1. Introduction
Gestational trophoblastic disease (GTD) is a spectrum of cellular proliferations arising from the placental villous trophoblast encompassing four main clinicopathologic forms: hydatidiform mole (complete and partial), invasive mole, choriocarcinoma, and placental site trophoblastic tumor [1] . It carries an incidence of 1 in 714 live births, with a higher incidence in the Asian population (1 in 387 live births in Asian women compared to 1 in 752 live births non-Asian women) [2].
A molar pregnancy is the most common type of GTD. There are two types – complete mole (75-80%) and partial hydatidiform mole (20-25%), differentiated by genetic and histopathological appearance. A complete mole is androgenic in origin, and is diploid. 90% of partial moles are triploid in origin, containing two sets of paternal haploid genes and a single set of maternal haploid genes. 10% are tetraploid or mosaic conceptions and considered neither normal nor viable [1] .
A molar pregnancy presents typically with symptoms such as abnormal uterine bleeding (80-90% in complete molar pregnancy, 75% in partial molar pregnancy) following a positive pregnancy test, uterus larger than dates (28%), hyperemesis (8%) as well as a typical snowstorm appearance on ultrasound. Other signs include an early miscarriage, hyperthyroidism, early onset pre-eclampsia or abdominal distension due to theca lutein cysts. Serum beta hCG levels are often above 100,000 mIU/mL in complete molar pregnancies and fetal heart tones are absent [3-6]. Serum beta hCG levels are above 100,000 mIU/mL in less than 10% of patients with partial moles [7-9].
If a molar pregnancy is suspected, the preferred treatment is by surgical evacuation of the uterus [10,11]. Cervical preparation prior to surgery is generally allowed [12] . However, the use of oxytocic infusion prior to completion of the procedure is discouraged due to the theoretical potential of an embolus disseminating the trophoblastic tissue through the venous system [13] . Anti-D prophylaxis is required following evacuation of a molar pregnancy. A diagnosis is confirmed by histology.
Subsequent follow up is individualized depending on the trend of serum beta-hCG values post procedure. There is a risk of persistent trophoblastic disease following surgery needing further treatment, mainly chemotherapy. The overall risk of needing further treatment is about 15% after a complete molar pregnancy and 0.5% after a partial molar pregnancy [14-19]. Studies have shown that once serum beta-hCG levels have normalized, the possibility of developing gestational trophoblastic neoplasm is very low [20,21]. Women who have completed treatment for GTD’s not requiring chemotherapy are advised to avoid pregnancy for at least 6 months and barrier methods are largely encouraged. 98% of women with a previous GTD will subsequently have a normal pregnancy. The recurrence rate is 1 in 80 [22] .
The single O&G cluster in this study involves two tertiary centers. Both hospitals have been around since the late 1800’s and later became one of the two major clusters to produce the many generations of current O&G Consultants. Previously, Singapore adopted the British system for training of its doctors but has since adopted the American Residency training system since July 2011. As this cluster consists of two of the three training centers for upcoming O&G practitioners in Singapore, it is essential to evaluate the knowledge of the current clinicians on the various diseases of the field, in this case, molar pregnancy.
Despite the rarity of a molar pregnancy, it is a treatable disease that carries a malignant potential. Thus, a clinical audit was set up to audit the clinical knowledge of O&G practitioners at Medical officer level and above. The audit tests the knowledge of each doctor regarding the incidence, clinical presentation, and treatment as well as followup of a molar pregnancy. The results reflect clinical knowledge of the clinicians regarding this disease which subsequently ensures good clinical practice and enhances patients’ care in the cluster.
2. Objectives
To discover the level of clinical knowledge and create awareness within a single cluster O&G doctors of medical officer level and above regarding molar pregnancy.
3. Materials and Methods
A questionnaire containing multiple choice questions (MCQ) and extended matching questions (EMQ) was created based on RCOG green-top guideline 38. There were a total of 15 questions on this questionnaire. The MCQ and EMQ included questions regarding incidence, presentation, management and follow up of a molar Pregnancy (complete and partial). The data collection was spanned over one month.
The questionnaire was distributed amongst O&G doctors (in the single cluster at Medical Officer level and above at random following verbal consent to participate in the audit. They were not given any forewarning prior to the distribution of the questionnaire. They filled in the questionnaire under observation to ensure no references were used. The questionnaire was then collected back and filed for data collection. The option of anonymity to name was provided. However it was compulsory to indicate the level of seniority on the questionnaire.
The collected questionnaires were firstly divided according to the different levels of seniority. The answers of each set of questions were manually inserted into a computerized spreadsheet using Microsoft Excel. It was then double checked to be correct before the data was subsequently collated using the available formulas that were available on the Microsoft Excel software (mainly the sum of a set of data or a group of doctors and its percentage according to the selected cohort).
4. Results
78 O&G doctors were enrolled into the study. Among them, 7 Basic Specialty Trainees (BST), 1 Clinical Associate (CA), 29 Residents, 11 Advanced Specialty Trainees (AST), 8 Staff Registrars, 2 Senior Staff Registrars (SSR), 7 Associate Consultants (AC), 7 Consultants (C) and 6 Senior Consultants (SC) participated in the audit.
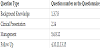
For the benefit of result interpretation, BST, CA and Residents are grouped together as “MO”, ASTs and Staff Registrars are grouped together as “Registrar”, SSR and AC are grouped together as “AC”, C and SC are grouped as “C”. Registrars level and above have obtained higher O & G qualification i.e. MRCOG or equivalent (Table 1-6).
For analysis purposes, the questionnaire is divided into 4 parts; background knowledge (incidence, predisposing factors), Clinical Presentation (including signs and symptoms), Management and finally Follow up.
5. Discussion
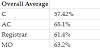
In this audit, all categories of doctors managed to score above 50% in the overall average (57.4% - 68.1%). This is to be expected as a molar pregnancy, albeit rare is a disease that should have been studied at medical school. Thus, all clinicians would at least have basic background knowledge of the disease. It is therefore reassuring that all categories of doctors are able to score above 50% in the overall average.
The AC group consisting of Associate Consultants and Senior Staff Registrars scored the overall highest of 68.1% in this questionnaire. This can be justified as clinicians in this group have just obtained their specialist qualification and thus are more up to date with the current clinical guidelines and protocols. They are usually the group of doctors who would have had the most exposure to various pathologies from hospital calls and inter-hospital referrals. From these calls, they are at the highest probability of seeing, diagnosing and managing a molar pregnancy.
The MO group scored second highest in this questionnaire with Registrar group following closely behind them. The two groups together encompass all O&G trainees in the cluster and they scored an average of 63.2% and 61.4% respectively. The MO group did better in the basic knowledge, management and follow up sections whereas the Registrars did better in the clinical presentation section. The MO group having younger clinicians who are closer to having recently graduated from medical school as well as the group of clinicians who are nearing and preparing for the higher examinations could justify this. They would have therefore been more up-to-date with the available clinical guidelines regarding the disease. The Registrar group however scored better in the clinical presentation part of the questionnaire. This is because they consist of the group of doctors who would have initially encountered patients suspicious with a molar pregnancy in a clinical setting in the early pregnancy unit. They would therefore be more aware of the clinical presentation of a molar pregnancy.
The group of doctors who scored the lowest in this questionnaire is the C group consisting of consultants and senior Consultants. Their overall average is 54.72%, over 10% below the AC group. The consultants and senior consultants not having constant clinical exposure to patients with molar pregnancy could explain this. Most patients suspicious of a molar pregnancy would present to the early pregnancy unit with a positive pregnancy test and abnormal vaginal bleeding. The Registrar and AC group of doctors largely manage these units. They may not be equipped with the up-to-date knowledge as a result of decreased exposure due to the rare occurrence of the disease.
Questions regarding clinical presentation received the most correct answers (83.3% to 94.9%) whereas questions regarding follow up received the most incorrect answers (21.8 to 70.5%). Most doctors would have been well educated regarding the clinical presentation of a molar pregnancy by the time they have left medical school. Therefore it is unsurprising that this bracket of questions returned the most correct answers. Follow up however is largely dealt with at clinical level, usually by registrar level and above. Molar pregnancies are followed upby this group of clinicians in the outpatient setting, following their histopathological diagnoses. However, due to the rarity of the disease, it is unsurprising that clinicians do not recall as accurately the follow up protocols and would need to refresh their memories with reference to the clinical guidelines.
Question 2 returned the most correct answers overall. This question is regarding the clinical presentation of a molar pregnancy. It is an EMQ question that asks for 3 signs or symptoms of a molar pregnancy. When calculated, 94.9% of the participants answered correctly. Correct answers include uterus larger than dates, positive pregnancy test, abnormal bleeding per vagina and an abnormally high serum beta-hCG. This proves that majority of clinicians are aware of the disease and its clinical presentation, which is reassuring as they are able to raise the suspicion of a molar pregnancy, should patients with the disease present to them in a clinical setting.
Overall, the question that had the most incorrect answers are question 13 and question 15 – both scoring 21.8% respectively. Question 13 asks when it is most suitable for a woman to conceive again should she had required chemotherapy following a complete or partial hydatidiform molar pregnancy. In the O&G cluster in this study, if a molar pregnancy should require chemotherapy, the patients are referred to the Gynecological Oncology unit. Subsequently, patients remain on follow up with the Gynecological Oncology unit and any further advice is provided from their team. Therefore, most general clinicians would not have had to manage these patients any further. This could probably explain why most clinicians would have answered this question incorrectly. Question 15 is regarding the recurrence rate of molar pregnancy. The disease is rare with an incidence of 1 in 387 live births in Asian women and a recurrence rate of 1 in 80. Therefore, most clinicians have acknowledged that the recurrence is rare. However, they were unfamiliar with the actual numbers. This questionnaire helped them become reacquainted of this.
As a form of continuing medical education, results were presented to all doctors during a teaching session. All answers were provided and questions were open for discussion. Clinicians were then given the opportunity to discuss the disease and clarify any uncertainties regarding molar pregnancy. They had agreed that the feedback session was useful.
The overall knowledge of O&G doctors in the cluster regarding molar pregnancy can be improved. It would be beneficial to have teaching sessions on GTD at all institutions that have an Obstetrics and Gynecology unit as a refresher course yearly in order to keep up to date with the current guidelines and remind doctors about the disease, its pathology, clinical presentation, management and follow up. We propose a repeat audit following the teaching session to see if there is significant improvement to the knowledge of the professionals following the teaching session. Furthermore, a continual system of education and clinical audit is in place to ensure optimum patient care.
Gestational Trophoblastic Disease is a rare spectrum of conditions, which is diagnosed histologically. To date, surgical evacuation of the uterus is the initial first line management followed by trending of serum beta-hCG levels. Despite having a potential to turn malignant, most of diagnosed GTDs resolve and 98% of patients with a previous GTD will go on to have a normal, healthy pregnancy. As the disease is potentially treatable with a low recurrence rate, it is important that healthcare professionals dealing with the disease keep up to date and are aware of the diagnoses and subsequent management of this disease.
6. Conclusion
Gestational Trophoblastic Disease is a rare spectrum of conditions, which is diagnosed histologically. To date, surgical evacuation of the uterus is the initial first line management followed by trending of serum beta-hCG levels. Despite having a potential to turn malignant, most of diagnosed GTDs resolve and 98% of patients with a previous GTD will go on to have a normal, healthy pregnancy. As the disease is potentially treatable with a low recurrence rate, it is important that healthcare professionals dealing with the disease keep up to date and are aware of the diagnoses and subsequent management of this disease.
Competing Interests
The authors declare that they have no competing interests.