1. Background
Hepatitis C virus (HCV) is an enveloped virus with a 9.6 kb single stranded RNA genome. Six HCV genotypes and a large number of subtypes have been identified [1]. It is an important global health and economic problem. A hundred eighty million people are infected in the world [2]. On one hand, two thirds of the patients with acute HCV infection become chronically ill, and may progress to having liver cirrhosis (LC) in fifteen to twenty years. One to three per cent of patients with LC may have hepatocellular carcinoma every year [3]. On the other hand HCV may cause an extrahepatic manifestation such as mixed cryoglobulinemia, chronic kidney disease, porphyria cutanea tarda, and type 2 diabetes mellitus, rheumatoid –like nondestructive inflammatory arthritis and depression [4-6] (table 1). In addition to clinical outcomes, HCV has an important impact on economic burden through direct and indirect medical cost associated with managing liver disease, decreased work productivity [7]. HCV is associated with the increasing liver-related and all causes of mortality [8].
Both HCV and Chronic Kidney Disease (CKD) have a negative impact both on morbidity and mortality. Clinical use of Direct Antiviral Agents (DAAs) for the treatment of patients with HCV infection revolutionized the increase of sustained virological response (SVR), decreasing the duration of treatment and severe adverse events.
The aim of this article is to reveal the close relationship between HCV and CKD, and to review the studies related with the treatment of patients with HCV and different stages of CKD.
2. How HCV Infection Influences the Kidney
In one study, long-term follow-up of 5737 patients with HCV infection compared to 11228 healthy control patients showed that HCV was associated with the increase liver-related and all causes of mortality [9]. HIV coinfection, diagnosis of drug use, coronary artery disease, stroke, diabetes mellitus, peripheral vascular diseases, depression and anemia are independent risk factors for mortality [9]. In the Dialysis Outcomes and Practice Patterns (DOPPS) Study, 16720 patients which have maintenance hemodialysis were followed up for five years. The crude 1 year mortality rates were found 6.6 % in Japan, 15.6 % in Europe, and 21.7 % in the USA [10]. In one metaanalysis, which has 14 observational studies, Anti-HCV antibody was found to be an independent and significant risk factor for death in 145,608 patients on maintenance hemodialysis. Adjusted relative risk for all causes of mortality was 1.36 (95 % CI; 1.25- 1.47) and also adjusted relative risk for cardiovascular mortality was 1.26 (95% CI; 1.10-1.45) [11].
In a nationwide cohort study from Taiwan, 9430 newly diagnosed HCV patients and randomly selected 37720 healthy people were compared in terms of incidence rate and incident CKD. It was found that the frequency of CKD was 1.66-fold higher in the HCV than the non-HCV cohort (5.46 compared with 3.43 per 1000 person per year). The risk for CKD in patients with HCV was higher in diabetes, hyperlipidemia and cirrhosis. This results showed that HCV infection is associated with the increased risk for CKD [12].
In a meta-analysis which has 18 observational studies, anti HCV antibody was found to be increased adjusted relative to the risk for all causes of mortality and all causes of graft loss in 133,530 unique renal transplant recipients. Adjusted relative risk for all causes of mortality was 1.85 with a 95% confidence interval; 1.49-2.31 (p<0.0001). Adjusted relative risk for all causes of graft loss was 1.76 (95% CI; 1.46-2.11; p< 0.0001) [13]. In another meta-analysis performed by the same study group, 8 observational studies, 105,462 unique patients with HIV and HCV were evaluated in terms of glomerular filtration rate, proteinuria. It was found that there was increased risk of reduced glomerular filtration rate (Relative risk 1.64 (95 % CI; 1.28-2.0; p<0.001) and increased risk for proteinuria, relative risk 1.23 (95 % CI; 1.18-1.28; P<0.001) [14].
According to United States Renal Data System, among 474,369 patients, 52,874 persons (11.1%) had a positive HCV antibody test results. It was shown that the patients with HCV were associated with a greater than twofold risk for developing end stage renal disease (adjusted hazard rate; 2.80 : 95 % confidence interval 2.43-3.23) [15].
3. How CKD Infection Influences HCV Infection
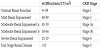
In order to standardize the terminology and decide better for the treatment, CKDs were classified by KDIGO [16].
The survival in patients with CKD, stages 1 and 2, is not different from that of the general population with normal kidney function. The 5-year survival for patients with CKD, stage 3, without HCV infection has been reported to be 76%, for patients with CKD, stage 4, 54%. Patients with CKD, stage 5, have a markedly reduced survival compared with the general population with normal kidney function [17].
A recent study showed that receiving the liver from Anti HCV positive donors to patients with HCV does not influence survival, and it is a safety procedure for long-term strategy. Besides that, it results in shortened waiting list of kidney transplantation [18,19].
In one meta-analysis, which has 14 observational studies, the risk for developing CKD/ESRD in 336,227 patients who have HCV infection was compared to uninfected 2,665,631 controls. It was found that the patients with HCV had a 23% greater risk for developing CKD/ESRD compared to uninfected controls. The risk ratio was 1.23 (95 %, CI; 1.12-1.34). In the subgroup analysis, increased risk for developing CKD/ESRD was found in both Taiwanese and US patients [20].
There is significantly increased risk of mortality, duration of hospitalization, anemia, pain, decreasing of quality of life in patients with end stage renal disease and HCV infection [21]. The prevalence of HCV infection in patients with chronic renal failure is higher (9.5% versus 1.6%) than with uninfected people. Those patients who have maintenance hemodialysis with HCV have also increased risk of mortality compared to uninfected ones because of not only liverrelated complications but also increased cardiovascular [22]. Because of those reasons, HCV infection in patients with renal impairment must be diseases treated. Before the treatment we have to be aware of those conditions:
- Level of fibrosis in the liver (F1-F6)
- Genotype of HCV (Genotype 1a, 1b, 2,3,4,5,6)
- Previous treatments (PEG-IFNs, PEG-IFNs+Ribavirin or Direct Acting Antivirals)
- Co-morbidity (HIV+HCV, HBV+HCV)
- Drug-drug interactions (Using of Protease inhibitors in liver disease, Sofosbuvir in CKD, Simeprevir and Calcineurin inhibitors)
- Kidney functions (Stage 2-5)
- Metabolic clearance of the drugs in order to treat HCV infection.
Sofosbuvir is eliminated from the kidney in 80%. When GFR is decreased less than 30 ml/min, Area under the Curve (AUC) increases by 456%. The dose of Sofosbuvir should be adjusted in CKD, stages 3-5. Dasabuvir is eliminated from gastrointestinal system by 90%. When GFR is decreased less than 30 ml/min, AUC increases by 50 %. Daclatasvir, Ledipasvir, Velpatasvir, Simeprevir, Ombitasvir and Elbasvir and Grazoprevir are eliminated mainly from the gastrointestinal system, and AUC will not be changed in renal impairments. Paritaprevir/Ritonavir is eliminated mainly from gastrointestinal system, 2% from the kidney. When GFR is decreased less than 30 ml/min, AUC increases by 114% [22].
When patients with HCV infection and CKD, stages 1-3, must be treated, it is not necessary to adjust the doses of DAAs. Those patients can be treated according to AASLD, EASL and APASL guidelines for HCV infection [23-25]. If patients with HCV infection and CKD, stages 4-5, are to be treated, we should be aware of elimination ways of the drugs, and we should choose them accordingly.
Four hundred and eight patients with HCV, genotype 1, were treated with the combination of Sofosbuvir 400 md/day and Ledipasvir 90 mg/day for 12 weeks. Seventy-three out of 408 had liver transplanted. Eighty-two % of 408 patients had chronic renal impairment with stage 2or 3. SVR rate was 95.9% [26].
In a comparative study, 1716 patients who had GFR> 45 ml/min were compared to 73 patients who had GFR< 45 ml/min in terms of effectiveness of Sofosbuvir 400 mg/day and Ribavirin 800 mg/day; and impact on renal glomerular functions. Seventy-three % of total 1789 patients had decompensated liver cirrhosis and forty-nine % of them had liver transplantation. SVR rates were similar, 82% and 83%. However, patients who had GFR<45 ml/min had worsened renal glomerular functions and anemia [27].
Treatment of fiftynaïve patients who are on hemodialysis were randomly treated with PEG interferon (n=25) and Classical interferon (n=25) for 48 weeks. SVR rates are 48% and 20% respectively (p=0.07). Withdrawal of treatments due to adverse events are 0% and 20% (p=0.04) [28].
Telaprevir-containing triple therapy had superior efficacy more than PEG-IFN/IFN/ and Ribavirin dual therapy [29]. But today due to common adverse events, those drugs are not recommended for the treatment of HCV infection.
Six patients with HCV, genotype 3, were treated with Sofosbuvir 200 mg a day, Daclatasvir 60 mg a day for 12 weeks. Two out of 6 patients had compensated liver cirrhosis, the other two patients had higher than 6,000,000 iu/ml HCV-RNA levels. SVR rate was 100% in this retrospective study [30].
Forty-seven patients with renal transplants were treated with sofosbuvir-based regimen. Fourteen sofosbuvir and Ribavirin for 24 weeks. SVR rate was 86%. Twenty-two patients were given sofosbuvir400 mg/day and Ledipasvir 90 mg/day for 12 weeks. Another 12 patients were given sofosbuvir400 mg/day, Daclatasvir 60 mg/day, Ribavirin (n=3) for 24 weeks. SVR rate was 100%. Anemia was seen in 57% of the patients [31].
Thirty-two patients with CKD, stage 3 (Glomerular filtration rate ≤60 ml/min ≥ 30 ml/min) were treated with Elbasvir 50 mg/day, Grazoprevir 100 mg/day for 8-18 weeks with or without Ribavirin. One out of four patients was compensated cirrhotic, 41% of them were co-infected with HIV. SVR rate for 12 weeks was 97%. There was no improvement of GFR in patients [32].
Two hundred fifty-four patients with HCV infection who had liver transplantation were followed up for 13 years. Chronic renal failure developed in seventy-six (30%) of them. HCV infection, Glomerular filtration rate before transplantation and being a woman are predictive factors for developing chronic renal failure. Diabetes Mellitus and use of calcineurin inhibitors are causes for developing renal failure. Fiveyear survivals were found 54.6% and 28.2% in patients who had not developed and had developed chronic renal failure respectively [33].
Three hundred and twenty-two patients with HCV,genotype1and CKD, stage 3b 5%,Stage 4-5; 2.5%, were treated with combination of asunaprevir 100 mg BID and Daclatasvir 60 mg/day for 12 weeks. SVR rates of Stage 3B and Stage 4-5 were 88% and 100% respectively. Two and one half % of patients discontinued the treatment. Baseline presence of NS5A resistance associated Variants, previous Simeprevir treatment, HCV-RNA levels before the treatment are predictors for SVR [34].
In a meta-analysis which has 11 studies,264 patients with HCV, genotype 1and CKD, stages 4-5 were treated with sofosbuvir based or non-sofosbuvir based regimens. The pooled SVR rate was 93.2%.
SVR rates of Sofosbuvir based and Non-sofosbuvir based regimen were 89.4% and 94.7% respectively. The pooled discontinuation rate was 2.2% [35].
Ten patients with HCV, genotype 1a, 1b and 4, were treated with PROD (Paritaprevir, Ritonavir, Ombitasvir and Dasabuvir) regimen. Seven out of ten patients had compensated liver cirrhosis, three patients had treatment experience. SVR rate was 100%. Eighty per cent of patients have side effects [36]. Twenty patients with HCV, genotype 1a (n=13), genotype 1b (n=7), and ESRD, were treated with PROD regimens for 12 weeks. SVR rate was 90%. One patient relapsed, one patient died from a reason other than a drug adverse event. Four patients had anemia because of Ribavirin treatment [37].
Seventeen patients with chronic renal failure (GFR< 30 ml/min) were treated with the combination of Simeprevir150mg /day and Sofosbuvir 400 mg/day for 12 weeks. Forty-seven % of patients were cirrhotic, 24% of them had F3 fibrosis of the liver. Seventy-six % of patients had genotype 1a. Four patients (24 %) experienced adverse events such as insomnia, headache and nausea [38].
Thirty-one patients were treated with the combination of Sofosbuvir 400 mg/day and Ledipasvir 90 mg for 12 weeks after kidney transplantation. SVR rate was 97%. Six patients who had proteinuria 500 mg/dl or more before the treatment had worsened proteinuria during the follow up [39].
Forty-six patients were treated with PROD regimen. Ten out of 46 (21.7 %) had CKD, stage 4; 30 out of 46 (78.2 %) had CKD, stage 5; 17 out of 46 (36.9%) had liver cirrhosis. Twenty-one (46%) patients received Ribavirin.SVR rate was 95.7%. Twenty-seven (58.6 %) patients received Erythropoietin. Twelve patients had anemia (Hb< 10 gr/dl). Two patients discontinued the treatment (4.3 %) due to congestive heart failure and atrial arrhythmias. Doses of the Tacrolimus, levothyroxine, Acenocoumarol were adjusted during the treatment of PROD regimen. When Immunosuppressives, Calcineurin inhibitors, anti- hypertensive, ACE inhibitors, and Calcium channel blockers were used together with PROD regimen, it was better to adjust the doses of those drugs [40].
In the C-Surfer study, 224 patients with HCV, genotype 1 and CKD, stage 4 or 5 were randomized to treat with the combination Grazoprevir 100 mg /day and Elbasvir 50 mg/day for 12 weeks. 179 patients (76%) were hemodialysis dependent, 122 patients (52 %) had genotype 1a, 189 patients (80%) were treatment naïve, 14 patients (6 %) were cirrhotic. SVR rate was 99%. Most common adverse events were headache, nausea and fatigue. One patient had relapse 12 weeks after the treatment [41].
A hundred and four patients with HCV (genotype 1, 52%, genotype 2, 16%, genotype 3, 11%, genotype 4, 19%, genotype 5 and 6, 2%) and CKD (stages 4 and 5) were treated with the combination of Glecaprevir (NS ¾ blockure) 300 mg/day and pibrentasvir (NS 5A blockure) 40 mg/day for 12 weeks. SVR rate was 98%. Four patients discontinued the treatment because of adverse events. But, three of them had SVR after following up 3 months [42].
4. Conclusion
HCV infection and CKD have a negative impact on each other on mortality and morbidity. The treatment with DAAs is effective more than 90% and safe in patients with HCV infection and CKD.
Competing Interests
The author declare that there is no competing interests regarding the publication of this article.