1. Introduction
Snake bite is one of the causes of stroke that has been reported less frequently. According to WHO, annual rate of snake bites have been estimated 5.4 million worldwide. Proximately 81000-138000 deaths have been reported annually. Most common affected population is among young adults and children in Africa, Asia and Latin America [1]. According to Center of Disease Control (CDC), annual rate of snake bite in the United States is 7,000-8,000 with about 5 deaths. The most common species in the United States reported by Central of Disease Control (CDC) includes rattlesnakes, copperheads, cottonmouths/water moccasins, and coral snakes [2]. In a Sri Lanka case series, the incidence of post-bite ischemic stroke was reported 9 in 500 bites [3].
Different Snake venoms contain different types of enzymes such as phospholipase A2, acetylcholinesterase, hyaluronidase, and metalloproteinases; such enzymes that have either direct neurotoxic or procoagulant or anticoagulation effects [4]. Therefore, These enzymes predisposing for causing either cerebral infarction due to cerebral hypoperfusion (watershed infarct), thrombotic occlusion of large vessels, vasculitis, consumption coagulopathy, or cardiogenic brain embolism; or hemorrhagic stroke [5,6].
Depending on the enzyme content in the venom, the procoagulation versus anticoagulation activities can be prominent. For Instance, viper and colubrid venoms contain metalloproteinases, serine proteases, and C-type lentins with either agonist or antagonist platelet aggregation activity while the venom of elapids contains phospholipase A2 and three-finger proteins, which acts as an neurotoxins in neuromuscular junction [7].
There are few case series reporting snakebite related strokes with detailed information regarding the type of the venom and the type of stroke. Previous work by our group examined the association of snakebite and acute myocardial infarction [8]. In this study, we reviewed different case reports and series of snake envenomation associated with stroke and the outcome.
2. Methods
On October 2018, a systematic search was conducted using PubMed and Google Scholar to review case reports about stroke caused by snake envenomation from January 1995 to October 2018. Studies that listed the keywords “snake, envenomation, stroke, cerebrovascular accidents” were used to identify case reports of stroke associated with snake envenomation. The reference list of each report was checked for additional cases. Data reviewed included demographic data, cardiovascular risk factors, snake species, computed tomography of the head, magnetic resonance of the head, time of presentation, complications, management, and outcome.
3. Results
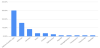
83 cases were identified (Table 1) [9-79]. The patients were in the age group of 5 to 80 years and the mean age was 40 ± 17.5 years, median age was 40 years and 66.3% of the cases were younger than 50 years of age. 68.7% of the cases were reported for males and 31.3% for females. Diabetes Mellites and hypertension were reported only in 2 cases (2.4%). Snake Species are represented in (Figure 1); however, about 30% of the cases did not mention snake species. 30% of the cases reported with Daboia, Russell's viper, species. 83.1% of the cases were bitten in their legs and 16.9% were bitten in hands. All the cases were managed by anti-snake venom, in 27.7% of the cases the symptoms started after receiving anti-snake venom. 19.3% of the cases also treated with antiplatelet and 3.6% were treated with craniotomy. The mean time for the onset of the symptoms is 23.8±10.9 hours after exposure. 77.1% of the cases found to have ischemic stroke, 20.5% with intra-cranial hemorrhage and both infarction and stroke in 2.4%.
Complications were reported in many cases: Altered mental status necessities intubation in 36.1% of the cases, acute kidney injury was reported in 12.2%, pulmonary edema in 3.6%, myocarditis in 1.2% and endocarditis in 1.2%. The outcome of the cases showed full recovery in 26.5% with mean time needed for recovery 88.9 days. Mortality was reported in 16.9% mainly due to complication of stroke with mean time between onset of the symptoms and death is 4.2 days.
4. Discussion
Venomous snakes can cause stroke due to either their neurotoxic or hemotoxic enzymes [4]. However, type of stroke either hemorrhagic or ischemic depends on the venom enzyme-make up in each different snake species.
Ischemic strokes were 77.1% of the cases while ICH were 20.5%. As reported, the most common species were Russell's vipers with higher incidence of ischemic stroke than intracranial hemorrhage (ICH). Whereas, reportedly Bothrops species were the second most common venoms to be reported with significantly more propensity towards ICH than ischemic stroke [3]. Most of the cases exposed to snake bites are young males <50 years old. Mortality rate was higher among Russell's vipers; however, Russell's vipers were the most commonly reported bite. There was single report of bite by Horned viper and Pseudonaja textilis with ICH; Cerastes and Deinagkistrodon envenomation were associated with large infarcts [29,74,32,66].
The venom of Bothrops species contains metalloproteinases, type of hemotoxin that can cause hemolysis, thrombocytopenia, disseminated intravascular coagulation [76,77]. Among Borthrops, ICH was frequently reported in jararacussu, atrox, marajoensis species and infarcts was reported for lanceolatu species. Most of the patient who had bites were young and no comorbidity or risk factor for either hemorrhagic or ischemic stroke except 2% who had history of diabetesmellitus or hypertension.
Mortality was more common among those who either arrived in coma or required intubation due to AMS during the course of hospitalization. Death happened within the first 4.2 days after the exposure. Risk of mortality was amplified by ICH, bilateral extensive cerebral, cerebellar infarction, mass effect, or post circulation occlusion.
However, all the cases received anti-venom once they sought medical care after exposure; while mean time for the onset of symptoms was 23.8 h after envenomation. In 27.7% of the cases symptoms started even after receiving antivenom which indicates the potency of the venom in causing stroke and the importance of early administration of anti-venom serum with consideration of other adjutant therapies. There are some animal studies indicating the critical and time sensitive usage of metalloproteinase inhibitors and antivenom would be the best approach to reduce hemorrhagic stroke after Bothrops species envenoming [78]. Studies have shown that single individual fractions of different venoms have failed to be lethal to mice in some studies even after 48 h, whereas a corresponding concentration of whole crude venom have been sufficiently lethal within 10 min. Synergistic action of venom component is important for designing more effective antivenoms [79]. In figure 2, we summarized the postulated mechanisms for cerebrovascular accidents following a snake envenomation.
Limited access to antivenom and also lack of awareness for seeking medical management shortly after snakebite to reduce the chance of cerebrovascular events and the other complications mainly in developing countries is an alarming medical emergency to be addressed. Therefore, WHO considered snake envenomation as category A neglected tropical diseases to maximize the efforts facing its complication [80].
5. Conclusion
Stroke is a rare but rather serious complication of snake envenomation that is associated with high mortality rate. Further research is needed to elucidate the mechanisms of stroke in the context of snakebites thus paving the way for the development of specific therapeutic interventions. However, early administration of anti-venom serum with consideration of other adjutant therapies is crucial in snakebites in order to reduce the associated complications including strokes.
Competing Interests
The authors declare that they have no competing interests.
Acknowledgments
This work is supported, in part, by the efforts of Dr. Moro O. Salifu M.D., M.P.H., M.B.A., M.A.C.P., Professor and Chairman of Medicine through NIH Grant number S21MD012474.