1. Introduction
Approximately 17 million people suffer a stroke every year worldwide [1]. Stroke is one of the disorders in which motor dysfunction after onset is likely to remain [2]. It is known that complete restoration of motor function of paralyzed limbs after stroke is approximately 20% in the upper extremities, whereas it is around 60% in the lower extremities [3]. As upper extremity dysfunction after a stroke greatly decreases the quality of life (QOL) [4], it is an important issue to improve upper extremity function after stroke.
Mental practice with motor imagery is one of the effective treatments for improving upper extremity function after stroke [5]. Motor imagery is commonly defined as the mental simulation of one’s own performance without any associated overt movement [6]. Motor imagery has been shown to induce neurophysiological activation of the brain areas related to the planning and execution of voluntary movement in a manner that resembles how the action is carried out in reality [7]. Moreover, previous studies reported that motor imagery is effective for improving motor skill acquisition [8] and increasing muscle strength [9], motor imagery is widely applied in stroke rehabilitation [10-14].
However, there are disadvantages in that the participant is not able to perceive the quality of the motor imagery performed during motor imagery [15], and that there are individual differences in the effect obtained by motor imagery [16]. In order to avoid these disadvantages, a technique to provide the brain activity during motor imagery to the participant, called neurofeedback, was developed. It was reported that neurofeedback training is effective for improving upper extremity function after a stroke [17-19]. Prasad et al. revealed that visual neurofeedback training with motor imagery using electroencephalography (EEG) improved upper extremity function in chronic stroke patients [17]. Moreover, Mihara et al. reported that visual neurofeedback training with motor imagery using functional near-infrared spectroscopy (fNIRS) improved upper extremity function in chronic stroke patients [18]. Furthermore, Zich et al. disclosed that home-based visual neurofeedback training with motor imagery using EEG improved upper extremity function and increased white matter integrity as revealed by diffusion tensor imaging in chronic stroke patients [19]. These studies indicate that visual neurofeedback training with motor imagery is effective for improving upper extremity function after stroke.
On the other hand, it has been reported that motor learning with feedback is sensory modality dependent [20]. Ronsse et al. revealed that motor skill acquisition with feedback was faster in the visual feedback group than in the auditory feedback group, whereas reproduction of acquired motor skill without feedback was higher in the auditory feedback group than in the visual feedback group [20]. This study suggested that auditory neurofeedback training with motor imagery is effective for improving upper extremity function after stroke, but this has not yet been fully clarified. Therefore, this study aimed to investigate the effect of auditory neurofeedback training on upper extremity function and motor imagery ability in a stroke patient.
2. Materials and Method
2.1 Case description
A 48-year old Japanese man with right hemiplegia after hemorrhage in the left putamen participated in this study. In the 3 months after the onset of stroke, the participant received standard rehabilitation (physical and occupational therapy). The standard rehabilitation included the essential treatment required for improving body function and structure, activity, and participation in the International Classification of Functioning, Disability and Health (ICF) model developed by the World Health Organization (WHO). The subscale scores of a Fugl-Meyer Assessment (FMA) of the upper extremity were as follows: the shoulder/elbow/forearm score was 14, the wrist score was 0, and the hand score was 4. The Mini-Mental State Examination score was 26, and higher brain dysfunction or evidence of a psychiatric disorder was not observed in the participant.
The study was conducted according to the principles of the Declaration of Helsinki and was approved by the local Institutional Ethics Committee (Kyoto Kizugawa Hospital). The subject gave their informed written consent and was free to withdraw from the study at any time.
2.2 Study protocol
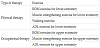
This study consisted of baseline and intervention periods (4 weeks each). During the baseline period, the participant performed standard rehabilitation, which included 60 min of physical therapy and 60 min of occupational therapy, conducted once daily for a total of 4 weeks (Table 1). During the intervention period, the participant performed auditory neurofeedback training with motor imagery in addition to standard rehabilitation. The auditory neurofeedback training was conducted once a day, three times a week, for a total of 4 weeks.
The motor imagery task of elbow and finger movements [18] was performed in the auditory neurofeedback training. Moreover, real-time auditory feedback of the EEG activity measured during the motor imagery task was provided to the participant. First, the participant was seated comfortably in a chair with back and armrests. The participant performed the kinesthetic motor imagery of selfpaced flexion and extension movements of the elbow joint on the paralyzed side. Next, the participant performed the kinesthetic motor imagery of finger movement on the paralyzed side. The imagined finger movement was self-paced and sequential folding of the fingers from the thumb to the little finger, and then unfolding them from the little finger to the thumb. The motor imagery tasks were 30 s each and were performed five consecutive times. EEG activity was measured when the participant performed the motor imagery tasks using an electroencephalograph (NeXus-10 MARKII, Mind Media, Netherlands) (Figure 1). The EEG was recorded using two channels (C3, C4) based on the international 10-20 system, at a sampling rate of 256 Hz. Reference electrodes were attached to both the mastoid processes. Frequency analysis using BioTrace software (NeXus-10 MARKII, Mind Media, Netherlands) was performed on the recorded EEG data, and real-time auditory feedback, which includes the degree of event-related desynchronization of mu rhythm (8-13Hz) related to the motor imagery [21], was provided to the participant. Specifically, when mu-event relation desynchronization (ERD) appeared during the motor imagery task, it meant that the motor imagery performed by the participant was good and an auditory stimulation was provided to the participant at that time. On the other hand, when mu-ERD did not appear, an auditory stimulation was not provided to the participant. For the auditory stimulation, a pleasant sound specified by the International Affective Digitized Sounds [22] was used. Using auditory neurofeedback, the participant was able to properly perceive the quality of the motor imagery performed.
Upper extremity function and motor imagery ability were assessed before (Pre1) and after (Pre 2) the baseline period, and then after the intervention period (Post). The FMA and Motor Activity Log (MAL) were measured to evaluate the upper extremity function. The Hand Laterality Judgement Task (HLJT) and Kinesthetic and Visual Imagery Questionnaire-10 (KVIQ-10) were measured to evaluate the motor imagery ability (Figure 2). FMA and HLJT were used as an objective index, and MAL and KVIQ-10 were used as a subjective index.
2.3 Measures
FMA is the most common assessment of the upper extremity function of stroke patients [23], which was developed by Fugl-Meyer et al. [24]. In this study, shoulder/elbow/forearm, wrist, and hand subscales of FMS were used. Each item is scored on a 3-point ordinal scale of 0 to 2. The shoulder/elbow/forearm score ranges from 0 to 36, the wrist score ranges from 0 to 10, and the hand score ranges from 0 to 14, with higher scores indicating greater upper extremity function.
MAL is a questionnaire used to assess upper extremity function in activities of daily living (ADL) in stroke patients, developed by Taub et al. [25], which was then was compiled into 14 items by van der Lee JH et al. [26]. The reliability and validity of MAL is high [27], thus, like FMA, it is used worldwide [23]. The MAL consists of 14 items, which assess the amount of use (AOU) and quality of movement (QOM) of the paretic upper extremity in ADL. Each item is scored on a 6-point ordinal scale from 0 to 5, and the average score was calculated by dividing the total score by the number of items. The AOU and QOM scores each range from 0 to 5, with higher scores indicating greater upper extremity function.
The HLJT is a mental rotation task used to assess the motor imagery ability [28]. The HLJT is widely used as a tool to evaluate the motor imagery ability of stroke patients [29-32]. In this study, Recognise (Neuro Orthopaedic Institute, Australia) [31] was used to assess the motor imagery ability. In the HLJT, pictures of the back and the palm of the hand are presented in different rotated angles on the screen. The participant was asked to respond as quickly as possible by pressing the left button when a left hand appeared and the right button when a right hand appeared. The unaffected hand was used to press the button. In the HLJT, 50 pictures were presented; the accuracy (% correct answer) and reaction time (s) were calculated.
The KVIQ is a questionnaire used to assess the motor imagery ability, which was developed by Malouin et al. [33]. The reliability and validity of the KVIQ was revealed by a previous study [33], and it is clinically applied as a tool to evaluate the motor imagery ability of stroke patients [34-37]. There are multiple versions of the KVIQ, including the KVIQ-20, which consists of 20 items (ten items each for visual and kinesthetic subscales), and the short version, KVIQ- 10, which is a subset of the KVIQ-20, consisting of ten items (five items each for visual and kinesthetic subscales). The KVIQ-10 [38] was used in this study. Each item is scored on a 5-point ordinal scale from 1 to 5. The KVIQ-10 total score ranges from 10 to 50 (visual and kinesthetic subscale scores each range from 5 to 25), with higher scores indicating greater motor imagery ability.
3. Results
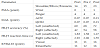
The shoulder/elbow/forearm subscale of the FMA improved in the Post compared with the Pre1 and Pre 2, whereas the wrist and hand subscales did not improve. The AOU and QOM subscales of the MAL, accuracy and reaction time of the HLJT, and visual and kinesthetic subscales of the KVIQ-10 improved in the Post compared with the Pre1 and Pre 2 (Table 2).There were no adverse effects of the intervention.
4. Discussion
The results of this study showed that the shoulder/elbow/forearm subscale of the FMA, the AOU and QOM subscales of the MAL, accuracy and reaction time of the HLJT, and visual and kinesthetic subscales of the KVIQ-10 improved after the intervention period compared to before and after the baseline period. This study suggests that auditory neurofeedback training contributes to improving upper extremity function and motor imagery ability in stroke patients.
In this study, the shoulder/elbow/forearm subscale of the FMA, which is an objective index of upper extremity function, improved after the intervention period, whereas the wrist and hand subscales of the FMA did not improve after the intervention period. Beebe et al. reported that the proximal and distal functions of the upper extremity in stroke patients show a similar recovery process [39]. On the other hand, it is reported that the degree of paralysis of the proximal and distal functions of the upper extremity after a stroke varies depending on the site of the lesion. Hatakenaka et al. revealed that stroke patients with a distal dominant paresis of the upper extremity had damage in the posterior putamen, posterior limb of the internal capsule, and posterior half of the corona radiata, whereas stroke patients with a proximal dominant paresis of the upper extremity had damage in the middle part of the corona radiata, usually sparing the posterior half of the posterior limb of the internal capsule [40]. The lesion site of the participant in this study was the putamen. Therefore, it was suggested that the wrist and hand subscales of the FMA after the intervention period did not show improvement, because the distal dominant paresis of the upper extremity appeared to be due to the damaged putamen in this study.
Moreover, the AOU and QOM subscales of the MAL, which is a subjective index of upper extremity function, improved after the intervention period; however, the improvement value was small. A previous study reported that there was a significant correlation between the AOU and QOM of the MAL and FMA [41]. In this study, the shoulder/elbow/forearm subscale of the FMA showed an improvement after the intervention period. Therefore, it is suggested that the change in the shoulder/elbow/forearm subscale of the FMA improved the AOU and QOM subscales of the MAL. Moreover, the MAL evaluates the skill of the upper extremity function in ADL, centering on finger function [25,26]. In this study, it is suggested that the skill of the upper extremity function did not change because the wrist and hand subscales of the FMA after the intervention period did not show an improvement. Therefore, the change in the AOU and QOM subscales of the MAL, which reflect the skill of the upper extremity function, was suggested to be small in this study.
In this study, the accuracy and reaction time of the HLJT, which is an objective index of motor imagery ability, improved in the unaffected and affected sides after the intervention period compared with before and after the baseline period. Moreover, the accuracy and reaction time of the HLJT improved in the unaffected and affected sides after the baseline period compared with before the baseline period. Boonstra et al. investigated whether there is a practice effect on the HLJT in healthy individuals and revealed that a practice effect does occur during repeated measurements of the HLJT, which was performed twice with a 3-week interval [39]. Therefore, the practice effect during the repeated measurements is suggested to be involved in improving the accuracy and reaction time of the HLJT in this study.
The visual and kinesthetic subscales of the KVIQ-10, which is a subjective index, showed improvement after the intervention period. A previous study revealed that motor imagery training improves KVIQ in stroke patients and contributes to motor recovery after stroke [42]. From this, it was suggested that auditory neurofeedback training with motor imagery improved the KVIQ, which contributed to improvement of upper extremity function in this study.
There were a few limitations to this study. First, since this study is a single case study, it is not certain whether similar effects can be obtained in other stroke patients. A further study is needed with an increased number of participants to verify the intervention effect of auditory neurofeedback training. Second, this study consisted of baseline and intervention phases; therefore, the residual effect of the former intervention may confound the latter intervention. The effect of the auditory neurofeedback training with motor imagery should be assessed in a future randomized controlled trial. Third, another evaluation method to assess the motor imagery ability, such as the mental chronometry, was not used in this study. Hence, some assessments to evaluate the motor imagery ability need to investigate the effect of the auditory neurofeedback training in a further study. Fourth, psychological aspects such as anxiety, depression, catastrophic thoughts, and the levels of self-efficacy were not assessed in this study. Therefore, a further study should investigate these psychological aspects.
5. Conclusions
This study investigated the effect of auditory neurofeedback training on upper extremity function and motor imagery ability in a stroke patient. The results showed that the shoulder/elbow/forearm subscale of the FMA, the AOU and QOM subscales of the MAL, accuracy and reaction time of the HLJT, and visual and kinesthetic subscales of the KVIQ-10 improved after the intervention period compared to before and after the baseline period. This study suggests that auditory neurofeedback training contributes to improving upper extremity function and motor imagery ability in stroke patients.
Competing Interests
The authors have no competing interests with the work presented in this manuscript.
Author Contributions
HN, TK and SM conceived and designed the experiments. HN, TK, TN, TF and YI performed the experiments. HN and TK analyzed the data. HN, TK and SM wrote the paper.
Acknowledgments
We would like to thank all volunteers who participated in this study.