1. Introduction
In Turkey, the increasing cesarean section (C/S) ratio is an universal problem. Especially in south eastearn region and in lower social economics part of Turkey, C/S ratio is rised steadily. Although the epidural vaginal delivery protocol, the lack of practical experience of anesthesia and the overcrowded hospitals limit the capability of epidural anesthesia. In contrast to European and American hospitals, the cost of C/S does not differ in Turkey even though in private hospitals from the normal vaginal delivery (NVD). For this reason, the increased elective C/S ratio can’t be decreased especially in primary pregnancy. The fearness of vaginal delivery that is emphasized with cultural factors is a nightmare in pregnant women. The satisfaction of pregnancy and the being a maternity or family is not considered. Poor emotional health is associated with increasing childbirth fear and risk of depression, birth trauma and inability to interact positively with baby and meet infant development needs and can be stressor in couple relationship [1-11]. By the improving of technology, the social media aggravated this fear with some videos of normal vaginal delivery.
In obstetric clinics at Mersin Sehir Hospital, we try to give education by mid-wive intervention and the opportunity of plates with coach. The aim of this organization to emphasize the nature of vaginal birth and the capability of mother vaginal delivery with less fear , more controlled body and the knowledge about delivery and baby.
This study is a retrospective case-control study among women that visit obstetric clinics in Mersin Sehir Hospital, Turkey. The case and control groups have been choosen randomly. The first goal is the measurement of fear about vaginal birth, and prefered mode of delivery before and after the midwife intervention. The tendency to the C/S because of fearfull pregnant women may be decreased by midwife intervention. The pregnant women with childbirth fear more often prefer a C/S [12-14]. Not only the lowering C/S ratio is
our goal, but also the satisfaction of pregnancy, vaginal delivery and lowering flashback are in our first goal. The maternity is a sacred phase of human being and it shouldn’t be interrupted with unsatisfied experience in delivery. Secondary goal of our study was the number of visit of obstetric clinic in postpartum period. The mother wonders that something is wrong with baby or herself because of unsatisfied delivery. The effective and continuation of breastfeeding, the programming of future pregnancy in first month and the planning of next pregnancy with normal vaginal delivery are also secondary goals. Infact, unsatisfied delivery causes bad flashback which is the reason of discontinuation of breastfeeding. The planning next pregnancy in the puerperal period with vaginal delivery is affected with bad experience. Even though the future pregnancy is planned as C/S.
2. Methods
This is retrospective case-control study with sample size of 482 pregnant women in case group and 949 pregnant women in control group. All women was in their first pregnancies the 12 women from case group were discontinued the education and 42 women were undergo to the C/S because of fetal distress or cephalopelvic disproportion. 8 women from case group were unreachable after the delivery. In the control group, 23 women were excluded because of cholestasis and preeclampsia, 43 patients were lost during pregnancy or postpartum period. 12 women refused the filling of WDEQ-A questionnaire. To summarize; the pregnant women between 16-40 years old first pregnancy was included to study. Those women were integrated in midwife intervention in 3 sessions and 3-6 times pilates sessions with coach in obstetric clinics of Mersin Sehir Hospital.
3. Data Collection and Measurements
The completion of questionnaire about demographic characteristics was asked to women. The WDEQ-A was used to measure the antenatal childbirth fear [15]. Women scoring high childbirth fear (>66) were randomised to the case and control group [16]. The other midwife intervention was done after 1 month of delivery in case and control groups.
4. Statistic Analysis
The study was a retrospective case-control study among patients in the obstetric clinics, at Mersin Sehir Hospital. The data was analyzed with SPSS (Statistical Package for Social Sciences) for Windows 22.0 programme. The analysis of data was delineated in numbers and percentages. The relation between the group variations was analyzed ki-square test.
5. Result
The estimated child birth fear is 6-10% of all pregnancy which is common among the nulliparous as in parous [17-20]. This study is the measurements of subjective findings. The absence of recall and the analysis of emotion will cause the biases in some degree. But the bad experience during the pregnancy and delivery may affect the whole women’s life. We try to standardized the education programme for pregnant women to increase the normal vaginal delivery (NVD) numbers, be satisfied from pregnancy and NVD, to reduce the unnecessary recurrent visit of obstetric clinics, to encourage breast feeding, to support families for their future pregnancy.
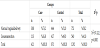
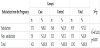
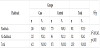
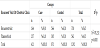
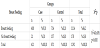
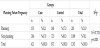
The study determined that the educational programme may encourage the pregnant women in the delivery room (as shown in Table 1). Instead, the cesarean ratio didn’t changed especially in planned pregnancy (as in Table 8). Especially in planned pregnancy, delivery route was chosen as cesarean section even in educated pregnant women. Besides, the midwife intervention satisfied women from pregnancy period and NVD (Table 2 and Table 3). Women felt the being mother during delvery by comparing with control groups. The nightmare or flashback recall during one month of peurperium was decreased by midwife intervention (Table 4). For this reason, the traumatic part of the delivery and pregnancy was regreded by the educational programme.
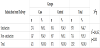
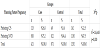
In the control group, the recurrent unnecessary obstetric clinic visit was detected because of questions about delivery and baby (table 5). In those visit the emotionally unsatisfied, scarred and doubtfull mother’s was observed. By means of midwife intervention, those traumatic factors was elected and happy mothers with happy babies were created. The emotional satisfaction effects the breast feeding positively, in the educated pregnant women the future plan and the happiness of being mother was showed by the high ratio of planning next pregnancy in contrast to control group (Table 7). Interestingly, the C/S ratio was not affected by the education, it was certain that, even though midwife intervention did not positively rised the desire of normal vaginal delivery (Table 8).
Surely, the case group didn’t want to undergo NVD in next pregnancy. The reason of this may be, although the education, traumatic pain of delivery which wasn’t decreased by the midwife intervention. Besides the positive effect of educational programme, the reality of normal vaginal delivery may have negatif consequences.
6. Conclusion
Midwife intervention should be professionally given to all pregnant women to encourage women for healthy mothers and babies but the C/S rate shouldn’t be designed by the educational programme.
Competing Interests
The author declare that there is no competing interests regarding the publication of this article.