1. Introduction
Post-thyroidectomy neck hematoma belongs to the most dangerous complications in thyroid surgery. It leads to respiratory distress by airway obstruction, and, if diagnosed and treated too late, subsequently severe brain damage may occur or at worst can lead to death. Intraoperative effective hemostasis is an important goal for every surgeon to prevent this life-threatening complication. In the early days of thyroid surgery bleeding was generally a major problem [1]. Samuel Gross, Professor of Surgery at Jefferson Medical College in Pennsylvania described the state of thyroidectomy in 1866 “a horrid butchery”. Emil Theodor Kocher was the first surgeon using precise surgical techniques for hemostasis and reduced mortality rate from 45 % to about 0.5 % in more than 5000 thyroid operations [2] (0.18% in about 7000 thyroid operation [3]). Nowadays, postoperative neck hematoma occurs in approximately 1 % after thyroid surgery [4] and the majority of these events happens in the first 6 hours [4]. About 20% occur 6 to 24 hours postoperatively [5]. Neck hematomas after 24 hours, as in our case, are rare [6]. In case of neck hematoma after surgery accompanied by respiratory distress, immediate protection of the airway by intubation is essential before reoperation. Sometimes even emergency “bedside evacuation” of the hematoma is necessary and protects the patient from fatal outcome. Intubation should be performed by the most experienced anaesthesiologist available, because significant edema of the epiglottis and the arytenoid may allready be present [7]. In our hospital we strongly recommend patients to avoid physical strain after thyroidectomy for 2 weeks. Till now no case of late hematoma (more than 24 hrs) after thyroid surgery is reported, according to our hospital data.
2. Case Report
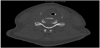
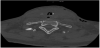
In a 56-year-old healthy female, 10 days post hemithyroidectomy and ipsilateral parathyroidectomy on the right side, a swelling of the neck, in terms of post thyroidectomy bleeding developed within a short time period during the night. Surgery was performed in another hospital and right afterwards the patient was on holiday for skiing in a mountain skiresort about 100 km away from our tertiary hospital. At about 3:00 in the morning the patient awoke because of a feeling of tightness in her throat but went on sleeping. About 2 hours later she awoke again, the tightness in her throat was much more intense, breathing and swallowing became harder. She also noticed a swelling of the neck and emergency doctor was called. At the arrival blood pressure was 141/84, pulse 106; SpO2 93%. The emergency doctor treated the patient with prednisolone 250 mg, 10 mg metoclopramide hydrochloride and 5 mg tropisetron. At departure to hospital blood pressure was 166/74; pulse 93; SpO2 98% with oxygen (2l/min). No attempt of intubation was made at that time. As helicopter transport was not available during night, the patient had to be transported on ground for 100 km. On arrival in our clinic the patient presented with swollen neck, hard breathing and almost unable to swallow and speak. The emergency team of our hospital was called immediately by the endocrine surgeon and intubation could be managed luckily under provision of technical assistance with videolaryngoscopy and in standby for evacuation of hematoma and tracheostoma bedside. During following evacuation and exploration of the neck in the operating theatre, arterial bleeding of a branch of the inferior thyroid artery could be detected and closed by ligation. After operation a computed tomography was performed. It showed the lumen of the trachea in the neck area just kept braced by the tubus, the surrounding structures, larynx, hypopharynx and parts of the oropharynx heavily edematous as shown by figure 1, 2, 3 and 4. The following treatment took place in the intensive care unit. Medication with prednisolone 500 mg on the first day, 250 mg on the second day, and cryotherapie was applied to reduce edema. Frequent control examinations of otorhinolaryngologists were performed to verify reduction of swelling and to evaluate the possibility for safe extubation. Three days after the event the attempt to remove the tracheal tubes, again with standby of an otorhinolaryngologist, succeeded. Laryngoscopy before extubation showed reduced swelling in the area of the supraglottis, epiglottis and the aryepiglottic plication to the arytenoid. Additionally, hematoma without swelling on the rear of the throat and severe hematoma of the vocal cords was found. The patient stayed another day under observation at the intensive care unit. On the fourth day the patient was transfered to the intermediate care unit of our department because she was still not able to cough up residual secretion out of the respiratory tract. On the next day clinical status improved and she was transfered again to normal ward. Another laryngoscopic control showed partial remission of the hematoma of the vocal cords. Seven days after the event the patient could be discharged from hospital (Time table).
3. Discussion
Now a days neck hematoma occurs in approximatly 0.1 % to 1.1 % after thyroid surgery [5] and late post-thyroidectomy neck hematoma is an absolutely rare event. New surgical techniques and especially improvement of devices for sealing vessels help to avoid post surgical bleeding. Operating strategies are reconsidered to minimize morbidity. For example, some studies advise against prophylactic central neck dissection in case of differentiated thyroid carcinoma less than 10 mm of diameter and clinically lymph node negative, because it may increase postoperative complications without any demonstrable benefits in terms of long-term survival [8,9]. Structured postoperative monitoring of the patients leads, in case of hematoma, to early diagnosis and treatment in clinical setting. However, as a result of this dangerous complication a rare number of patients suffer from apallic syndrome per year. Cough, valsalva maneuver [10] and also physical strain-for example carring heavy luggage -leads to high pressure in the vessels of the head and neck causing after bleeding. This can also happen by rapid movement or accidents in sports. In the guidelines of our endocrine unit we recommend to refrain from physical strain for at least 2 weeks after thyroidectomy. Because the outcome of bleeding after thyroidectomy is much worse and life-threatening outside of clinical setting, and often initially a result of underestimation by physicians because of lack of experience with a long approach to expert help. In this case report the patient recovered luckily without any related complications and long-term health damage.
4. Conclusion
Post-thyroidectomy neck hematoma evolving more than 24 hours after surgery is rare. Outside of clinical setting misinterpretation of the situation and long approach to expert help may lead to major complications and even death. Immediate protection of the airway by intubation is essential.
Competing Interests
The authors declare that they have no competing interests.