1. Introduction
Cerebrovascular accident (CVA) is a known cause of significant morbidity and mortality in the United States [1]. Ischemic stroke accounts for majority of strokes [2]. Cardio-embolic strokes account for nearly 14-30% of ischemic stroke and are often associated with recurrence and high mortality [3]. Lambl’s excrescences (LE) (Figure 1) though often reported in transesophageal echocardiography of patients who suffered stroke it is not clear if they are bystanders or the cardio-embolic source of such stoke [4]. Multiple isolated case reports of stroke where LE has been attributed as the cause of stroke have been reported. Guidelines regarding management of LE in the setting of stroke are largely lacking. We here undertake the first scoping study of cases of stroke associated with LE reported to understand the clinical profile of these patients, imaging studies and management that were employed, recurrent rates and mortality.
2. Methods
On 28th January 2018, a systematic search was conducted using Pubmed, Google Scholar, CINAHL, Cochrane CENTRAL and Web of Science databases (Figure 2). Studies listing the keywords “lambl’s excrescences, stroke, cerebrovascular accidents” were used to identify cases of stroke associated with LE. No specific duration was chosen during search.The reference list of each report was also checked for additional cases. All cases were reviewed in detail. Data reviewed included demographic data, CV risk factors, electrocardiography (ECG) findings, transthoracic echocardiography (TTE), transesophageal echocardiography (TEE), computed tomography of the head, recurrence of stroke, management of LE and death (Figure 3).
3. Results
A total of 27 cases were identified (Table 1) [5-27]. The patients were in the age group of 25 to 78 years and the mean age was 51 ± 14.2 years, median age was 53 years and 44% of the cases were younger than 50 years of age and 55.5% of cases were younger than 55 years. 56% of the cases were reported in males and 44% in females. Prevalence of cerebrovascular risk factors and co-morbidities in the population was as follows: hypertension 29.63%, diabetes 18.52%, history of stroke 14.81%, smoking 14.81%, alcohol abuse 11.11%, chronic obstructive pulmonary disease (COPD) 7.41%, history of transient ischemic attack 3.70%, history of coronary artery disease (CAD) 3.70%, obstructive sleep apnea 3.70%, deep vein thrombosis 3.70% and cocaine use 3.70%. Majority of patients presented with dysarthria/aphasia (51.85%) and hemiparesis (37.04%); other presenting complaints have been tabulated (Table 2).
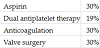
TTE was reported in 14 cases, of which 6 cases (42.85%) reported LE (2 on aortic valve, 4 on mitral valve), 1 case (7.14 %)raised the suspicion for LE and no LE was detected on TTE in 7 cases (50%) all of whom were noted to have LE on TEE. TEE was reported in 22 cases of whom LE was noted on aortic valve in 82%, on mitral valve in 14% and pulmonary valve in 4%. A total of 26 cases reported the valve of LE origin which was aortic valve 73%, mitral valve 23% and pulmonary valve 4%. 25 cases reported the number of LE of which 64% of cases reported a single LE and remaining 36% of cases reported more than one LE as visualized in TEE or TTE (Table 3). Middle cerebral artery (MCA) territory was most commonly affected (Table 1). 30% reported recurrence. Management of stroke secondary to LE (Table 1 and Table 4). No mortality was reported.
4. Discussion
Cerebrovascular accidents (CVA) also known as stroke is a significant cause of morbidity and mortality in the United States and is the fifth leading cause of death [1]. About 800,000 cases of stroke are reported annually of which about 600 are new strokes [1]. About 87% of CVA are ischemic in nature [28-31]. When compared to firstmultiple isolated cases of LE association with stroke and recurrent stroke have been reported. Also cases of thromboembolism into coronary artery [32], renal artery [33] and popliteal artery [34] have been reported. LE usually develop at the site of valvular closure where endothelial damage happens secondary to valve wear and tear forces [35]. LE on gross examination are filiform projections with narrow base, that are 1X 4-10 mm in size and often branches are noted. LE most commonly noted on aortic and mitral valves [18,35]. Potion of LE may detach to cause embolisation or an atheroma originating on LE may embolize to cause stroke [18,36]. Transesophageal echocardiogram is more specific in detection of LE as compared to transesophageal echocardiogram [18,36,37]. Differential diagnosis for LE include i) papillary elastomers which has short broad stalk, jelly like homogeneous masses that appear in endocardium areas of valves where there is less wear and tear, ii) infective endocarditis, iii) artifact, iv) thrombus, v) redundant leaflet of a valve, and vi) intimal flap of aortic dissection [11]. Computed tomography is helpful in differentiating LE from its differentials [18,36]. LE was noted to be present in 22% of patients on whom transesophageal echocardiogram was performed following stroke [4]. Despite the high prevalence of LE in patients who had stroke it is unclear if LE is the etiology or an incidental finding in these patients [38].
Recent trends suggest age at relatively younger age and in 2005 age at stroke was 69.2 years with 12.9% of patients under age 55 years [39]. The mean age at stroke in our study was 51 ± 14.2 years and about 55% of patients were younger than 55 years of age. Compared to statistics from 2005 [17] our patients were relatively younger likely due to cardio-embolic source of stroke. MCA territory was most commonly affected territory. TTE was not effective in detecting LE and missed LE in 50% of the cases and LE in these. Thus it can be concluded that TEE is superior to TTE in diagnosing LE. LE originated from aortic valve most commonly followed by mitral and pulmonary valve. Recurrent stroke was reported in 30% of cases. Though no mortality was not reported at the time of publication of these cases it is not clear if stroke secondary to LE led to mortality in any of the patients. Management strategy employed varied widely likely based on individual experience as large.
5. Conclusion
LE is a rare cause of cardioembolic stroke. When noted on imaging studies it is difficult to conclude if LE is the cause of stroke or just an innocent bystander. As noted in our study LE is associated with high risk of stroke recurrence. TEE is superior to TTE in detection of LE. The study design likely attributes to no mortality not noted in our study and as noted with other causes of cardioembolic stroke, LE may be expected to carry a high mortality rate on follow up. We recommend dual antiplatelet after the first episode of CVA related to LE and an antiplatelet in combination with anticoagulation after the second CVA attributed to LE. Also it is reasonable to offer valve replacement after second CVA related to LE as the recurrence rate of CVA is high. Due to rarity in LE reporting and its management a shared decision making has to be made depending on the clinical status of the patient.
Competing Interests
The authors have no competing interests with the work presented in this manuscript.