1. Introduction
Gastroesophageal reflux disease (GERD) is acommon multi factor disorder of the gastrointestinal system due to a defective sphincter mechanism at the oesophagus-gastric junction [1]. It has a great medical-social importance, with a high and growing prevalence. Because of the various oesophageal and extra-oesophageal-related symptoms [2-4], GERD has an obvious negative impact on quality of life (QOL), which may even be reflected in the economy of the society [5,6].
Today, apharmacologic approach is the primary treatment for people with GERD, and the most commonly used class of drugs is the proton pump inhibitors (PPI). However, this approach is not curative and requires continuous medication. In addition, patients are advised to make lifestyle changes, which may decrease the incidence of reflux (e.g., stop cigarette smoking, reducing the consumption of coffee and fat, avoiding meals 2 hours before bedtime, and sleeping with the upper body elevated).
The only approved curative treatment today is surgical procedures such as fundoplication, which is primarily used in patients with severe GERD symptoms and combined with medication with limited effect. In a fundoplication, the gastric fundus of the stomach is wrapped or plicate around the lower end of the oesophagus, and stitched in place to reinforce the closing function of the lower oesophageal sphincter (LES). This procedure is routinely performed laparoscopically, although with some disadvantages such as irreversibility and side effects.
The role of osteopathy in understanding and treating the musculoskeletal system has been known for over 100 years [7]. During the last decades, this understanding has greatly changed by integrating techniques with influence on the visceral system.
A randomised double-blinded and controlled multicentre trial assessing the efficacy of osteopathic manual treatment (OMT) as an adjunctive treatment in elderly patients with pneumonia has been reported [8,9]. The results showed a significant reduction in hospital stay, duration of intravenous antibiotics, respiratory failure, and death with OMT compared with conventional care.
OMT used in the treatment of patients with irritable bowel syndrome (IBS) was investigated in a randomised double-blinded study [10,11]. Qualitative evaluation of depression and four symptoms including constipation, diarrhoea, abdominal distension, and abdominal pain before and after each study sequence was conducted using visual analogy scales (VAS). In addition, rectal sensitivity and transit time were recorded. One year after the end of the study, the assessment of symptoms was repeated. The results indicated that OMT improved both short- and long-term abdominal distension and pain, and reduced rectal sensitivity in IBS patients.
Fourteen patients with pancreatitis who were receiving standard care treatment were randomly allocated to the OMT group or the control group in a single-blinded clinical study [12]. The OMT standardised protocol included 10 to 20 minutes of daily treatment using myofascial release, soft tissue, and strain-counter strain techniques. The trial detected a significant reduction in hospital stay in the favour of OMT.
Recently, OMT has been introducedas a possible treatment in patients with GERD [13]. The study suggested an OMT procedure combining traction of the cardiac, mobilisation of the diaphragm and thoracic spine, and posture correction. Twenty-two endoscopically examined GERD patients were included. The study was performed as an open, observational study, without a control group. The presence of patient-reported heart burn, retrosternal pain, acid taste in the mouth, epigastric pain, and tension or pain in the thoracic spine were recorded before and after treatment. Significant reduction in the total number of GERD symptoms and “moderate” or “good” effect was detected in 77.3% of the patients. The results indicate a positive effect of OMT in the treatment of GERD, but the lack of a control group reduces the strength of the results. To the best of our knowledge, no randomised, double-blinded, and placebo-controlled study in OMT for GERD hasbeen performed. The aim of the present study is to estimate and compare the effect of the previously described OMT procedure against a placebo in a blinded and controlled manner.
2. Material and Methods
Study population: The study group comprised patients of both genders between 18 and 90 years of age with endoscopically verified GERD. Patients who had previously undergone gastric surgery of the upper gastrointestinal tract were excluded.
Study material: Thirty-four male and 24 female patients with a mean age of 50.1 years (range 27-87 years) were in the study group. Twenty-six men and 18 women were allocated to the OMT group, and eight men and six women were allocated to the placebo treatment, or control, group. The mean body mass index (BMI) was 26.1 kg/ m2, ranging from 19.5 to 36.7kg/m2. The group of patients allocated to OMT was slightly older and had a greater BMI than the control group. The mean duration of GERD symptoms and use of antacid was 10.7 years (range, 1-35 years) and 6.4 years (range, 0.2-20 years), respectively. Both these factors had a significantly longer duration in the OMT group compared with the control group. Correlation analysis detected that only BMI was significant positively correlated to the reduction in GERD symptoms and used as a covariate in the statistical analysis.
All the patients were previously endoscopically examined, and 28 patients in the OMT group and 10 patients in the control group obtained endoscopic examination just before inclusion in the study. In addition, 40 patients in the OMT group and 14 control patients had undergone radiographic examination. Only three patients did not report the use of antacids, and one patient had a hiatal hernia. General practitioners, physiotherapists, and manual therapists in the site areas recruited the patients. The regional ethical committee approved the protocol, and the patients gave informed consent to participate before the start of the study treatment.
Study design: The study was performed as a randomised doubleblinded multicentre trial with a stratified parallel group design [14]. The site was used as stratification factors. The patients were allocated (3:1)to the OMT or control group within each strata by block randomisation with a fixed block size of eight.
Study treatment: The patients allocated to OMTreceived traction of epigastric tissue. Patientis lying in supine position on the table. Operator is standing on the left side, at the level of thorax, facing the patients’ feet. Operators left hand stabilizes the patients vertebral column, at the level of the 10th thoracic vertebrae. Operator’s right hand grasps the patient’s epigastric tissue with an open palm. A longitudinal stretch is placed upon this tissue, while patient is inhaling.
While exhaling, operators hand is slowly stretching the tissue in caudal direction. This procedure is repeated three times. Then follows the mobilization of diaphragm. The patient is placed in supine position and the operator stands at the head or at the side of the table. The margins of the lower rib cage are gently grasped and pulled and pushed to its rotation restriction and held as the patient deeply breathes in and out. Sometimes a superior or inferior vector is added to the direct rotation of the thoracic cage so that there is a good palpable movement of both sides of the diaphragm during deep breathing, i.e. both leaves of the diaphragm are moving well. The position is held for about three big breaths so that the fascial preference is eliminated and the respiratory effort has normalized the movement of the diaphragm. After that follows the mobilization of the thoracic spine.
Both the left and right cruses are surrounding LES and their contractions are important for the closing mechanism. These are the muscular connection between the body and transverse of the second lumbar vertebra and LES. Contractions of these muscle fibers are supporting the closing of LES. The following technique has to be repeated three times.
The patient is lying on the left side with the operator standing on the right side, facing the back of the patient. The left hypotenar is placed on the patients sternum, the right palm on the spine, at the level of the 10th thoracic vertebrae.
The patient is asked to inhale and then slowly exhale. While exhaling, operators left hypotenar is giving a pressure on sternum in cranio-dorsal direction. The right palm is moving the spine , at the level of the 10th thoracic vertebrae in anterior direction.
At the end of exhaling, operators both hands are fixating this position. In the following inhaling process, operator is holding this extended position in proximately 10 seconds and then releases the pressure on sternum and the 10th the thoracic vertebrae.
Finally the posture is corrected. A lowered thoracic kyphosis is common among patients suffering from GORD. This position is taking tension away from the diaphragm cruse and the closing mechanism of LES. The thoracic kyphosis may cause an insufficient function and stomach acid is entering esophagus. By forcing the lowered thoracic kyphosis into extension and activating deep breathing, the tension of both cruses will increase. Patient is laying in supine position in the bed or coach.
A pillow, medium hard, not to big, is placed under the 8-12th vertebrae, forcing this part of spine into extension. Patient is now trying to relax the spine while slowly breathing in and out.
This position and exercise takes about 10-15 minutes. These treatment-techniques are repeated one timeper week.
The control patients were treated with a non-active laser pen on the lowest setting on the epigastric area, on the midline between processes us xiphoideus and umbilicus for 10 minutes, one time a week.
During these different treatment procedures, the patient was instructed how find the correct position on the treatment bench and how to breath. There was no other conversation.
Study procedure: Patients recruited to the study were clinically investigated, a complete anamnesis was obtained, and the inclusion and exclusion criteria were verified. The clinical investigation and the patient interviews were conducted by an external osteopath without knowledge of the treatment allocation. The degree of patient-reported acid taste in the mouth, heartburn, epigastric pain, chest pain, and lower thoracic pain were recorded by the patient on 10 cm VAS(15). The duration of symptoms in minutes was estimated by the patient. In addition, provocation factors and the use of antacids, H2 antagonists (H2), and PPIswere recorded.
The same external and blinded osteopath performed the patient examinations and measurements before the start of the study and 1 week after the last treatment.
Statistical analysis: All the assumed continuously distributed variables were examined by anormal quartile plot and the Shapiro Wilktest [16]. In case of deviation from normality, the variables were log transformed, and the results retransformed for presentation. The results are expressed by mean values with 95% confidence interval (CI) constructed with Student’s t test [17]. Standard deviation (SD) and total range were used as indices of dispersion. Categorised and discontinuous distributed variables were expressed in contingency tables, and changes in cross-tables [18]. Variables of “time until event” are graphically expressed by Kaplan-Meir plot and given by median with 95% CIs constructed using the Wilcoxon procedure [19]. Differences considers significant for p-value below the significance level of 5%. Comparisons of groups with regard to continuously distributed variables were performed using analysis of variance (ANOVA) with BMI and site as covariates. Categorised and discontinuously distributed variables were analysed by contingency table analysis [18]. Survival analysis was performed for comparison of the groups regarding variables such as “time until event” [19].
3. Results
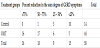
The two treatment groups were found clinically equal regarding the sum of GERD symptoms before the start of treatment (p=0.72). In the OMT group, the sum of symptoms was significantly reduced (p<0.01) from 22.0 (CI: 19.3-24.7) to 7.7 (CI: 5.6-9.7) 1 week after the last treatment (Figure 1). The sum of symptoms was also reduced, but not significantly, in the control group, from 21.0 (CI: 18.3-23.8) to 18.4 (CI: 14.2-22.7). Comparison of the groups 1 week after the last treatment regarding reduction in sum of GERD symptoms detected highly significant differences in favour of the OMT group (p< 0.01).In the OMT group, four patients were GERD symptom free 1 week after the end of treatment. An at least 75% reduction in the sum degree of symptoms was reported by 36.4 % of patients (95% CI: 22.4-52.2). The limit for minimum efficacy, defined as a 50% reduction in the sum of GERD symptoms, was obtained in 75% (95% CI: 59.7-86.8%)of patients (Table 1). The number of GERD symptoms was significantly reduced (p<0.01) in the OMT group during treatment. Ten patients had a reduction of one symptom, ten patients had a reduction of two symptoms, four had a reduction of three symptoms, and one had a reduction of four symptoms. No significant change was detected in the control group. Only one patient had a reduced number of symptoms, with one symptom reduced.
The two groups were found to be clinically comparable initially with regard to all five GERD symptoms (p>0.26). The symptoms of acid taste in the mouth, heartburn, and chest pain were found to be significantly reduced (p<0.01) during treatment in the OMT group, but not in the control group (Table 2). In addition, the degree of these symptoms and the reductions were significantly different in favour of the OMT group (p<0.01). The degree of epigastric pain was significantly reduced both in the OMT group (p<0.01) and the control group (p=0.04) 1 week after the last treatment. The degree was found to be significantly lower in the OMT group at the end of treatment compared with the control group (p<0.01), with a borderline significantly larger reduction (p=0.08). The degree oflower thoracic pain was significantly reduced during treatment in the OMTgroup, but not in the control group. However, no significant differences between the treatment groups were detected.
Initially, the two groups were found to be clinically comparable regarding the use of anti-reflux medication (p=0.55). One week after the last treatment, the use of medication was found to be significantly lower (p=0.05) in the OMT group compared with the control group (Table 2). The use of anti-reflux medication was significantly reduced in the OMT group (p=0.02), but not in the control group. No significant difference in reduction between the groups was detected (p=0.10).
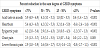
All the five recorded GERD symptoms contributed significantly (p≤ 0.005) to the reduction in the sum degree of symptoms in the OMT group (Table 3). The symptoms with the largest contribution were Acid taste in the mouth and heartburn, and these two symptoms alone explained 81% ofthe variation in reduced sum degree of symptoms.
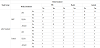
The median time of pain release before treatment was 1.5 hours in both group, with a 95% CI of 1.0 to 2.5 hours in the OMT group and 1.0 to 4.0 hours in the control group (Figure 2a). No significant difference between the groups was detected (p=0.66). After treatment, the median time to pain release in the OMT group was reduced to 0.5 hours (CI: 0.5-1.0), but was unchanged in the control group with a median time of 1.5 hours (CI: 1.0-2.0) (Figure 2b). The difference in time to pain release was found significantly shorter in the OMT group (p<0.01).
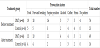
The use of anti-reflux medication was nearly unchanged in the control group. Only one patient reduced the use of antacids after treatment (Table 4). In the OMT group, 4 of 21 patients using PPIs before treatment stopped this medication. In addition, one patient stopped the H2 treatment, and four patients stopped the antacid medication.
The mean number of provocation factors before treatment was 1.6 in both groups. The most pronounced provocation factors were food intake, forward bending, and supine position (Table 5). These factors were substantially reduced in the OMT group, but nearly unchanged among the control patients.In the OMT group, 19 patients reduced the number of provocation factors with one and two patients with three factors. Five patients in the control group reduced the number of provocation factors with one and one patient with two factors.
4. Discussion
The sum of GERD symptoms was significantly reduced in the OMT group, but not in the control group. This finding demonstrates an obvious effect caused by the previously described OMT procedure [13]. A minor and insignificant reduction was obtained in the control group, but the difference in reduced sum score in favour of OMT was obvious and significant. The primary variables in the study are classified as subjective, but GERD symptoms and variables related to GERD cannot be recorded in an objective way. There is always a limitation in this kind of study, underlining the need fordoubleblinded placebo-controlled trials.
The OMT used in this study was given in three treatments with an interval of 1 week between the interventions. This dose was primarily based on clinical experiences without sufficient scientific documentation [13]. By introducing a minimum efficacy dose (MED) to obtain a percent reduction of at least 50%, the present study classified 75% of the patients as responders to OMT. Of these responders, 12% were free of GERD symptoms and 48.5% obtained a reduction of at least 75%. From a clinical point of view, this is promising, but underlines the need for a dose-response study of OMT. By optimising the combination of number of OMTs and the interval between each treatment, an increase in the responder rate might be expected.
The largest significant reduction and difference between the groups was found in the symptoms of acid taste in the mouth, heartburn, and chestpain. These variables were significantly reduced in the OMT group, but not in the control group, and significantly in favour of OMT. Of these three variables, acid taste in the mouth and heartburn were the most dominant, and explained more than 80% of the variation in sum of GERD symptom reduction. Epigastric pain and lower thoracic pain were also found significantly to be reduced in the OMT group. However, epigastric pain was also significantly reduced in the control group, and the difference between groups was not significant. The symptoms that start first in the lower oesophagus are the last to disappear. The influence of acid irritationin this area requires more time before an effect can be expected. The lower thoracic pain comes later and stays longer because of the anatomically close connection tothe columna vertebralis and the efferent neurons in this area [20]. However, nearly 50% of the patients in the present study did not report lower thoracic pain. This reduced sample size may explain the difference between the groups.
As previously described, the primary variables related to the clinical treatment effect of GERD are subjective. However, the change in use of anti-reflux medication might have supporting value. All the GERD patients included in the present study used such medication either daily or occasionally. This use was nearly unchanged among the controlgroup, but was significantly reduced in the OMT group. Four of the 21 patients using PPIs before treatment stopped this medication; one patient stopped the H2 treatment; and four patients stopped the antacid medication. This finding supportsthe significant reduction in the GERD symptoms. Considering the economic benefits and side effects of drugs, this is a promising result.
Several anatomic and physiologic factors normally prevent GERD [21]. The closing mechanism, the cardiac sphincter, is supposed to open only when food is transported through the oesophagus into the ventricle. Insufficiency of this mechanism causes acid content from the stomach to ascend into the oesophagus. This closing mechanism does not have an anatomic sphincter, but has more of a sphincter function. This is explained by a special muscular architectonic structure of the 3 to 5 cm of the terminal oesophagus. When the tension in this area is increased, a screwing motion starts [22]. The OMTs used in this study has a direct effect on the LES by increasing the tension in the lower part of the oesophagus [13]. The clinical practice experience also indicates that people who working in a position in which they bend forward for long periodstend to have GERD. This position decreases the tension in the terminal oesophagus and provokes stomach acid reflux.
Ravinder et al. [21] states that the anti-reflux barriers include two sphincters, LES and the diaphragmatic sphincter with unique anatomic configuration at the gastroesophageal junction. Impairment of these mechanisms promotes GERD. The neuromuscular mechanisms that maintain the tonic or reflex contraction of these sphincters are essential for their anti-reflux behaviour.
The median time to pain release after OMT treatment was significantly reduced to 0.5 hours, but unchanged in the control group, with a median time of 1.5 hours. This finding supports that the manual intervention has a positive effect on the closing mechanism of LES, increasing the tension in the lower part of oesophagus. Food intake, forward bending, and supine position wereinitially the most provoking factors for GERD symptoms, and were equal in the two groups. These were substantially reduced in the OMT group, and nearly unchanged among the controls ubjects, supporting the activation of the LES closing function.
The treatment used in the control group might be a weakness of this study. The control subjects were treated with a non-active laser pen on the epigastric area for 10 minutes every week during the study. However, the sham treatment may have had a positive effect on the patients’ subjective experience. It is reasonable to assume that the obtained effects include a considerable placebo effect [14].
The present study has a short follow-up period, but long-term follow-up studies after OMT are obviously required. Based on this short follow-up study, 11% of the patients were without symptoms 1 week after treatment. In addition, the majority of the patients reported a significant reduction in GERD symptoms. The present study does not prove OMT as a curative GERD treatment, but it might in some cases give the patients relief of symptoms. A larger scale randomised controlled trial with long-term follow-up might give valuable information and answers to this item.
5. Conclusion
OMT seems to have a significant effecton GERD symptoms and positively stimulating the LES function. OMT might represent a positive contribution to existing GERD treatment.
Competing Interests
The authors declare that they have no competing interests.