1. Introduction
Blunt vertebral artery injury (VAI) is uncommon. The reported incidence is only 0.5% to 2.0% of all trauma patients [1-3]. However, about 30% of the patients with cervical spine injury are reported to have also suffered a VAI [4,5]. Most unilateral VAIs are asymptomatic on admission, and symptoms develop in a delayed fashion from the time of initial injury [5-7]. Early suspicion, diagnosis, and treatment before the onset of neurological sequelae are required.
In 2013, the American College of Surgeons proposed screening criteria for the investigation of patients with cervical spine injury in the Advanced Trauma Life Support® (ATLS) manual [8]. These criteria suggest that screening should be performed especially in patients with fractures of the first three cervical vertebrae, cervical fracture subluxation, and fractures through the foramen transversarium.
VAI can cause neurologic deficits due to posterior circulation stroke. Biffl and his colleagues reported that the respective rates of death and severe neurologic complications directly related to VAI were 5% and 8% [1]. To prevent the sequelae of VAI, several treatment strategies are recommended. The major treatments are anticoagulation therapy and endovascular therapy, but controversy still remains due to the lack of high-grade evidence.
The purposes of this study were to evaluate the effectiveness of the ATLS screening criteria and to establish an effective strategy to prevent subsequent posterior lesion infarction. This study is a retrospectively reviewed sequential case series from a single institution.
2. Materials & Method
Trauma patients with an Abbreviated Injury Scale (AIS) score of ≥3 in any body region who were treated at the trauma and critical care center in Osaka City University Hospital were included in this study.
The patients’ clinical records were retrospectively investigated, and the following data were evaluated: computed tomography (CT) with or without enhancement on admission, evidence of cervical spine injury, VAI, treatment for these injuries, and outcome.
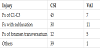
The injury pattern of each VAI was graded using a grading system previously proposed in 1999 that is based on the angiographic findings (Table 1) [9].
3. Results
3.1 Diagnosis of VAI
From 2007 to 2017, 1627severe trauma patients with AIS score ≥3 were admitted to our department, and 114 patients were diagnosed as having cervical spine fracture or subluxation. Contrast-enhanced whole-body CT was performed in 82 patients, and 13 patients were diagnosed as having VAI by CT angiography (CTA) (Table 2). Among these 114 patients, 73 met the ATLS screening criteria for investigating VAI, and all were investigated using enhanced wholebody CT scanning.
Among the 73 patients who had at least one of the three injuries mentioned in the screening criteria, 12 patients had more than two injuries, and these 12 patients (16.4%) had VAIs. Thus, all but one of the 13 patients diagnosed as having VAI by CTA (92.3%) had injuries meeting one of the VAI screening criteria (Table 3). Among the three injuries of the screening criteria, fracture of the foramen transversarium (41.7%) had the highest morbidity for VAI, followed by fracture with subluxation (36.7%) and fracture of C1-C3 (15.6%). The injury in the patient who did not have any of these three injuries was a fracture of the C7 spinous process.
3.2 VAI grade
The 13 patients had 16 VAIs, with 11 VAIs of grade IV (68.8%), four VAIs of grade II (25%) and one VAI of grade I (6.3%). There were no injuries of grade III or grade V. Two patients had either grade I or II VAIs. One had a unilateral grade I injury, and the other had bilateral grade II injuries. There were 11 grade IV VAIs in the 11 patients, and two patients had grade II injury on the opposite side.
3.3 Treatment of cervical spine injury and VAI
Among these 11 patients, seven patients had a dislocation or fracture of the spine between C3 and C6 and required urgent operation. Prophylactic coiling to completely occlude the injured vertebral artery was performed before the operation or reduction in four patients. In case #7, angiography was performed for prophylactic coiling, but it was technically impossible because the occlusive lesion was very close to the root of the right vertebral artery. Prophylactic coiling was not selected in two patients based on the physician’s decision.
Heparin infusion as the antithrombotic therapy was performed in all but one patient, and accordingly no patient experienced an infarction. In the other four patients with grade IV VAI, one had a grade II VAI on the opposite side. Three of them received antithrombotic therapy, but the remaining patient with bilateral VAIs could not receive antithrombotic therapy due to a subdural hematoma. This patient was also complicated with cerebellar infarction on the second hospital day. Thus, antithrombotic therapy was performed in 9 patients and not performed in 4 patients due to other concomitant organ injuries. Two of the 13 VAI patients suffered subsequent cerebellar infarction.
Case #2 showed bilateral grade II injuries in an 84-year-old man who had fallen down the stairs and showed quadriplegia. Cervical CT revealed a C3 spinal fracture and subluxation between C3 and C4. Head CT showed a subdural hematoma, and vertebral angiography revealed the bilateral Grade II injuries. Because the left VAI had an unstable intimal flap and severe stenosis, endovascular stenting was performed to prevent distal embolus. Antithrombotic therapy was not performed due to the subdural hematoma. The CT scan on the next day revealed a low-density area in the right cerebellum. It was hard to diagnose whether this infarction had occurred before or after the endovascular treatment because he has shown no symptoms of cerebellar infarction.
Case #3 was a complicated cerebellar infarction in a 72-year-old man who was hit by car and thrown about 4 meters while walking on the street. Whole-body CT scan revealed traumatic subarachnoid hemorrhage, a small subdural hematoma, and fractures of the right ribs and femur. A right grade IV VAI was noted on admission, but antithrombotic therapy was not started because of the traumatic brain injury. Re-canalization of the right vertebral artery and an infarction lesion in the right cerebellum were observed on CT scanning on hospital day 19.
These two patients with cerebellar infarction had bilateral VAIs, and neither received antithrombotic therapy due to traumatic brain injury.
4. Discussion
The frequency of VAI in this study was 0.8% (13 of 1627), which corresponds to rates reported previously [1-3]. Clinical symptoms of VAI, such as headache, dizziness, nausea, vomiting, sensory and gait disturbance, speech and visual abnormalities, and altered consciousness, are attributed to ischemia of the posterior circulation. However, most unilateral VAIs are initially asymptomatic, and symptoms develop in a delayed fashion from the time of the initial injury [5-7]. Thus, early diagnosis and treatment before the onset of neurological sequelae is required.
In the diagnosis of VAI, digital subtraction angiography (DSA) has previously been considered the gold standard [10]. DSA can provide high-resolution images of injuries and detect subtle intimal defects. DSA also affords the opportunity to undertake endovascular treatment if necessary, and it may detect blunt cerebrovascular injuries in up to 34% of asymptomatic patients with blunt trauma [10,11]. However, it is invasive and also carries the risk of iatrogenic injuries.
DSA also has limitations in terms of expense and availability. Thus, it is currently usually reserved for patients with uncertain noninvasive imaging findings or with a clear indication for a therapeutic endovascular procedure. Other modalities such as magnetic resonance imaging and CT are less invasive but historically have shown poor sensitivity compared to DSA [12,13]. However, CTA using a multi-row scanner has recently shown encouraging results. Both 16- and 64-slice CTA are reported to have greater than 95% sensitivity and specificity [3]. We evaluated the VAIs in the present study with a 64-slice CT scanner.
The rate of VAI was 92.3% in the patients who met the ATLS screening criteria and was comparable to that previously reported [3]. The only injury that did not meet the criteria was the injury to the C6 spinous process. From the present study, we recommend not only the three criteria proposed by ATLS but also that any fracture or subluxation might be an indication for the screening of VAI. Further studies are required to evaluate the screening criteria.
There is no high-level evidence on the management of the various grades of VAI. The options for treatment include observation, antithrombotic therapy, endovascular therapy, and open surgery. In addition, the morbidity rate from stroke does not correlate with the injury grading. In patients with VAIs, grade II injuries have the highest reported morbidity rate, ranging from 14% to 40% [5,12,14]. The patients in the present study with subsequent cerebellar infarction had grade II injuries. Furthermore, the grade of VAI may change as the clinical course progresses. More than 40% of grade II VAIs were reported to progress to grade III [12].
Antithrombotic therapy is the widely recommended therapy except for grade V VAI. Retrospective studies showed that antithrombotic therapy reduced the risk of ischemic neurological sequelae [5,12,14]. However, as patients with VAI have often suffered polytrauma, about one-third of the patients with cerebrovascular injuries could not receive systemic antithrombotic therapy [14,15].
Antithrombotic therapy includes anticoagulation therapy and antiplatelet therapy. Several studies suggested that systemic heparinization and antiplatelet therapy are equally efficacious in the prevention of stroke [1,11,15,16]. Biffl and his colleagues have recommended using intravenous heparin to achieve a partial thromboplastin time of 40 to 50 seconds. Bleeding complications due to systemic heparin were observed in 4% of patients [12]. As antiplatelet therapy, aspirin 325mg daily and/or clopidogrel 75mg daily is recommended [1,16].
The duration of antithrombotic therapy is controversial, but some papers recommend3 to 6 months of therapy [17,18]. However, as ischemic sequelae usually occur within 2 weeks after injury, an adequate duration of anticoagulation therapy might be about 2 weeks. Patients in whom anticoagulation therapy is usually chosen are then converted to warfarin titrated to a prothrombin time.
At our institution, we use intravenous heparin first for antithrombotic therapy. As most of the patients with VAI have other concomitant injuries, if bleeding complications do occur, intravenous heparin offers more safety because it can be acutely reversed.
In this case series study, two of the 13 patients with VAI showed cerebellar infarction. However, none of the VAI patients who received antithrombotic therapy showed cerebellar infarction, indicating that anticoagulation therapy appears to be effective in reducing ischemic complications. The two patients with bilateral VAIs showed cerebellar infarction, so we can see that bilateral VAI is one of the risk factors for subsequent stroke and neurological deficit.
Endovascular therapy is especially considered in VAI of grades II to IV. Options include stenting, occlusion of the vertebral artery, and coil embolization of the pseudoaneurysm [11,18] (Figure 1). Because VAIs are accompanied by cervical spine fracture, subluxation, or dislocation, urgent operation for reduction or fixation would generally be performed to prevent secondary injuries to the contused spinal cord and to improve motor and sensory disturbances. However, these manipulations can dislocate the foramen transversarium and might re-canalize flow in the vertebral artery that could push on any thrombus present, which could potentially completely occlude the posterior circulation. Embolization of a completely occluded grade IV VAI with coils might be effective in preventing distal embolization and infarction. In some small case series, coil embolization was reported to be effective in preventing infarction [19,20]. None of our patients who received coil embolization were complicated with cerebellar infarction.
5. Conclusions
ATLS screening criteria have high sensitivity for the diagnosis of VAI. However, further studies are required to evaluate these screening criteria. The risk factors of subsequent cerebellar infarction are bilateral VAI and not receiving anti-thrombotic therapy, which might be effective and recommended unless contraindicated. Coiling of the obstructed vertebral artery might be effective in preventing thrombus in the distal arteries and subsequent infarction. However, a randomized controlled study would be required to evaluate the efficacy of this endovascular treatment. As this was a single-institution, retrospectively reviewed study, further multi-institutional studies will be required to evaluate these outcomes.
Competing Interests
The authors declare that they have no competing interests.
Author Contributions
Fumiaki Wakita contributed to the design of the study, analysis and interpretation of the data, and writing of the article. Maiko Esaki contributed to the design, analysis, and interpretation of the data. Kenichiro Uchida contributed to critical revision of important contents. Yasumitsu Mizobata made substantial contributions to the conception and design of the study and to revision of the intellectual content. All authors gave their final approval of this version of the manuscript for publication.