total of 2,394 patients with age at the beginning of the study period greater than 18 years old, with diabetes mellitus, were included in the study cohort. In general, patients were in their late 40’s and early 50’s, mostly female, with over half of the patients being African American (Table 1). The percentage of patients during the study period with commercial insurance remained stable throughout the study period (14.3% on 10/1/01 and 14.5% on 9/30/05), with no sharp changes noted before or after the policy implementation and washout periods.
3.1 Healthcare quality
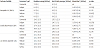
Table 2 shows the clinical quality measures by payment type. The interaction term between time and insurance type represents the significance of the changing relationship from before the policy change to after the policy change. Negative relationships/interactions represent a decrease in the SBP, HbA1c, and LDL values after the policy change (Table 2).
3.2 Healthcare charges
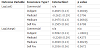
In Table 3, with commercial insurance as the reference group, an interaction term assessed the costs by insurance type before and after the policy change. For example, the interaction value of 0.4605 implies that after the policy change, the group difference between indigent and commercial insurance type in the log of annual costs was 0.4605 higher than before the policy implementation.
3.3 Healthcare utilization
Table 4 shows the four utilization outcomes by payment type after the policy change compared to before the policy change (Table 4). The interaction values of the emergency department visits, hospital admissions, and length of hospital stay, are all positive, which represent an increase in the utilization after the policy change. However, the relationship for primary care visits for patients with the indigent care insurance is also significantly positive (0.0875), indicating that patients with diabetes mellitus with indigent care insurance were more likely to visit their primary care physician after the policy change compared to before the policy.
3.4 Conclusion
In this project, we examined the impact of a newly implemented co-payment policy on patients with diabetes mellitus. We focused on the impact of the policy over three major areas: quality of care, healthcare costs/charges, and utilization. We hypothesized that the policy implementation creates a gradient of risk in all three areas for the patients according to their third party pay or status and related portion of cost sharing. The results supported our hypotheses that increased copayments increased emergency department visits and increased hospital admissions with higher costs/charges but it’s not always true. Primary care visit data were mixed based on the pay or status. We were not able to prove the worsening quality of care measures as a result of the policy implementation.
We did discover both some positive and negative aspects of the policy change. Contrary to our hypothesis, we found statistically significant, albeit questionably clinically significant, improvements in blood pressure (SBP) and glucose control (HbA1c) measures before and after the policy implementation and no significant change in lipid control (LDL).We believe this was not related to the change in the co-pay policy, but may have been due to other quality of care activities in the healthcare system focused on improving the care of patients with diabetes, including implementation of a diabetes registry and incentive compensation to providers for meeting quality targets related to diabetes care. As part of these efforts, for example, physicians and clinical staff were given quality monthly performance reports for diabetes related care measures, including blood pressure control, glucose control, and lipid control [15,19].
The results for healthcare utilization and financial impact [20] however, were generally as predicted. The policy implementation resulted in increased utilization of hospital and emergency department services. Our findings support other research indicating that the increase in patient co-payment may shift costs to more expensive acute care and create a barrier to efficient health care for low-income patient groups [21,22]. A pattern of reduced primary care visits is observed for all payment types except those with the indigent care program. It is not clear why patients on the indigent care program had increased numbers of primary care visits. Improved collection of primary care clinic nurse visits, decreases in capacity of other local health systems for indigent patient care, and changes in perception of value of primary care visits, are all plausible reasons that need further elucidation.
The hypothesized effects of the co-payment policy were most pronounced for patients on the indigent care program and self-pay patients. Minimal impact was expected for Medicare, Medicaid as these patients’ cost sharing responsibility remained consistent. However, the results suggest minimal impact for self-pay patients, mixed impact for indigent care patients, and a tremendous impact for Medicare patients. This change in patterns for Medicare patients was much more negative than hypothesized. More research is needed to understand patient behaviors in this area.
Patients with diabetes mellitus have poor health outcomes, or increased utilization if their disease is not well controlled [9]. Although, in this study, most of the quality of care measures continued to improve over time, the increased healthcare utilization and increased charges revealed the hidden risks for health care systems caring for vulnerable patients with diabetes. The deteriorating utilization pattern may lead to higher medical and social costs in the long-term for these vulnerable patients and the healthcare systems which care for them [23-25]. This deteriorating utilization pattern may ultimately lead to decreased financial benefit to the system and society [25,26].
These results need to be viewed within the context of several limitations. First, the cohort studied contains a majority of female patients. Medicaid patients in this Midwest state are statistically more likely to be females due to eligibility requirements. As a result, the impact on such policies on men may not be fully represented in this study since male patients may not use health care at the same rate as female patients [27]. Second, because the study was limited to patients with diabetes mellitus, it is uncertain if results may be generalized to patients with other types of chronic diseases. However, this study can provide insights into the impact of the policy implementation which may also be applied to other types of chronic diseases. Future studies will be conducted for patients with other types of chronic diseases such as heart failure. Finally, the insurance status of patients in this study was collected in a point by point manner. As a result, pay or information could only be determined when a patient accesses the healthcare system. A continuous, membership level view would provide a more reliable estimate of pay or status, but such data was not available for our entire study populations. While a standard pointby- point method of pay or estimation could not account for services accessed outside of one healthcare system, our study was able to provide significant additional information because the data included point-by-point utilization and clinical data from multiple healthcare systems.
Despite these limitations, this study provides valuable information for this healthcare system and for the policy makers. Results of this study should be taken into account for future cost-effective medical policy implementation. In addition, since the increase in co-payments may force low-income patients to turn to other hospital systems, we also hypothesize that implementation of policies, like this, may shift the indigent population to other hospital systems. These changes could place financial burdens on other area hospitals. Future research should focus on not only a single hospital, but the influence of this policy implementation on other hospital systems [28].
Abbreviations
DM: Diabetes Mellitus; PCC: Primary Care Clinic; MIXED: Linear Mixed-Effects; GEE: Generalized Estimating Equations
Competing Interests
The authors declare that they have no competing interests.
Author Contributions
All the authors substantially contributed to the study conception and design as well as the acquisition and interpretation of the data and drafting the manuscript.