1. Introduction
Advances in health technologies have led to the development of a variety of therapy robots for use in rehabilitation. In particular during the past decade there has been a rapid increase in the number of robotic devices that are being developed to assist movement rehabilitation of the upper paretic extremity resulting from brain injury [1]. They were introduced in rehabilitation settings by neurorehabilitation specialists who recognized that there is no proof of any one therapy's superiority over the others [2]; rehabilitation of the motor function of upper limbs is expensive and labor-intensive and upper-limb robot devices can be valuable additions to a therapist's treatment in order to deliver large doses of motor training in a cost effective manner.
2. Impairments
Functional improvement of the upper paretic limb after Acquired Brain Injury (ABI) is determined mainly by motor recovery of the paretic hand [3,4].
In the early stage of brain injury, the normal resting tone on more affected side is diminished, muscles are unable to produce adequate force even for the smallest of movements, there is often a loss of automatic control, decreased tactile sensation and diminished proprioception [5].
Physiologic and anatomical changes occur in muscles and soft tissues since acute phase [6] resetting them to a shortened position [6,7]. The most common functional consequence of this, is the development of joint contractures and increased tissue stiffness [8,9].
The combination of altered sensation, decreased motor control, weakness and stiffness of the hand and arm may impact on the performance of daily activities and cause swelling or Oedema of wrist and hand [10-16].
A recent study has found swelling of wrist and hand in 72,7 % of 88 patients with Stroke and oedema in 33% [9].
Isolated Oedema of upper limb after stroke has received little attention in the scientific literature and the aetiology remains unclear. Geurts [13] stated that oedema is not a limphoedema[17].
Its development reasons are therefore more likely to be a changed microcirculation with an imbalance in the filtration and reabsorption mechanism[17]. If the oedema persists the initial fluid accumulation could progress into limphoedema.
Oedema is accompanied by heaviness, stiffness, reduced active motion [14,15,18,19] and may cause additional problems like diminishing functioning and occurrence of shoulder-hand syndrome thus interfering with the rehabilitation process [13,19,20].
3. Conventional Treatment Approaches
Conventional treatment approaches for rehabilitation of the hand functions usually employ different kind of techniques. Recent studies have found botulinum toxin, nerve block, stretching programs to be effective in the management of tissue shortening and in the decreasing tone [5,21,22]. Intermittent pneumatic compression, neuromuscular nerve stimulation and continuous passive motion seem to be useful in the management of upper limb swelling and oedema [14,15,18,19]. Moreover there are evidence that task specific training, constraint induced therapy, extrinsic feedback, action observation, robot devices and virtual reality technologies are helpful to promote recovery of motricity and skills acquisition [2].
But the most favorable therapy has not yet been recognized [2] and several studies pointed out that upper limb motor re-learning and recovery levels tend to improve with intensive physiotherapy delivery [23].
3.1 Robotics Upper-Limb Devices
In view of the observations described above, robotic upper limb rehabilitation devices have the potential to deliver high intensity therapy in a cost effective and easily reproduced manner [23].The robot devices can allow completion of movements throughout the range of motion, monitoring patient performance and adapting therapy intensity and difficulty after each session thus preventing inappropriate movements [24].
Robotic upper limb devices that are well tolerated by patients can be used in both acute and post acute settings and be a valuable addition to conventional approaches.
Studies with robots upper limb devices have demonstrated improved proximal arm function after cerebral injury [24-27] although these improvements did not transfer to the distal arm function which is necessary for most activities of daily living [28-30]. Robot-assisted training which specifically targets the hand might be required to achieve significant improvements in hand function. Furthermore, several studies indicate a generalization effect of distal arm training, e.g. hand and wrist, on proximal arm function, i.e. elbow and shoulder, which may lead to improved control of the entire arm [29,31,32].
In our rehabilitation unit we had the opportunity to experience using the Gloreha hand device that provides computer-controlled, repetitive, passive mobilization of the fingers through hand gloves connected with the machine, which re-elaborates a visual feedback of the moving hand on a computer screen.
We therefore focused on the improvement of upper limb function adopting a rehabilitation approach based on the combination of robot hand mobilization and manual therapy delivered by therapists.
The current study tested whether additional Gloreha hand mobilization, could maintain range of motion, could decrease edema and spasticity and improves movements of upper-limb.
4. Methods
4.1 Subjects
Twenty-seven subjects were enrolled for this study that conformed to the ethical principles set forth in the Helsinki Declaration of 1975 and revised in 1983. Before beginning, all subjects or legal representatives for the incapacitated subject signed a consent form.
Subjects presented slight to severe residual arm impairment post acquired brain injury.
Inclusion criteria were: subjects aged between 18 and 99 years who were at most 100 days post acquired brain injury with a Level of Cognitive Functioning Scale (LCFs) > 4, a low level of spasticity of the upper-limb with Motor Tardieu Scale (MTS
LCFs is one of the earlier developed scales used to assess cognitive functioning in post-coma patients [33].
MTS was used to measure spasticity. The therapist quantified the resistance to passive movement at three different speed definition (V1: slow as possible; V2: speed of limb falling under gravity; V3: moving as fast as possible) and defined the quality of muscle reaction, the angle of muscle reaction (R1) and the full range of motion (R2). Subject was tested in sitting position [34].
MLT were used to provide information regarding whether the limitation in the hand movement range is due to shortness or adhesion of the respective muscle and/or tendons. The therapist tested the subject in sitting position and followed procedure-testing described in literature [35]. Exclusion criteria were medical or functional control indications, upper limb poor skin condition over hand and wrist; other vascular cerebral events in anamnesis and/or neurological disease.
4.2 Gloreha
Gloreha (System idrogenet srl) is a novel robot designed for clinical neurological applications. It was developed to train the ability to grasp and release objects through a smooth passive mobilization of the hand.
Weight and multy-sensorial stimulation are the key features of this device. Metacarpo-phalangeal, proximal and distal interphalangeal articulations are moved through a light weight glove which is connected to a column chassis where five electrical actuators are placed; mechanical power is transmitted by bundle of 5 chords to the glove. The Mobilization can be linked to sight and hearing stimulations or driven on a object. A touch screen PC can be used as a control panel or a 3D interface and it can produce hearing effects. Gloreha device is safe, flexible and customizable, intuitive, easy to use and fast to set-up.
For this reason it can provide a simplified, low cost version intended for patient use at home. A more complex and more adaptable professional version (Gloreha Professional) has been produced for hospitals and rehabilitation centers (survey on robot rehabilitation).
Six simple exercises are implemented on Gloreha:
- First: flexion-extension of the individual fingers in order, from thumb to little finger;
- Second: functional movements with the fingers to count from one to five;
- Third: pinching;
- Fourth: flexion from the little finger to the thumb, and extension from the thumb to the little finger, to create a flowing wave effect; Fifth: flexion-extension of the whole hand;
- Sixth: individual and simultaneous finger flexion / extension in the order chosen by the therapist.
4.3 Sperimental protocol
In this randomized controlled cross-over trial (figure 1) with two sequence, two period, and two treatment (AB/BA design), we randomly (simple randomization) assigned twenty-seven subjects in two groups. The first group received robot assisted therapy plus conventional therapy in the first week and then only conventional teraphy in the next week (Group 1) and the second one (group 2) received only conventional therapy in the first week and conventional teraphy plus robot assisted teraphy in the second week. Each subject received 2 weeks of treatment.
Robot assisted therapy consisted of five 42-minutes sessions (seven minutes for each exercise); intensive therapy consisted of five1-hour sessions of muscular realignment, stretching, sensory stimulation, active-assisted mobilization, trunk realignment, functional exercises.
4.4 Clinical outcome measures
A therapist blinded to the group assignment, tested all subjects with a battery of clinical evaluations immediately before the start of treatment (pre_tx) and immediately after the end of treatment (post_ tx).
The primary outcomes were a change in Volumetric Measurement of the hand. The secundary outcomes were a change in Upper Limb Motricity Index, in range of motion (ROM), in MTS and MLT.
Hand volumeter was used to measure the presence, the severity and the evolution of hand swelling. The volume of the paretic hand derived from the water displacement, was compared with the volume of the non paretic hand in order to establish the presence of swelling. Water displacement is a common measurement in physical therapy practice [36-39], and is both reliable and highly correlated but not interchangeable [40,41]. The therapist followed these indications to measure reproducibility: hand immersion in the water filled-volume until the lister's tubercule; water-temperature ranged between 20°- 30°; weighing the water gap on a balance to determine the volume of the hand.
Goniometric measurements of the hand were used to quantify range of motion. The therapist followed a standardized procedure [42] and obtained wrist joint angles and fingers (middle finger and thumb) joints angles.
Upper Limb motricity index test (ULMI)[43] was used to quantify muscle weakness of the upper extremity. The upper extremity motricity index includes three actions: pinch grasp, elbow flexion, shoulder abduction. Each action scores 0-33 according to the instructions of the author. The total score is obtained by the sum of three actions; maximum score is 100.
4.5 Data reduction
To further investigate the prevalence of swelling and oedema in our sample we defined the degree of swelling as a positive difference in volume between paretic (P) and non paretic hand (NP), expressed as a percentage of volume of the non paretic hand [10].
Any volume difference indicated some degree of swelling (percentage larger than 0). We defined oedema as a volumeter score that deviates by more than 2 SD from the expected score [44]. Pinchgrasp portion were extracted from the ULMI for statistical analysis.
To analyze data outcome the values of post-treatment for each subject were subtracted from the corrispondent values pre-treatment (post_tx- pre_tx). This difference was called Delta (Delta= post_txpre_ tx) for each outcome measure (delta volume, delta range of motion, delta ULMI and delta pinch-grasp). A negative delta volume, a positive delta range of motion and a positive delta ULMI represented good measurements.
4.6 Statistical Analysis
The following findings would support the hypothesis that Gloreha therapy plus intensive therapy should show a greater improvement than intensive therapy only.
Baseline differences between groups were evaluated with Mann- Whitney test (continuous and ordinal data) and chi-Square (categorical data). Several statistical procedures were used to test differences in improvement over time between the two groups. The statistical tests used depended on the type of measure. A T-test for independent data was applied if rating scales were continuous and met the assumption of normality (Anderson-darling test for normality) and a T-test assuming unequal sample variance was calculated when homogeneity variance of sample was not respected. A Mann-Whitney test was applied on ordinal data and when rating scale did not met the assumption of normality. McNemar's test was applied on binomial data as recommended [45].
T-test and Mann-Whitney were applied to investigate carry-over effect, treatment-effect and period-effect. McNemar's test was applied on binomial data in order to analyze treatment-effect.
The level of significance (P) was set at 0.05 for each outcome.
5 Result
A total of 27 patients met the inclusion criteria, consented to participate, completed the baseline assessment and were randomly allocated to receive Gloreha therapy plus intensive therapy and intensive therapy. One subject whitdrew from randomization because an error in the initial evaluation of inclusion criteria in the anamnesis. Two subjects whitdrew from treatment because of a decline in cognitive status and did not participate in the assessment after the first week. 24 subjects completed the intervention and participated in the assessment. One additional subject was lost during the analysis because of data conflict due to diabetic pathology.
Thus the data from 23 subjects was used to perform the analysis on baseline characteristics.
In Table 1 the baseline characteristics and baseline intake values of all dependent variables are presented for all subjects and combined for group 1 and group 2 separately. Baseline characteristics and intake values for all dependent measures of subjects in group 1 did not differ significantly from those of group 2 in term of age, months post Cerebral Vascular Accident (CVA), sex, side of lesion, etiology, hand volumeter. Group 1 did differ significantly from the group 2 in terms of range of motion of flexion and extension of fingers methacarpusphalangeal joint.
5.1 Prevalence of swelling and oedema
Following the definition from literature previously reported, in our sample swelling was present in 78,3% of all patients, oedema was present in 13,04%.
5.2 Carry over effect
Significance tests for carry-over effect did not reveal significant differences between carryover effects of the two groups in terms of hand VOLUMETER , Upper Limb motricity index, pinch grasp and goniometric measurement except for the flexion of the thumb metacarpal-phalangeal (P= 0,048) (Table 2). In this case we discarded data from the second period and analyzed only the data from the first period as if from a parallel group trial (treatment effect) as highly recommended [45]. Table 2 summarizes the clinical outcomes in relation with carry over, treatment and period effects.
5.3 Treatment effect
Significance tests for treatment effect did reveal significant differences in hand volumeter, in inter-phalangeal extension and methacarpus phalangeal flexion of the thumb (Table 2).
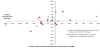
Each individual’s measurements of hand volume on the two treatments are shown in a scatter-plot (figure 2).
Hand Delta volume measurements for the 11 individuals in group 1 are shown with delta volume measurements for the 12 individuals in group 2. The line of equality (measurement after Gloreha therapy plus intensive therapy= measurement after intensive therapy) is superimposed on the plot.
The hand volume mean of group 1 after Gloreha therapy plus intensive therapy (first week) was -17.56 ml. The hand volume means of group 1 after intensive therapy (second week) was 9.77ml.
The hand delta volume mean of the group 2 after intensive therapy (first week) was -5.82 ml. The mean of the group 2 after Gloreha therapy plus intensive therapy (second week) was -15.23 ml. These means are displayed in a plot (figure 3).
The mean of interphalangeal extension of the thumb of group 1 after Gloreha plus intensive therapy (first week) was -0.91°. The mean of interphalangeal extension of the thumb of group 1 after intensive therapy (second week) was 1.36°.
The mean of interphalangeal extension of the thumb of group 2 after intensive therapy (first week) was 1.25°. The mean of interphalangeal extension of the thumb of group 2 after Gloreha plus intensive therapy (second week) was -0.83°.
The mean of methacarpus phalangeal extension of the thumb of group 1 after Gloreha plus intensive therapy (first week) was -2.18°. The mean of methacarpus phalangeal extension of the thumb of group 2 after intensive therapy (first week) was 1.17°.
5.4 Period effect
Significance tests for period effect did reveal significant differences in term of range of motion of flexion of the wrist.
The mean of flexion of the wrist of group 1 after Gloreha plus intensive therapy (first week) was 0.091°. The mean of flexion of the wrist of group 1 after intensive therapy (second week) was -1.45°.
The mean of flexion of the wrist of group 2 after intensive therapy (first week) was 5.33°. The mean of flexion of the wrist of group 2 after Gloreha plus intensive therapy (second week) was – 1.58°.
6. Discussion
Our study focused on the possibility to achieve an improving in hand volume, of paretic upper limb of patients undergoing Gloreha treatment in addition to conventional treatment.
Data from 23 patients was analyzed in order to verify these hypotheses.
Subjects in our sample were mostly characterized by a low level of spasticity, no shortness or adhesion of muscle and/or tendons, normal range of motion of joint of the hand, and the primary motor impairment was decreased motor-unit activation (table 1).
These characteristics were quite similar to these found in literature: initial muscles weakness or paralysis followed by secondary adaptive changes like muscle stiffness and length-associated changes.
About incidence and prevalence of swelling and oedema the literature shows extreme variability most probably due to differences in definition of oedema, study populations and measures [10]. In literature a complete definition of oedema is not recognized and is missing an hand volume classification in order to assess it. The physiotherapist can observe a different paretic hand conformation who appears more swollen than the opposite, but the reliability and accuracy of the visual inspection is unknown [10]. Volumetric assessment is recommended even if a clear cut-off point to determine oedema from the degree of swelling is not available. For all these reasons we choose the cut-off point introduced in a previously paper [10] of 2 SD of the population distribution. According to this definition in our sample swelling was very common and found in 78.3%,while the oedema was 13.04%. The prevalence of oedema in our sample was quite different from that found in literature [10], because the cut-off strongly depends from the population data. Our sample was not so numerous and the values were very scattered.
In addiction to conventional treatment, a program of robot assisted movements had the advantage of decreasing oedema after just one week of treatment in absence of a spontaneous improvement or of extended previous treatment effect. This observation was confirmed in T-test for treatment effect and showed a relevant influence on the oedema reduction in the group who had gloreha treatment in addition to conventional treatment, without a carry over effect and period effect, as described in Table 2. This result could have important consequences on the clinical approaches because a decreased swelling in paretic hand brings a higher possibility to avoid the pain, the stiffness due to adhesions, thickening, and shortening of connective tissue [10]. Moreover we know from the literature that oedema decreased active motion and disuse of the hand, so a positive effect on the oedema in paretic hand could lead to improving even on this aspects.
Even if the causes of the oedema are still not completely clear, for some authors swelling or oedema seems to be caused from the microcirculation modification [46,47] and could be responsible of an imbalance of pressure between the capillaries and tissue spaces [17]. Other authors state that oedema is only fluid accumulation at the beginning and will progress into linfoedema if the oedema persist [18,49,50]. Another hypothesis affirms that is a result of increased disuse due to the hemiplegia, that would be responsible for fluid accumulation because the muscle pump action is decreased [14,18,20].
Oedema management intervention reported in literature includes use of continuous passive range of motion machine [14,15]. Our results confirm that smooth passive mobilization of the hand with Gloreha, in addiction to conventional treatment, is helpful in reducing swelling on the affected hand in patients with hemiplegia.
This robot device can then be a support in daily practice in addition to the therapist’s treatment to achieve faster and better recovery of the hand in the intensive care unit, because we know from the literature that the intensity as well as task-specificity is the main drivers in an effective rehabilitation treatment program.
In our practice as physiotherapist we could also use this device before our treatment in order to lessens the swelling of the hand.
In daily living at home after the hospital the possibility of practicing with this robot device could maintain present in body schema the paretic hand and could allow better performance in the upper limb, because just 10 minutes specific input will regain the body maps for 24 hours [50]. On the opposite the sensory maps in the brain adapt within 12 hours negatively without activity [51]. The body schema in the parietal temporal lobe and in the cerebellum is the bases to generate motor output.
Despite of the considerations above, in our study there was not statistical evidence in the secondary outcomes (range of motion, muscle length, spasticity, motricity) between the two groups except for inter-phalangeal extention and methacarpus phalangeal flexion of the thumb, but the little modifications observed in these joints could be invalidated by error in goniometric measurement.
Our study is limited by little sample size and by the short period of observation. These limitations could have influenced the statistical significance in the secondary outcomes. Other studies could consider a longer time of evaluation in order to understand if a continuous passive motion with robot and a visual feedback could improve active movements.
7. Conclusion
The results of this cross-over study confirm that upper limb robot assisted passive mobilization, in addition to conventional treatment, is effective in reduction of swelling or oedema. These data may be useful for physiotherapists that treat patients in sub acute stage of recovery to prevent hand oedema and to achieve faster and better recovery of the hand in intensive care unit. Future research with longer time of observation and larger sample could show if this robot treatment could promote new muscles activations and new hand movements, that are essential in hand and upper limb recovery after ABI.
Competing Interests
The author declare that there is no competing interests regarding the publication of this article.