1. Introduction
There is a high prevalence of depressive disorders worldwide, with over 350 million people suffering from depression globally [1]. A meta-analysis of 84 observational studies in 44 countries showed that the global prevalence of anxiety disorders was estimated at 7.3% [2]. The estimated yearly cost of treating depressive and anxiety disorders in Europe is approximately €3,826 and €1,804 per single case [3]. The pharmaceutical cost of depression treatment is a relatively minor component of the overall costs [4-6]. Simon et al. in 1995 investigated the individual components of overall medical expenses in detail and reported that the mean costs for depressed patients are much higher as compared to non-depressed patients with regards to outpatient laboratory/radiology tests, with imaging tests accounting for higher costs than with blood tests [7-8]. These studies highlighted the relevance of radiographic and blood tests of depressed patients to healthcare services.
Low adherence to medication is another factor which is known to increase medical expenditure. It has been shown that although high adherence to medication in chronic disease is associated with increased costs of drug prescriptions than non-adherence, this is offset by a significant decrease in overall medical costs [9-10]. Several studies investigated the link between clinical outcomes and therapy adherence, suggesting that high adherence to therapy is necessary for patients to benefit from their medication [11-15]. Cantrell et al. carried out a study to evaluate the effect of medication adherence on medical costs in a cohort of 22,947 patients of whom 48% were diagnosed with depression, 29% with anxiety disorder and 23% with both [16]. This study found that adherence to ADs was associated with significantly lower overall yearly medical costs than non-adherence [16]. Given that the costs of diagnostic tests are a non-trivial part of the overall medical costs, it is plausible that the frequency and resulting costs of these tests are also associated with adherence to antidepressant therapy.
The main aims of this retrospective population-based study using an electronic medical record database were to: a) describe and compare the frequency and cost of different types of diagnostic tests in patients with depressive/anxiety disorders newly treated with ADs vs. nonusers of ADs in a general population from Southern Italy during the period 2006-2011; b) evaluate the effect of AD treatment adherence in patients with depressive/anxiety disorders on the appropriate use of diagnostic tests, stratifying by AD class where possible.
2. Materials and Methods
2.1 Data source
Data was extracted from the Arianna database from 2006-2011. This database was set up by the Caserta Local Health Agency in Southern Italy in the year 2000 and currently contains information on a population of almost 400,000 inhabitants who are registered with 300 general practitioners (GPs). Participating GPs record data during their daily clinical practice using dedicated software and send complete and anonymous clinical data of their patients to the Arianna Database on a monthly basis. The Arianna database can be linked to the claims databases of the catchment area through a unique and anonymous patient identifier. The quality and completeness of submitted clinical data is evaluated based on defined acceptable ranges. Any data outside of these ranges is investigated and backsubmitted to each participating GP in order to receive immediate feedback. GPs failing to meet standard quality criteria are excluded from epidemiologic studies. Overall, 123 GPs covering a population of 168,397 inhabitants met these standard quality criteria and were included in the study.
Data concerning demographics as well as drug prescriptions, hospitalization and out-patient diagnostic tests were extracted. Diagnostic tests and hospitalization are coded by the ninth edition of International Classification of Diseases, Clinical Modification (ICD- 9 CM), while data on drugs is coded according to the Anatomical Therapeutic Chemical (ATC) classification system and consists of information on all drugs reimbursed by National Health System along with the linked indications for use. So far, the Arianna database has been shown to provide accurate and reliable information for pharmacoepidemiological research [17-25].
2.2 Study population
AD users were included in the study if they were alive and had a diagnosis of depression and/or anxiety (ICD-9 CM codes: 293.84, 296.2, 296.20, 296.21, 296.23, 296.3, 296.30, 296.30, 296.31, 296.32, 296.33, 296.34, 296.35, 296.36, 300, 3000, 300.00, 300 300.02, 300.x, 309.21, 311, 311 S, 311/0, 311.0, 313, 313.0, 313.1, 313.9, V111) and were incident antidepressant drug users during the years 2006-2011(no use in the year prior). As we aimed to evaluate the effect of adherence on different AD classes separately, patients who started the treatment with more than one AD belonging to different classes were excluded. The index date (ID) was defined as the date corresponding to one year after the first prescription of AD. Up to two patients not prescribed ADs (as comparator groups) were matched to every AD user on sex and age (±2 years). The index date assigned to non-users was the same as for AD users. The comparator group was not intended to act as a control group with respect to AD users but to provide an indication of patient characteristics and diagnostic requests at baseline by the general population. All patients were included only if they had at least one year of database history prior to the start of AD treatment and at least two years of follow-up after the ID (Figure 1).
The first year of treatment was used to characterize the treatment adherence of AD users. The requests for diagnostic tests were measured in the two years following the ID because it would be expected that any potential effects of adherence on the former are more likely to be related to adherence level once it is ascertained that the patient has a high, medium or low-adherence to their therapy; the first year of treatment served to provide this ascertainment.
2.3 Exposure
The following ADs were identified and classified based on ATC classification as: selective serotonin reuptake inhibitors (SSRI; N06AB*); tricyclic antidepressants (TCAs; N06AA*);other ADs included noradrenergic and specific serotonergic antidepressants (NaSSAs): mirtazapine (N06AX11) and mianserine (N06AX03); noradrenaline reuptake inhibitor (NRI): reboxetine (N06AX18); serotonin-norepinephrine reuptake inhibitors (SNRIs): duloxetine (N06AX21), venlafaxine (N06AX16) and other N06AX* excluding those previously mentioned. A posteriori TCAs were not considered in the analyses due to the very limited number of TCA users with high adherence (N=7).
2.4 Adherence measurement
For each AD user the total number of defined daily doses (DDDs) prescribed during the first year of treatment was calculated starting from the first prescription. This value was divided by 365 as a proxy measure of treatment adherence (i.e. proportion of days covered). Based on this measurement, AD users were then classified as having high (>80%), medium (20-80%) or low (<20%) treatment adherence.
2.5 Covariates
Demographic and clinical characteristics of the patients included in the study were evaluated any time prior to the first AD prescription. The following co-morbidities were identified using ICD 9-CM codes: diseases of the circulatory system, including hypertensive disease (401-404.x), ischemic heart disease (410-414.x), cerebrovascular disease (430-438), other types of heart disease (427-428.x), diseases of arteries, arterioles, and capillaries (440-449); dyslipidemia (272.x); type 2 diabetes (250.x); obesity (278.0); chronic kidney disease (250.4, 285.21, 585.x, 586.x, 583.x, 403.x, 404.x, 996.73, V45.1, V56.x); chronic liver disease (570.x-573.x); thyroid disease (193.x, 226.x, 240.x-6.x, 648.1); cancer (140.x-208.x); osteoarthritis (715.x); rheumatoid arthritis (714.0-714.4x); chronic obstructive pulmonary disease (COPD) and asthma (496.x, 491.2.x, 493.x) and dementia (290.x, 291.20, 292.82, 294.1, 294.2, 331.0, 331.1x 331.2, 331.8). The number of co-morbidities was quantified and categorized as 1, 2, 3-4 or >4 co-morbidities.
In addition, we evaluated the concomitant use (within 90 days prior to the study entry) of the following drugs: anti-thrombotic drugs (B01*); salicylates and ticlopidine (N02BA*, B01A, C05-06); antihypertensive agents (C02*, C03*, C07*C0-9*); cardiac therapy (C01*); corticosteroids (H02*); non-steroidal anti-inflammatory drugs (NSAIDs) (M01A*); psychotropic drugs: anti-Parkinson agents (N04*); antiepileptic drugs (N03*); antipsychotics drugs (N05A*); opioid agents (N02A*) and cholinesterase inhibitor agents (N06DA*). The number of concomitant drugs was measured and categorized as <3, 3-5, 6-8, >8 drugs.
2.6 Diagnostic tests
Data on out-patient laboratory and radiological tests as well as specialists’ referrals which were requested between the index date and the two following years were extracted using ICD9-CM codes (Table 1). As regards laboratory tests we identified the total number of blood tests, including specific blood tests (e.g. thyroid-related blood tests). Radiological tests were categorized as: a) computerized tomography (CT) scans; b) magnetic resonance imaging (MRI); c) X-ray; d) ultrasound scans; e) electrocardiogram (ECG); f) nuclear medicine, and g) others, which also include medical procedures (e.g. tooth extraction, magneto-therapy, and dental panoramic radiography).
Requests for visits to the following medical specialists were also identified: a) cardiologists; b) oculists; c) dentists; d) gynecologists; e) neurologists, and f) diabetologists. The cost of each diagnostic test/ specialist visit was derived from the Campania Regional diagnostic tests formulary, which was used within the Arianna database catchment area.
Indicators of diagnostic test appropriateness for cardiac ultrasound, head and neck CT, ECG and cardiological visits were developed based on the known standard indications for the use of such tests. An algorithm to classify diagnostic test appropriateness was developed based on standard indications and pre-disposing risk factors for the requests of these tests. The indications/pre-disposing risk factors for which these tests may have been requested were identified from: a) medical events recorded among indications of use for drug prescriptions as well as among primary and secondary hospital discharge diagnoses; b) drugs used as proxies (e.g. cardiovascular drugs as proxy of cardiological diseases) (Table 2). Within the algorithm, requests for the above-mentioned diagnostic tests during the two years following the ID were considered as potentially inappropriate in the absence of the indication/pre-disposing risk factor for the diagnostic test any time prior to and within 90 days after the date of the diagnostic test. For example, a request for an electrocardiogram in the absence of a diagnosis of heart disease and/or prescription for cardiovascular therapy 90 days before or after the electrocardiogram would be considered potentially inappropriate.
2.7 Statistical analysis
Demographic and clinical patient characteristics were reported as mean and standard deviation (or median with lower and upper quartiles) or as absolute and relative frequencies for continuous and categorical variables respectively. For new users of ADs only, such characteristics were stratified according to their drug classes and level of treatment adherence and were compared among adherence levels using Pearson Chi-Square and Kruskal-Wallis statistics for categorical and continuous variables, respectively. If the expected frequencies were less than 5, the Fisher exact test was used instead. A test for linear trends across treatment adherence levels was further performed using Cochran-Mantel-Haenszel and Spearman correlation statistics for categorical and continuous variables respectively.
The absolute and relative frequencies of patients who requested at least one diagnostic test within two years of follow-up was further calculated within each treatment adherence level (for AD users only) and for each specific diagnostic test, along with the median number of total tests requested by each patient. A co-morbidity-adjusted estimation of the number of patients who requested at least one test was carried out by fitting a multivariable logistic regression model, where adherence level and number of co-morbidities (using the following groups: 0, 1, 2, 3-4 and >4 co-morbidities) were included as categorical covariates and deriving their adjusted means. A test for linear trends across treatment adherence levels was performed including adherence level as continuous covariate into the logistic regression.
Moreover, a co-morbidity-adjusted estimation of the total diagnostic test-related costs per individual for new users of ADs and non-users who requested at least one diagnostic test was provided through ANOVA models using the log-transformation of costs as outcome and both number of co-morbidities and adherence treatment as categorical covariates. Tests for linear trends across treatment adherence levels were performed including adherence level as continuous covariate into the ANOVA models.
The absolute and relative frequencies of requested inappropriate tests among the total number of requested tests were also estimated within each treatment adherence level (AD users only) and for each diagnostic test, separately. The association between the inappropriate request of diagnostic tests and cost of diagnostic tests per individual was described using the Mann–Whitney U test.
2.8 Results
From a source population of 168,397 inhabitants, 3,225(1.9%) incident users of ADs with anxiety/depressive disorders and 6,205 (3.7%) matched patients from comparator group (i.e. non-users of ADs) were identified during the years 2006-2011 (Figure 1). Almost two thirds of AD users were female and had mean age of 56.7±16.4 years.
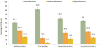
Overall, 55% of AD users had low adherence during the first year of therapy (Figure 2). The highest proportion of patients with high adherence was observed for SSRI users (17.2%), while TCA users were mostly low adherent (82.8%), with very few users being highly adherent to TCA therapy (2.7%). No statistically significant difference by age and sex was observed across AD classes and different levels of adherence, apart from 65-80 year old SSRI users who were more likely to have medium-high adherence (Table 3). In comparison to non-users, AD users had a much greater burden of co-morbidities as well as larger number of concomitant drugs. SSRI users with dementia or ischemic brain disease were more likely to have high adherence to treatment; on the other hand, a diagnosis of osteoarthritis was associated with low SSRI treatment adherence. In general, SSRI users with no co-morbidities have the highest adherence, while those with 3-4 co-morbidities were significantly more likely to have lower adherence (p<0.05). Higher levels of adherence to both SSRIs and other ADs were associated with concomitant use of other psychotropic drugs and (only for SSRIs) antithrombotic and antiplatelet drugs, while use of corticosteroids and NSAIDs was associated to low SSRI treatment adherence.
Overall, higher adherence to ADs was modestly associated with fewer requests for diagnostic tests (Table 4). In particular, SSRI users with low adherence had a slightly greater number of requests for ultrasound and blood tests as compared to those with high adherence (p-value <0.05). This trend remained similar after adjustment for number of co-morbidities, although it lost its statistical significance. The proportion of patients with at least one diagnostic testamong SSRI (76.7%) or other AD (71.7%) users with high adherence was higher than non-users (66.8%) but lower than SSRI (78.9%) or other AD (80.0%) users with low adherence.
As shown in Table 5, the median (with interquartile range)costs related to diagnostic tests were lower in AD users with high treatment adherence than those with low adherence for the following tests: CT scan (€86.3;€83.2-169.4 vs. €115.2;€83.2-175.6), X-ray (€22.2; €15.5- 40.3 vs. €31.0; €17.3-50.1) and blood tests (€113.4;€54.8-205.0 vs. €122.2;€65.4-224.2). Adjusting by the number of co-morbidities, the estimated mean cost of the total number of diagnostic tests per individual was lower in AD users with high treatment adherence (€171.9; 95%CI: €154.7-191.1) than those with low adherence (€185.8; 95%CI: €175.3-197.0), although findings were not statistically significant.
The proportion of inappropriate diagnostic tests requested for SSRI users during two-year follow-up was slightly higher in patients with low adherence than in patients with high adherence (Table 6). Specifically 38.4% of all head and neck CT scans requested for SSRI users with low adherence were potentially inappropriate, as compared to 23.3% for those with high adherence. Similarly, 12.7% of cardiological visits and 11% of ECG requested for SSRI users with low adherence were potentially inappropriate as compared to 7.8% and 8.5% respectively, for those with high adherence.
3. Discussion
To our knowledge, this is the first population-based study evaluating and comparing the frequency, appropriateness and cost of diagnostic tests and specialist visits among patients with anxiety/depressive disorders in relation to the levels of AD treatment adherence. Other studies have demonstrated that depressive or anxiety disorders are associated with significant healthcare costs in general. The majority of patients with depression/anxiety in the present study were females, as described elsewhere [25]. In line with previous studies, we observed that over 50% of AD users had low adherence to treatment during the first year of therapy [26-27]. SSRIs, the most commonly prescribed ADs, were used with the greatest level of adherence as compared to other ADs [28-30]. In contrast, TCA users had the lowest adherence, probably as consequence of the limited tolerability, as demonstrated by a large body of scientific literature [31].
Our analysis on the association between adherence by AD class and frequency of diagnostic tests showed that higher levels of treatment adherence to SSRIs were associated with fewer requests for blood tests and ultrasound scans. Other diagnostic tests were not found to be associated with SSRI adherence. There were too few patients prescribed ADs other than SSRIs to reach any conclusive results from this population. Our findings therefore suggest that the relevance of AD adherence to healthcare costs does not seem to hold for all the diagnostic tests investigated and for non-SSRI users. Low adherence to ADs was only marginally associated with higher costs.
It has been previously shown that patients with depressive/anxiety disorders use more healthcare resources, including diagnostic tests. An Italian survey on the 6-month prevalence of depression evaluating the socio-economic consequences of the illness found that depressed patients used healthcare resources more extensively (e.g. physician visits drug therapy and instrumental examinations) compared to nondepressed subjects [32]. Another study observed that older people with symptoms of depression had higher average diagnostic test costs and other healthcare resources than patients without any symptoms of depression [33]. These findings were confirmed in Canada in two studies which analyzed the same association between healthcare costs and depression/anxiety [34-35]. Our findings confirm this trend, which can be explained by the likelihood that in general, nondepressed persons are healthier overall than depressed persons. While all the above studies provide valuable information on the increased healthcare costs in depressed/anxious patients, they did not investigate the impact of AD treatment adherence on the healthcare costs related to laboratory and radiological tests, such as MRI and CT scan. Finally, none of these studies investigated the link between antidepressant utilization and the use of potentially inappropriate diagnostic tests. This is particularly important because inappropriate diagnostic tests not only incur additional costs [7-8] but may represent an excess and avoidable exposure to radiation and radioactive substances which can be carcinogenic with repeated exposure.
The main finding of this study is that patients with lower adherence to ADs, mostly SSRIs, had a modestly higher chance of having an inappropriate diagnostic tests compared to highly adherent patients. This may be because high adherence to therapy is linked to positive clinical outcomes and/or to lower health care costs [9-10]. Being aware that other factors could have also influenced the request for such tests as well as their appropriateness, we adjusted for several covariates and used multiple approaches to investigate potential trends in diagnostic test utilization. The weak association despite extensive statistical analysis suggests that although not insignificant, antidepressant adherence is likely to act in concert with other factors increasing the inappropriate use of diagnostic tests.
This study has several strengths as well as limitations. The use of the Arianna database provides access to a large general population and reflects actual clinical practices as recorded during GP routine care. The GP setting is particularly suitable to study AD use, asin Italy patients receive ADs free of charge only through GP prescriptions irrespective of whether the AD therapy is initiated by GPs or specialists working in either public or private sector. In addition, including only AD users with a diagnosis of depression or anxiety limits the risk of including patients with a short-term indication of AD use (e.g., neuropathic pain) who are likely to have selectively low adherence. As for diagnostic tests, only those ordered through GPs are not charged to citizens. Such an incentive increases the chances of capturing diagnostic tests within the general practice Arianna database. Since it is likely that depressed persons are less healthy overall than non-depressed persons it would be plausible for the former to have more diagnostic test requests than the latter, which nevertheless could be considered appropriate. The approach used in this study, whereby an algorithm was used to classify diagnostic test appropriateness based on medical diagnoses and prescriptions for diseases associated with indications for diagnostic tests, i.e. the quality of diagnostic test requests, was intended to minimize the risk of misattributing the quantity of diagnostic tests as inappropriate. Nevertheless, by investigating the quality and quantity of diagnostic test requests among AD users and non-AD users, our findings provide a relatively detailed description of diagnostic test requests in a general population of AD users.
On the other hand, some limitations warrant caution. It is possible that findings from the catchment area of Caserta are not generalisable to the rest of Italy or to countries with a healthcare system different to that in Italy. Since prescription data was used in this study, the actual consumption of medicines cannot be ascertained [36]. It is possible that the frequency and cost of diagnostic tests were underestimated if patients underwent diagnostic tests in private clinics which were not affiliated to the national healthcare service. Since this is more likely with depressed/anxious patients who are not successfully treated, use and costs of diagnostic tests in AD users with low treatment adherence may have been underestimated.
4. Conclusion
This population-based study found that a greater adherence to AD treatment in patients with depressive and anxiety disorders is associated with a slightly reduced number (and costs) of diagnostic tests. Although a modest effect of AD adherence on inappropriate diagnostic test requests was observed, adherence is likely to be one of several factors affecting the request and appropriateness of diagnostic tests.
Competing Interests
The authors have no competing interests with the work presented in this manuscript.
Author Contributions
GT designed the research methods, contributed to the interpretation of results and wrote the manuscript. FP carried out data management, data analysis, contributed to the interpretation of results and wrote the manuscript. JS, CF and APC contributed to the interpretation of results and wrote the manuscript. FG, VIand AF carried out data management, data analysis, contributed to the interpretation of results and wrote the manuscript. CT and DUT made substantial contributions to acquisition of data.