1. Introduction
Parkinson’s disease (PD) is the second most common neurodegenerative disease. It is estimated that PD affects nearly 1% of the population over the age of 60. In the last 25 years, the number of people suffering with PD doubled to more than 6 million, reaching a pandemic dimension [1,2]. The pathophysiology of PD involves the progressive, unremitting loss of dopaminergic neurons in the basal ganglia and the gradual widespread of abnormal alpha-synuclein aggregates, which have been linked to neuronal death. The classic clinical phenomenology of the disease includes bradykinesia, tremor, rigidity, postural instability, and gait dysfunction. Commonly, nonmotor features are also present and could pre-date the classical motor symptoms (e.g. constipation, hyposmia, sleep abnormalities, depression, etc) [3]. Due to disease progression, many other nonmotor symptoms may rise and become a critical cause of disability, including autonomic instability, cognitive impairment, hallucinations and dementia [3]. The prevalence of mild cognitive dysfunction is around 15 to 30% at the time of the diagnosis. Among 20-year PD survivors, an 83% prevalence peak of dementia has been observed [4]. In PD, cognitive abnormalities affect multiple cognitive domains, including executive functions, visual-perceptual functions and motor learning [5-8].
Several drug treatments are available with established symptomatic effectiveness in patients with PD. The therapeutic rationale of these treatments rests on the restoration of adequate levels of brain dopamine (dopamine replacing therapies) or in the mimicry of its post-synaptic effects (dopamine-agonist therapy). To date, there are no disease-modifying drugs to halt the disease progression, and many clinical features become refractory to conventional therapies over time (i.e. DOPA-resistant). Two important and frequent DOPA-resistant sets of symptoms are represented by ‘cognitive decline’ and ‘postural instability and gait dysfunction’ (PIGD) [9,10]. These disorders are intriguingly interrelated and are well-established predictors of decreased quality of life and decreased survival in people with PD [6,11,12-14].
Motor function rehabilitation programs for PIGD typically include dedicated exercise, physiotherapy (PT) and occupational therapy (OT) [15,16]. These treatments usually provide some symptomatic relief, but improvements are generally short-lived and only partially maintained. This limited response appears to be related in part to comorbid cognitive and motor learning impairments [16,17].
Acquiring and consolidating new motor skills are regarded as the hallmarks of motor learning, which are essential for achieving efficient rehabilitation thus, the importance of finding new feasible and safe therapies able to enhance motor learning. Motor learning therapies could then be combined with motor rehabilitation programs to achieve more sustained functional benefits.
Non-invasive brain stimulation (NIBS), such as transcranial magnetic brain stimulation (TMS), is an emerging safe tool for rehabilitation of certain cognitive and psychiatric symptoms in different neuropsychiatric disorders [18,19]. rTMS has facilitated motor memory consolidation in healthy subjects and possibly in patients with brain disease [20-23]. TMS uses magnetic pulses to induce electrical currents in localized brain areas for neuromodulation. Neuromodulation of corticospinal excitability by repetitive TMS (rTMS) induces lasting neurophysiological changes that persist up to 60-90 minutes after stimulation and are the basis of long-term depression- (LTP) and long-term potentiation- (LTP) like mechanisms [24]. These changes are the foundation of therapeutic and rehabilitative paradigms. As such, pairing PIGD rehabilitation training with rTMS could facilitate consolidation of motor models learned during rehabilitation. Hence, PT could be coupled with rTMS in order to maximize the chances of inducing beneficial long-term plastic changes for better functional recovery.
In a previous experiment in our laboratory, we demonstrated that in PD patients, the application of high frequency rTMS over the right posterior parietal cortex (PPC), immediately after a newly acquired visuo-motor adaptation task, restored motor memory consolidation [25]. This area is involved in the integration of proprioceptive, visual and vestibular inputs. As such, the PPC plays an important role in forming and maintaining new internal models used for movement planning. In particular, the binding of multisensory information, as well as the development of memories or models such as those required for moving under new visuo-motor coordinates, is reflected by activity changes occurring over this area [5,26]. Our study showed that while PD patients did not appear to have impairments in memory acquisition during the practice of a learnt motor skill compared to healthy (HC) controls, when re-tested 24-48 hrs later (off-line learning), they performed significantly poorer. Our study further demonstrated that, applying rTMS over PPC immediately after the new hand-skill training session restored the deficient consolidation (24-48 hrs performance) to a level comparable to HC [18].
On this topic, it was recently emphasized how the control of the temporal aspect between motor training and NIBS is crucial in maximizing the chances to achieve effective associative plasticity, as the latter is a time-dependent phenomenon [18,27]. Such a limited time window implies adequate logistics to ensure an effective, standardized and reproducible workflow. For example, the rehabilitation setting where PT is administered, should be equipped with, or be conveniently located in proximity to the TMS device. Furthermore, some population-specific considerations should be taken into account. In patients with PD, the administration of rTMS immediately after a PT session may challenge subject’s endurance and tolerability, particularly in presence of highly prevalent comorbid factors such as anxiety, apathy, fatigue, depression, and chronic pain.
In the present pilot trial study, we aimed to evaluate the feasibility of recruitment, randomization, retention, assessment procedures and implementation of a novel protocol of rehabilitation. The study involves pairing multiple, consecutive sessions of standard PT for PIGD in patients affected by PD, back-to-back with rTMS sessions. The aim is to improve consolidation of PT practice by means of inducing longer-term plastic changes to maximize the clinical benefits.
2. Materials and Methods
2.1 Study design
The study design was a double-blind, randomized, in-parallel, sham-controlled, pilot trial, pairing standard PT with either rTMS or sham rTMS stimulation in patients afflicted with PD with PIGD. Subjects were recruited among patients followed at the Marlene and Paolo Fresco Institute for Parkinson’s and Movement Disorders, New York University School of Medicine, New York, USA. Patients who agreed to participate signed a written informed consent. The study complied with the Declaration of Helsinki and its amendments and was approved by the local Institution's Ethics committee. Patients were randomly allocated to the two experimental arms (PT + rTMS vs PT + sham) on a consecutive basis. No stratification based on age, gender or other characteristics was performed. Randomization codes were generated using https://www.randomizer.org/ and had 4 sets of 4 codes each (for a total of 16 participants). Both subjects and PT providers were blind to the rTMS protocol. Study outcomes included: (1) the feasibility of recruitment and maintenance of subjects, (2) the tolerability, compliance and blinding of rTMS; and (3) the exploration of motor and non-motor outcomes.
2.2 Study population
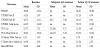
Individuals diagnosed with PD, who were referred to PT for PIGD rehabilitation were telephonically pre-screened to verify study eligibility and interest in participation. The main selection criteria for the study are detailed in Table 1.
2.3 Intervention
PT was administered by an expert physical therapist at Rusk Institute, Department of Rehabilitation Medicine, New York University School of Medicine, New York, USA. Nine PT sessions were administered on a one-to-one basis, One to two times weekly, to specifically address PIGD through dedicated training for gait and balance rehabilitation. Following each PT session, subjects were immediately directed to our NIBS lab to randomly receive either rTMS or sham rTMS. Patient and administrator were blind to intervention. The experimental treatment (rTMS) was designed to follow each PT session within a pre-established time window of 40 minutes.
2.4 TMS protocol
rTMS was delivered over the right posterior parietal cortex (PPC), corresponding to P6 in the 10x20 EEG system of electrode placement. TMS procedures followed our prior methods described by Moisello and colleagues (2015) [25]. In brief, we used a tangentially oriented Magstim 70 mm figure of eight coil with the grip pointing backwards, at 90% resting motor threshold (RMT) intensity. Twenty-five trains, each one consisting of 50 pulses of 5 Hz lasting for 10 seconds (s), were delivered with an inter-train interval of two seconds. The 25 trains were grouped into five blocks of 250 pulses each, for 1250 pulses/session. The five blocks were spaced by a stimulus-free interval of 1 minute. For realistic sham stimulation, we used a figure-of-eight shaped placebo coil generating both noise and vibration similar to the real coil without stimulating the cerebral cortex.
2.5 Assessments
The primary endpoint of the study was to determine feasibility of combining multiple PT sessions for PIGD in patients with PD back to back with NIBS, within a pre-established time window of 40 minutes. As exploratory endpoints, we assessed both motor and non-motor symptoms of PD. The exploratory outcomes are detailed in Table 2. Exploratory outcomes were assessed at baseline, after 5 PT sessions and following the 10th PT session (end of study). Potential adverse events and changes in subjects’ medications were recorded at each encounter. A follow up telephone encounter was performed one month after the last PT session for potential adverse events.
2.6 Exploratory outcomes
Mini Balance Evaluation Systems Test (Mini-BESTest): This is a clinical balance assessment tool that asses dynamic balance through 14 items. It requires 10-15 minutes to be administered [28]. Physical therapists at Rusk use this scale during their normal evaluative sessions. The Mini-BESTest is recommended by MDS-commissioned task for assessing PIGD in PD patients [29].
Five Times Sit to Stand: This is a measure of functional lower limb muscle strength and may be useful in quantifying functional change of transitional movements [30]. Physical therapists use this scale during their normal evaluative sessions. It requires < 5 minutes to be administered.
10 Meter Walk Test: Assesses walking speed in meters per second over a short duration. Time is measured as subject walks a set distance [31]. Physical therapists use this scale during their normal evaluative sessions. We will use this data collected for our outcome purposes. It requires <5 minutes to be administered. It is recommended by MDScommissioned task for assessing PB&G in PD patients [29].
Unified Parkinson’s Disease Rating Scale (UPDRS): The UPDRS is a Parkinson’s rating scale which includes evaluations of mentation, behavior, mood, and activities of daily life as well as a clinician scored evaluation to assess motor symptoms of Parkinson’s disease [32].
Timed Up & Go (TUG): Assesses mobility, balance, walking ability, and fall risk in older adults. Physical therapists use this scale during their normal evaluative sessions [33]. It requires less than 3 minutes to be administered. It is recommended by MDS-commissioned task for assessing PIGD in PD patients [29].
Parkinson’s Disease Questionnaire-39 (PDQ-39): This is self-report questionnaire that assess PD-specific health related quality over the last month. It assessed how often patients experience difficulties across 8 quality of life dimensions and asses impact of PD on specific dimensions of functioning and well-being [34]. It has become the most frequently used disease-specific measure of health status. It takes 10-20 minutes to be administered.
2.7 Data analysis
Statistical analysis was performed using SPSS version 23 (IBM, Armonk, NY). The explore tab from descriptive characteristics was run to test for normality and determine if the variables were parametric or non-parametric. The normality of data was checked by applying the Shapiro-Wilk’s test. The initial planed statistics included within-subjects changes in outcomes using paired T-tests if the data is normally distributed, or Mann-Whitney if the data is non-parametric and between group using the independent T-test or the Wilcoxon signed-rank test for two data time points and repeated measures of ANOVA or Friedman test if there are more than 2 data time points. Based on our preliminary study using similar methods, we estimate the enrollment of 16 patients (8 patients per arm) will be sufficient to determine feasibility and generate preliminary data. After the completion of the 5th patient, the study was stopped due to changes in the Center’s location and logistics couldn’t meet the study goals (distance between the PT and the TMS lab were too far). Limited analysis was performed instead.
3. Results
3.1 General Characteristics
The demographic and general characteristics of our sample are summarized in Table 3. The mean age of the sample was 74 (SD 8.6) years (4 males). The mean disease duration was 9 (SD 4.6) years. The mean Unified Parkinson’s Disease Rating Scale (UPDRS) was 62 (SD 11.3) and motor score (UPDRS-III) was 44.2 (SD 10.5). The Mini-Balance Evaluation Systems Test (Mini-BESTest) score mean was 19.6 (SD 5.4), and the Timed Up & Go (TUG) 13.5 (SD6.3). The Hoehn & Yahr (H&Y) stages at screening were 2 (n=1) and 3 (n=4).
3.2 Feasibility of recruitment and maintenance of subjects
Nine patients were consecutively referred to PIGD-oriented PT from August 2016 to November 2016. Among these, seven prescreened subjects qualified to be invited to participate in the study. One patient refused participation and one patient received PT from another provider. The remaining five patients accepted to participate. One participant withdrew consent from the study after the 5th visit due to loss of interest in participating. All (100%) PT sessions were followed by the experimental TMS/sham stimulation. The average time lapse between PT and TMS/sham delivery during the first session (that included TMS intensity determination) was 23 (SD 13) minutes (min: 10 and max: 40 minutes). At the following sessions, the average time lapse between PT and TMS/sham was 12.7 minutes, SD 5.4 (min: 5 and max: 25 minutes). On December 2016 our movement disorder center moved to another location and recruitment was stopped as per protocol requirements.
3.3 Tolerability, Compliance and Blinding of rTMS
A total of 41 paired sessions were completed in 5 subjects with 100% adherence. Binding was considered adequate all five subjects believed stimulation to be real (three randomized to real and two randomized to sham rTMS). We observed four (4) adverse events. Subject 1 presented neck pain of mild intensity following one rTMS session. The pain subsided within 24 hours, and required no medical attention. Subject 5 experienced an episode of bronchitis deemed unrelated to study. Subject 4 had one fall and one episode of dizziness, both unlikely related to study procedures. There was no severe adverse event.
4. Discussion
In the present study, we aimed to test whether systematic rTMS adjuvancy to PIGD-oriented PT constitutes a feasible paradigm of neurorehabilitation to improve motor memory consolidation and with this, functional outcomes in patients with PD. To date, most of the evidence supporting rTMS adjuvancy for the consolidation of motor learning rests on studies utilizing laboratory-based motor tasks. The “ecological” validity of these paradigms, as well as their generalizability into clinical settings is therefore limited. This is particularly relevant for people suffering from PD, in which PT is administered to improve or restore gait and balance dysfunction with often-limited results.
We purposefully designed our NIBS protocol to avoid any interference with the administration of standard PT. Even so, administering TMS after a PT session can represent an additional burden for patients with PD, who commonly, suffer from comorbid pain, anxiety, apathy, fatigue and depression. The possibility of dropouts needs to be carefully considered. According to our preliminary data, systematic TMS paired with multiple session of standard PT represents a feasible and safe paradigm with excellent compliance as far as the TMS is at or nearby the PT center.
It is crucial to control the temporal aspect between motor training and NIBS to optimize the chances to achieve effective associative plasticity. This has been shown to be a strictly timedependent phenomenon. Hence, the rehabilitation setting where PT is administered should be conveniently located in the proximity of the TMS device. For this study, we took advantage of a consolidated scientific partnership and a conveniently shared location between our NIBS lab and the PT facility. This allowed us to comply a predetermined temporal window of 40 minutes between the end of each PT session and the administration of our NIBS protocol. As a case in the point, the fact that the Parkinson’s clinic was relocated far away from the PT building, determined the early termination of the study.
In patients affected by PD, PIGD are well-established predictors of decreased quality of life and decreased survival. These symptoms typically worsen as the disease progresses, becoming increasingly refractory to conventional pharmacotherapy. Physical therapy rehabilitation often offer some symptomatic relief, but even then, improvements are generally short-lived and only partially maintained. This limited response seems to be related in part to a peculiar impairment of the motor learning process, occurring in patients with PD. Indeed, the acquisition and the retention of new skills are both necessary to achieve optimal levels of motor performance in everyday functioning. In PD, the initial stage of learning, where new skills are acquired or previous skills are modified (i.e. motor memory encoding), appears to be substantially preserved. However, the consolidation and the subsequent retention of motor skills into later stages of learning seems poorly efficient.
Comprehensive experimental evidence suggests the potential for TMS to facilitate the motor learning process in both healthy subjects and patients with brain disease. In a previous experiment in our laboratory, we demonstrated that the application of high frequency rTMS over the right PPC, immediately after a newly acquired visuomotor adaptation task in PD, restored motor memory consolidation to a level comparable to healthy controls [25]. The PPC is traditionally considered as the bridge between vision and movement. Within the PPC network, the integration of different sensory modalities occurs at a unique, highly sophisticated, associative level. Therefore, this area appears as a suitable target of neurostimulation to boost the consolidation of recently acquired complex visuo-motor tasks such as gait and balance training [26]. The underlying proposed mechanisms include the normalization of cortical excitability and the induction of adaptive plasticity through LTP-like phenomena [35]. Pairing PT with rTMS could therefore optimize motor memory consolidation during an intensive rehabilitation training, with the goal of attaining better and more sustained functional benefits.
5. Limitations
Limitations of the study include its small sample size, which currently prevents efficacy analysis. Furthermore, as the time window for associative plasticity has not been clearly stablished, potential efficacy of our protocol in different settings where the TMS device and the PT practice are not in proximity remains to be determined. Our paradigm may contribute to the definition of new models of neurorehabilitation, with broader applications in different clinical settings. Future studies are strongly needed to elucidate the clinical impact of this novel modality of neuro-rehabilitation.
6. Conclusions
In summary, this study has shown that systematic rTMS adjuvancy to standard PT for the rehabilitation of PIGD in patients affected by PD appears to be a feasible, safe, and well-tolerated modality of neurorehabilitation. The efficacy of this paradigm and its generalizability in different clinical settings remain to be determined and the data from our trial would encourage undertaking further studies in larger, randomized, placebo-controlled trials.
7. Disclosures
The authors declare that they have no competing interests and report no disclosures relevant to the manuscript.
Competing Interests
The authors declare that they have no competing interests.
Acknowledgments
The authors would like to thank the Marlene and Paolo Fresco Institute for Parkinson’s and Movement Disorders and the Neurology department at NYU Langone Health for the support.