1. Introduction
Cancer breakthrough pain is described as the “transient enhancement of pain that occurs spontaneously or in association with an expected or unexpected trigger, despite adequate relief of persistent pain” [1,2]. The hallmark of cancer breakthrough pain is that it peaks in a short time (approximately 3 min) and subsides in around 30 min. However, the pain intensitycan reach 70 mm or higher on the visual analog scale, and its expression is often unpredictable [3]. That is, there is a clear difference between the exacerbation of persistent pain with insufficient relief and cancer breakthrough pain [1]. Therefore, healthcare practitioners must understand both pain profiles and link them to the appropriate pain relief. However, in cases in clinical practice when the patient may be complaining of either an exacerbation of persistent pain or cancer breakthrough pain, a short-acting opioid (SAO) formulation or a rapid-onset opioid (ROO) formulation may be administered without adequate pain assessment. The authors have noted several cases in which patients were unable to achieve satisfactory pain relief and adverse reactions occurred. Previously, SAOs have been used for cancer breakthrough pain. However, their effects take approximately 30 min to appear and 1 h to reach the maximum effect and the effect lasts for several hours. Therefore, an analgesic effect cannot be obtained and adverse reactions such as nausea, vomiting, and somnolence cannot be sufficiently controlled when used for cancer breakthrough pain. Conversely, ROOs have a rapid-onset of action (within 10 min) and produce an analgesic effect at the peak time of cancer breakthrough pain; moreover, the effect disappears within 1 h of pain relief [4]. According to a previous report [3], ROOs are useful in treating breakthrough pain because they are consistent with the characteristics of cancer breakthrough pain in cancer patients. However, ROO formulations can only be used a limited number of times per day, the starting dose does not depend on the amount of opioids administered at a fixed time, and the starting dose must be low. Furthermore, the aggravation of persistent pain and cancer breakthrough pain must be assessed, and it is possible that the characteristics of ROO formulations and the different administration methods between SAO and ROO formulations are not fully understood in the medical field.
In this study, we conducted a questionnaire survey on cancer breakthrough pain and awareness of ROO formulations among physicians, nurses, and pharmacists with experience in palliative care to examine whether awareness of the characteristics of ROO formulations and the differences between SAO and ROO formulations are sufficiently widespread in medical practice.
2. Materials and Methods
2.1 Facilities and questionnaire subjects
Thirteen facilities affiliated with the Kanagawa Prefectural Hospital Pharmacists Association that used ROO drugs and received consent from their medical, nursing, and pharmaceutical departments to complete the questionnaire survey were selected for analysis. The subjects of the questionnaire were physicians, nurses, and pharmacists with experience in palliative care who worked at those facilities. Questionnaires were sent by mail, and an anonymous selection method was used. The survey period lasted from December 1, 2017, to December 31, 2017.
2.2 Questionnaire form
The questionnaire is shown in Figure 1 (supplementary file). It was prepared based on an agreement between pharmacists familiar with palliative care and by referring to a previous study [4] that evaluated the efficacy and safety of ROO formulations for proper use. The questionnaire assessed an overview of cancer breakthrough pain, awareness of the proper use of ROO formulations, and evaluation of differences between SAO and ROO formulations. The questionnaire was not intended to evaluate the respondents themselves, and it explained in writing that the participants were free to participate and could stop at any time during the course of the study.
2.3 Survey items
The respondents’ job type, experience in palliative care, use of ROO formulations, and experience in instruction and care were investigated. Survey items concerning cancer breakthrough pain included (1) definition of cancer breakthrough pain, (2) frequency of cancer breakthrough pain episodes per day, (3) type of cancer breakthrough pain (predictable and spontaneous), and (4) duration of cancer breakthrough pain; survey items regarding the dosage and administration of ROOs included (5) starting dose, (6) starting dose does not depend on the daily dose of the opioid analgesic being administered on time, (7) how to adjust the dosage, (8) upper limit of single dose, and (9) restriction of the number of doses; items addressing pharmacokinetics included (10) time of onset of effect and (11) duration of effect; items assessing medication instructions included (12) drug intake method (E-fen® buccal tablets) and drug intake method (Abstral® sublingual tablets); items addressing adverse effects included (13) somnolence, (14) nausea/vomiting, (15) constipation, and (16) side effects that are more likely to occur due to stomatitis or oral bleeding; and items assessing drug price included (17) approximate cost.
2.4 Measurement scale
Four levels (have no idea, do not know much about, well, I know, and know enough) were used to evaluate the items related to cancer breakthrough pain and ROO formulations in questionnaire Q4. For convenience, the levels were converted to scores of 1-4 points. In this study, four even-numbered scales were used instead of odd-numbered scales. This is because it is possible to grasp either trend without setting the center based on the previously reported survey method [5]. For Q5, morphine hydrochloride for internal use and oxycodone hydrochloride hydrate powder comprised the SAO formulation, and knowledge of the differences (use of different drugs for cancer breakthrough pain and exacerbation of persistent pain, dosage, and administration, pharmacokinetics, dosing methods, etc.) from ROO formulations was evaluated on a scale of 0 ~ 10.
2.5 Data compilation and analysis
The cancer breakthrough pain in Q4 and the degree of awareness of ROO formulations were expressed as the number of people (percentage of total) by occupation. Differences between occupations for each item were measured with the χ2 test and the Bonferroni multiple comparison test. Awareness of differences between the SAO and ROO formulations in Q5 was expressed as the mean ± standard deviation. To clarify the factors related to the differences between the two formulations, a multiple regression analysis was conducted using the stepwise variable increase and decrease method, with the objective variable as the knowledge of both of Q.5 and the explanatory variables as the following fields: dosage and administration, instructions on the use of drugs, adverse effects, drug price, pharmacokinetics of ROO formulations (questions 5 to 17), and occupation. The significance level for each test was p < 0.05, and JMP Pro 13 ® (SAS Institute Inc.) was used for statistical analysis.
2.6 Ethical regulation
This study was performed with the approval of the Yokosuka Kyousai Hospital Ethics Committee. This study was conducted in compliance with the Declaration of Helsinki, with due attention paid to the ethical guidelines for clinical research.
3. Results
3.1 Response status
The questionnaire response rate was 72.2% (13/18 facilities), and valid responses were obtained from 25 doctors, 76 nurses, and 77 pharmacists. Eight (7.8%) nurses had worked for less than 5 years, 27 (26.4%) for between 5 and 10 years, and 67 (65.8%) for more than 10 years. Twelve (15.6%) pharmacists had worked for less than 5 years, 22 (28.6%) for between 5 and 10 years, and 43 (55.8%) for more than 10 years.
3.2 Current status of palliative care
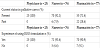
Twenty-five physicians (100%), 70 nurses (92.1%), and 55 pharmacists (71.4%) reported being currently engaged in palliative care. Conversely, 0 physicians (0%), 6 nurses (7.9%), and 22 pharmacists (28.6%) reported being engaged in palliative care in the past (Table 1).
3.3 Experience with use of ROO formulations
Twenty-five physicians (100%), 71 nurses (93.4%), and 70 pharmacists (90.9%) reported previous experience using ROO formulations. Conversely, 0 physicians (0%), 5 nurses (6.6%), and 7 pharmacists (9.1%) reported no previous experience (Table 1).
3.4 Awareness of ROO formulations among physicians, nurses, and pharmacists
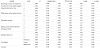
Knowledge of ROO formulations among doctors, nurses, and pharmacists is shown in Table 2. There was a significant difference in knowledge of the definition of cancer breakthrough pain and the frequency of cancer breakthrough pain episodes per day between occupations. Similarly, there were significant differences between occupations for knowledge regarding the following items: starting dose, starting dose does not depend on the daily dose of opioid analgesics being given on time, and constipation.
3.5 Awareness of differences between SAO and ROO formulations among physicians, nurses, and pharmacists
Knowledge of the differences in the SAO and ROO formulations between doctors, nurses, and pharmacists is shown in Table 3. Knowledge of the differences between the two formulations received a score of 4.8 ± 2.5 among all occupations, with significant differences between physicians and nurses and between pharmacists and nurses.
3.6 Multiple regression analysis of differences between SAO and ROO formulations
Factors related to the differences between the SAO and ROO formulations were examined using a multiple regression analysis; the results are shown in Table 4. The following factors were independently and significantly associated with the differences between the formulations: starting dose does not depend on the daily dose of opioid analgesics being given on time, restriction of the number of doses in ROO formulations, duration of effect, drug intake method (Abstral® sublingual tablets), drug price, and occupation.
4. Discussion
This study demonstrated that the awareness of the differences between the SAO and ROO formulations scored as low as 4.8 on a scale from 0 to 10. This finding indicates that less than 50% of professionals with experience in palliative care recognize the use of both formulations, suggesting that the use of both may not be widely accepted in clinical practice. Additionally, the following six factors were specific factors for the insufficient recognition of the ROO formulation and the differences between formulations: starting dose does not depend on the daily dose of opioid analgesics being given on time, restriction of the number of doses in the ROO formulation, duration of effect, drug intake method (Abstral® sublingual tablets), drug price, and occupations.
Confusion with the SAO formulation is considered why the following factors were associated with differences between the drug formulations: starting dose does not depend on the daily dose of opioid analgesics being given on time, restriction of the number of doses in the ROO formulation, and duration of effect. For the SAO formulation, 1/6 or 1/8 to 1/4 of the daily dose of opioid analgesics during regular administration is approved in the package insert as a single dose of morphine hydrochloride oral solution or oxycodone hydrochloride hydrate powder. Conversely, the package insert specifies that the ROO formulation should be started at the lowest dose regardless of the daily dose of opioid analgesics given during regular administration. Additionally, for the ROO formulation, residual pain should be confirmed 30 min after administering the minimum dose. Additional doses can be given if pain persists. Furthermore, the frequency of administration is also limited. The use of the ROO formulation is more complicated than that of the SAO formulation because the titration methods for both drugs differ. Furthermore, the duration of effect differs between the SAO and ROO formulations. SAO formulation effects take approximately 30 min to appear and 1 h to reach the maximum effect, and their effects last for several hours. Conversely, ROO formulations have a rapid-onset of action within 10 min, and the effect disappears within 1 h, which is considered the end of cancer breakthrough pain [6]. Therefore, caution should be exercised because adequate pain relief cannot be achieved without a thorough understanding of the pharmacokinetic characteristics of both drugs.
Awareness of drug price was lowest among all occupations. The ROO preparation is very expensive. Therefore, increased efforts should be made to understand the awareness of the economic burden these drugs place on patients.
In this study, there were significant differences among occupations regarding knowledge of the definition of cancer breakthrough pain and the frequency of cancer breakthrough pain episodes per day. The prevalence of cancer breakthrough pain can reach 51-89% [7-9], and 40-80% of patients with cancer-related pain develop cancer breakthrough pain. Cancer breakthrough pain occurs approximately three to five times a day [7,10]. The time from the onset of pain to its peak is as short as 3 min, and the duration of pain is approximately 15-30 min, with 90% of cases ending within 1 h [11,12]. It is important to understand the differences between breakthrough pain and exacerbation of persistent pain when administering the ROO formulation. In other words, if the ROO formulation is administered to patients with worsening persistent pain, the patient may mistakenly perceive the pain at the time when the effect of the ROO disappears as breakthrough pain, and the ROO formulation may be repeated. Therefore, healthcare practitioners involved in palliative care require skills that enable them to assess both types of pain. These skills are considered essential in nurses, who are stationed in the ward 24 h a day, 365 days a year, because they are the most familiar with collecting patients’ complaints. However, approximately 50% and 60% of nurses reported that they did not know anything or did not know much about the definition of cancer breakthrough pain and the frequency of cancer breakthrough pain per day, respectively. Additionally, more than 50% did not know anything or did not know much about the starting dose, which does not depend on the daily dose of opioid analgesics being given on time and the restriction of the number of doses in ROO formulations, respectively. Consequently, nurses’ awareness of the characteristics of cancer breakthrough pain and the ROO formulation may not be sufficiently widespread compared with that of physicians and pharmacists. Therefore, nurses require an increased awareness of the type of pain so they can understand whether the patient is complaining of cancer breakthrough pain or other pain. Furthermore, a thorough understanding of the pharmacokinetic characteristics of ROO formulations will lead to improved proper use of ROO formulations and may contribute to patient pain relief.
The present study has several limitations. First, since this questionnaire is based on an anonymous self-assessment, it is unclear whether high recognition and correct knowledge coincide. Second, since this questionnaire is a subjective evaluation, there is a possibility that the participants overestimated or underestimated themselves, and the reliability of their self-evaluation may not be adequate.
This study evaluated the differences in awareness between the SAO and ROO formulations based on a self-evaluation performed among physicians, nurses, and pharmacists with palliative care experience. The differences in awareness of both drugs reported by all occupations received a score of less than 5 on a scale of 0-10, and there were significant differences in awareness among occupations. These findings suggest that awareness of the proper use of ROO formulations is low, even among those with palliative care experience.
In conclusion, it is necessary to disseminate and evaluate correct information on ROO formulations based on the results of this study and to promote the proper use of ROO formulations through cooperation and information sharing among various job types.
Competing Interests
The authors declare that they have no competing interests.
Author Contributions
Eiji Kose: Conception and design; doing the field work and data
collection; data analysis and interpretation; preparation of draft
manuscript and doing revisions; overall scientific management.
Taesong An, Akihiko Kikkawa: Doing the data collection.
Nobuhiro Yasuno: Giving scholarly input in field work; providing
critique; overall scientific management.
Acknowledgments
We would like to express our deepest gratitude to the members of the Kanagawa Prefectural Hospital Pharmacists Association for their cooperation in the questionnaire survey.