What is known?
- Liver biopsy is a useful way to diagnose biliary atresia.
- Liver biopsy is a invasive way compared to B-ultrasound scanner, MRCP, ERCP and so on.
What is new?
- Liver biopsy can make differential diagnosis to other cholestasis.
- Liver biopsy has many advantages and shortcomings.
1. Introduction
Biliary atresia (BA) is a disease with unknown etiology that affects both the extrahepatic and intrahepatic bile ducts, it is a progressive; obliterate fibro-inflammatory disease in infancy [1]. BA is most common reason of causing pathologic jaundice in infants, accounting for more than 30% neonates have obstructive cholestasis, cirrhosis and end-stage liver disease in first year of life. And it is the most common indication for liver transplantation in infants [2]. Many investigators aim to solve the dilemma of early diagnosis of BA, it is particularly distinguished it from other causes of neonatal cholestasis (NC) without need of cholangiography [3]. So it is very important to make differential diagnosis of BA and other neonatal cholestasis as soon as possible. Liver biopsy is seemed as the second gold standard of diagnosing BA, but it has many demerits. Therefore, the purpose of our study is to evaluate liver biopsy to diagnose BA in infants with cholestasis.
2. Methods
2.1 Literature search
We searched PubMed, EMBASE and the Web of Science databases for articles published up to December 2017, using following terms(BA [Title/Abstract]) AND (liver biopsy [Title/Abstract]), (cholestasis [Title/Abstract]) AND (liver biopsy [Title/Abstract]), (infantile jaundice [Title/Abstract]) AND (liver biopsy [Title/Abstract]) without any language or data limits. Reference lists of the relevant studies were evaluated for any possible missed citation. Cited articles of each relevant study were also reviewed for any other possible relevant study.
2.2 Inclusion criteria
The inclusion criteria for identified articles were as follows:
- Use pre-operative liver biopsy or percutaneous liver biopsy or ultrasonic guided liver biopsy. All measure about liver biopsy was finished before surgery.
- Data including: at least one of the sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy or have definite number of TN (True Negative), FN (False Negative), FP (False Positive), TP (True Positive).
- Articles were published in full texts in English.
- Studies with other sufficient information for analysis.
- The confirmed diagnosis of BA used cholangiography as golden standard
2.3 Exclusion criteria
The exclusion criteria for the identified articles were as follows:
- Letters, reviews, case reports, and conference abstracts, editorials, and expert opinion reviews and abstracts.
- Data deficiency to analysis or false data.
- Studies with overlapping cases and data. If cases of two or more studies overlap each other, give priority to the study with more diagnosis methods evaluated and whose cases are more if diagnosis methods are the same.
- Use intraoperative liver biopsy or intraoperative frozen section to diagnose BA.
2.4 Screening
Retrieved articles were evaluated blindly by two of authors and in case of any disagreement the opinion of a third author was used.
2.5 Data extraction
Data were extracted on study characteristics. Extract the data of the commonest criteria if the study evaluates two or more criteria of a diagnosis method.
2.6 Quality assessment
Using the version 2 of the Quality Assessment of Diagnostic Test Accuracy Studies (QUADAS-2) tool [4], quality of studies included in our study was assessed by two researchers.
2.7 Data analysis
For those studies where the TP, FP, FN, and FN were available, forest plots were generated for the sensitivity and specificity, positive likelihood ratio (LR+), negative likelihood ratio (LR-), diagnostic odds ratio(DOR) with 95% CIs, PPV and NPV using Meta-Disc. Pooled averages of sensitivity, specificity, and accuracy are calculated as the sum of individual data weighed based on sample size. We constructed a summary receiver operator characteristic curve (SROC) andcalculated the area under curve (AUC). Heterogeneity was assessed using the I2 statistic index. When a great heterogeneity was noted, heterogeneity by a “threshold effect” was analyzed using Spearman correlation coefficients (p<0.05 represents threshold effect). We evaluated the effects of age, wound degree and serum bilirubin level on the accuracy of liver biopsy by using chi-square and independent sample t-tests and the binary logistic regression method. We also made subgroup analyses on study design (prospective versus retrospective), cases (<60versus≥60) to discuss the heterogeneity. SPSS software version 11.5 was used for these statistical analyses (SSPS, Chicago, IL). And publication bias is assessed by a Deeks funnel plot (p 0.05 was considered representative of significant statistical publication bias). And publication bias was analyzed by StataMP-64.
3. Result
3.1 Study selection
Data extracted from the 20 included studies had information regarding 1582 patients for further assessment. Figure 1 shows the flow of studies through the review (20 studies were listed in reference [5-24]). Initial search of PubMed, EMBASE and the Web of Science provide 3303 studies. After de-duplication, a total of 2090 studies remained for screening. Following title and abstract screening, 236 studies were included, to read the full text leaving 53 full text articles to be assessed for final eligibility. Of the 53 full text articles assessed a further screening, 20 studies met the appropriate inclusion and exclusion criteria. 33 studies were excluded (5 full text could not be obtained, 1 non-English, 15 insufficient data to construct diagnostic 2-by-2 table, 1 evaluated by two or more researcher without a consensus, 9 with incorrect data, 2 with overlapping patients). All the including articles compare liver biopsy with cholangiography as the golden standard.
3.2 Study characteristics
The characteristics of the studies are available in Table 1. The 20 studies involved 1582 people. 11 studies were prospective, 7 were retrospective and 2 could not be clearly indentified. 10 studies were over 60 cases, 10 were less than 60 cases. Studies were published between 1967 and 2016. Studies most commonly collected from the United States (6/20), studies, followed by Iran (3/20studies) and India (3/20), UK (2/20), China (2/20), S.Korea (1/20), Thailand (1/20), Sebria (1/20), Venezuela (1/20). In 12 studies reporting gender 52.18% (n=1234) of participants were men. About the clear age of diagnose is not mentioned. There are 7 articles [5,7-9,11,14,18] refer to the median age of operating liver biopsy, 4 articles refer to the jaundice index of patients [6,9,17,18], 2 articles about the needle of liver puncture [15,17]. Table 2 summarizes the quality assessment for the 20 full text studies. The overall quality of the included studies assessed by the QUADAS-2 was moderate, and all of the studies were low risk of bias on 5 or more of the 7 items. In 20 articles, the authors make differentiation of BA from other cholangetic jaundice such as infant hepatitis syndrome (IHS). There are main complications mentioned in 20 articles. The main complication is intraperitoneal hemorrhage. The second complication is pain around the puncture position. Others are not mentioned in 20 articles, but we found them in similar articles. In all studies conventional cholangiography was the reference standard.
3.3 Diagnostic values
Data on the diagnostic of liver biopsy were collected from 20 studies with 1582 patients. The Spearman correlation coefficient was -0.405, p value was 0.077, indicating no threshold effect. The diagnostic odds ratio was 170.39 (95% CI, 84.90-341.97), I2 was 49.9%, showing medium heterogeneity among the studies (Figure 2).
The forest plot of the sensitivity and specificity of the diagnostic performance of liver biopsy is shown in Figure 3, 4. The sensitivities and specificities of individual studies varied from 50% to 100% and from 67% to 100%, respectively. The liver biopsy showed pooled sensitivity of 92% (95% CI, 90%–94%), specificity of 95% (95% CI, 93%–96%). LR+ and LR- are shown in Figure 5, 6. LR+ of 12.51 (95% CI, 8.04-19.46) and LR- of 0.09 (95% CI, 0.05-0.16). The summary ROC curves of liver biopsy for the diagnosis of BA are illustrated in Figure 7. The summary ROC curve was symmetric, and the AUC was 0.9761, Q was 0.9300. PPV was 93.84%, NPV was 92.84%. The accuracy was 93.30%.
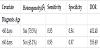
3.3 Subgroup analyses
We compared the different median days of diagnosing BA in two groups, one is less than 60 day [7,9] another is more than 60 days [5,8,11,14,18]. We also compared the degree of jaundice. It can be stand for total bilirubin value and direct bilirubin value. It can be divided into two groups; one is the total bilirubin more than 3.0 mg/ dL,direct bilirubin more than 40% total [6,17]. Another is the total bilirubin more than 2.0 mg/dL,direct bilirubin more than 20% total [9,18]. But one group is contained in another group, so analysis is meaningless. Only 2 articles mentioned with the needle, the size is both 18 mm [15,17], one said the length of puncture is 1 cm; another did not mentioned [17]. So the analysis of the size of needle is meaningless. The results are present in Table 3.
We also performed subgroup analyses and result was present in Table 4. In 20 articles, there are 10 articles using liver biopsy to differential diagnose BA from neonatal hepatitis, data also in Table 4. The heterogeneity evaluated liver biopsy is caused by study design and cases according to the results.
4. Discussion
4.1 Data discussion
Sensitivity can evaluate the ability of finding true patients by liver biopsy. Specificity can react the ability of identifying people who don’t got disease. In this study, sensitivity is 92%, specificity is 95%, that means liver biopsy can make almost true diagnosis to true patient and can identify other disease from BA clearly. LR+ is the index of ratio of true positive to false positive. In this study, LR+ is 12.51, LR- is 0.09, it means that liver biopsy has little possibility to misdiagnose BA and wrong diagnosis. Accuracy can evaluate the ability of diagnosis patient and non-patient. The accuracy is 93.3%, can almost make a clear diagnosis that patient is or is not BA. PPV can predict morbidity if the diagnosis is positive. NPV can predict non-morbidity if the diagnosis is negative. In this study, PPV is 93.84%, NPV is 92.84%, that means if liver biopsy is positive, the patient has 93.84% possibility to have BA, if liver biopsy is negative, the patient has 92.84% possibility to have not BA. ROC curve can response the value of this study, AUC can evaluate the accuracy. In this study, AUC is 0.9761, if AUC 0.9, it has high accuracy, so liver biopsy has high accuracy on diagnosing BA.
4.2 General situation
Percutaneous liver biopsy was finished by Ehrlish in 1883 in Germany. In 1958, Nerghini reported liver biopsy in one second [25]. With the developing of technology, liver biopsy can be divided into the following categories: (1) The percutaneous blind puncture (Menghini method). (2) Ultrasound or CT guided liver biopsy. (3) Liver biopsy guided by laparoscopic. (4) Intraoperative liver biopsy. (5) Liver biopsy via vein [26]. Although liver biopsy has been carried out for a long time, but it is still difficult to popularize with a variety of reasons. In our opinion, liver biopsy has important value in determining the difficult liver disease, differentiate the pathological classification of viral hepatitis, making a direction on treatment and prognosis. It is one of most important research method with small side effects, safe in operation, and it cannot be replace by a lot of non-invasive detection method at present [27]. Although analysis shows high accuracy, specificity and sensitivity, PPV, NPV, AUC. But for infants, this is not only a trauma, but also a psychological pressure. And complications are inevitable.
4.3 Subgroup analysis
Diagnose days: data analyses show that the high accuracy occurred in 60 days (median).
The jaundice was diagnosed as BA occurred in total bilirubin more than 2.0 mg/dL, direct bilirubin more than 20% total.
The needle of puncture has no difference.
4.3 The advantage of liver biopsy
Liver biopsy has high accuracy, specificity and sensitivity, PPV, NPV, AUC. The main use of liver biopsy is to know the degree of liver injury. And we can make a plan to treat. Also liver biopsy can make differentiation of BA from other cholestasis disease. In infant time, BA and infant hepatitis syndrome (IHS) are the common reason of obstructive jaundice. The liver tissue pathology of BA and IHS learn to change have many similarities such as: cholestasis, liver cell damage, hyperplasia of fibrous tissue, inflammatory cells infiltration, giant cells liver cells change, etc. There is still no unified standard of diagnosis and differential diagnosis. And other diseases such as concentrated bile plugs syndrome, biliary dysplasia, liver genetic metabolic disease and so on. BA required surgical treatment as soon as possible, while others are given priority to need medical treatment or liver transplantation [28].
Concentrated bile plugs syndrome, the liver biopsy showed mild change, no obvious fiber group woven and bile duct proliferation.
Biliary dysplasia expressed intrahepatic bile ducts to reduce or disappear, but BA with hyperplasia.
Liver genetic metabolic disease is mainly to metabolism of sugar and fat disorder, such as glycogen storage disease with the common performance is liver disease change: swelling of liver cells and empty pale cytoplasm, nuclear small, thin like plant cell, PAS staining showed lots of positive substance in the liver cells. Some types can be a significant fibrosis, and for the development of cirrhosis of the liver. Bile duct lesions is not obvious, however, there will be no bile duct hyperplasia obviously.
4.4 The shortcomings of liver biopsy
- Liver biopsy is an invasive examination. There are many complications [29-31]. (1) The local biopsy site occurred pain and discomfort. (2) Mid transient hypotension (vascular vague reaction). (3) The right upper quadrant or right shoulder pain. (4) Intraperitoneal hemorrhage. (5) Bleeding of puncture site. It reported that 5.8%-13.5% infants appear transient bacteremia after liver biopsy. Bacteria in biliary obstruction or cholangitis occasionally develop into septicemia or shock. Mortality is about 1/10000-1/12000 [32]. (6) Other rare complications such as: biliary ascites, bile pleurisy, bile peritonitis, hemothorax, subcutaneous emphysema, pneumoperitoneum, scrotal emphysema, abscess under diaphragm.
There have been reported about 1-3% infants need hospitalization for complications, especially use the Tru-cut needle. Froehlich discovered that the incidence of complications lower in surgery doctors who did more than 50 cases per year [33].
- The preoperative preparation and post-operation of liver biopsy are large work. Such as medicine and examination. Regular use vitamin K1 10 mg, vein input, once per day before 3 days to after 2 days of surgery[34].Before liver biopsy, make some tests, platelets, etc [35].
- Repeat sampling. Due to uneven of liver lesions, so need to repeated sample for the same liver and it can cause greater trauma [36].
- The subjectivity of read tissue is strong. The literature said that infants with BA have the following features [37]: (1) The liver portal area occurred perilunate bilious liver fibrosis. (2) Portal area small bile duct hyperplasia, deformity, often associated with progressive developing fibrosis. (3) The formation of capillary bile duct silting bravery and interlobular bile duct bile plugs. (4) The hepatic portal vein and the surrounding inflammatory cells infiltration. (5) With few multinucleated giant liver cells.
- The prognosis is related to the diagnosis time. Some patients need the second liver biopsy. Jolley reported that liver pathology in infants with significant changes occur in the growth of 3-4 weeks, due to cholestasis, the bile salts is not clear in time, mainly distribute around the portal vein. It caused that change. The change is significant in the portal area [38]. As a result, the different days of age influence the accuracy of diagnosis. Alagile considered that combined the liver biopsy with other clinical manifestations can identify about 85% similar cases [39].
4.5 Comparison of advantage and shortcoming of liver biopsy
Although liver biopsy has many shortcomings, but the rate of complications is low, it can be avoided by developing of this technology. And it is necessary to make a pathological diagnostic criteria of BA. There are 4 articles [6-9,12] mentioned pathological diagnostic criteria which were different and this shortcoming should be solved. Although patients should do some pre-examinations, it is necessary for them to have these tests if BA is diagnosed and the surgery will be done in a few days. 10 articles using liver biopsy to differential diagnose BA from neonatal hepatitis, it has high sensitivity, specificity and AUC. So it’s a good way to distinguish BA from hepatitis. Other articles about BA and cholestasis, it’s also a good technology to distinguish BA from other cholestasis.
In a word, liver biopsy has shortcomings, but it is a good way to diagnose BA, and make differential diagnosis from cholestasis. The accuracy is high; we can use liver biopsy before cholangiography and surgery. It is noteworthy that doctors should improve technology, make a clear pathological diagnostic criteria and communicate to patients and relatives.
5. Limitations
Our study has several limitations. First: We do not have enough data to do the subgroup analyses. And in subgroup, the changing factor is not uniqueness, the results of subgroups show the heterogeneities, because the heterogeneities are caused by other aspects such as years, technology. Second, the articles screening has bias, this reason can do a lot of work on heterogeneities. Third, about the days of age, in 20 articles, there are not the actually data about days, only the mid age, it cannot on behalf of the patients’ conditions of disease. As we all know, BA is a disease with progressive and obstructive biliary, the prognosis is related to the diagnosis time. But the progress of liver pathology is different in patients with different days of age.
6. Conclusion
The results of Meta analyze is that liver biopsy is a important method in diagnosing BA. With high accuracy, it can be used in the clinic. But it has many short comings, so we need to avoid the appearance of complications and normalized use this technology.
Competing Interests
Jianghua Zhan is currently receiving a grant (2019D01A12) from the Natural science foundation of xinjiang uygur autonomous region: The mechanism of Notch pathway in hepatic fibrosis of biliary atresia. For the remaining authors, none is declared.