1. Background
The periocular region is susceptible to numerous benign and malignant neoplasms. The most common types of skin cancer in the periocular region are basal cell carcinoma, followed by squamous cell carcinoma and sebaceous gland carcinoma [1] . The annual incidence of nonmelanoma skin cancer is increasing, being Australia and Brazil who record the highest incidence rates [2,3]. In Spain, the incidence of nonmelanoma skin malignancies has doubled or tripled in both sexes between 1978 and 2007 [2] .
Periocular skin malignancies may present differently, behave more aggressively, and pose more management challenges than malignancies at other cutaneous sites. Extent of skin cancer is often difficult to assess prior to surgery [4,5].
Management of periocular malignancies involves high cure rate along with maximal preservation of healthy tissue [6] . The standard of care for surgical treatment of skin cancer comprises total tumor excision with microscopic tissue margin control [1,7]. Microscopically controlled surgery (MCS) aims to assure complete removal of a malignancy with histological confirmation while preserving as much of the adjacent tissues as possible [5] . Consequently, tumors can be completely removed in a single procedure carried out in one or more stages. As MCS requires special training, multiple procedures, more time and costs and hence generally less available because of practical limitations in the service delivery, it is reserved for predicted highrisk cutaneous tumors such as aggressive behavior or those situated in anatomic sites where local recurrences are more common [3,4,7] . This retrospective case series distinguishes clinical-practice management trends in periocular nonmelanoma skin malignancies.
2. Methods
2.1 Study design and patients
A retrospective descriptive analysis of the medical records of 37 consecutive patients requiring surgical excision of periocular non-melanoma skin malignancies (Figures 1 and 2) was performed in patients seen in Oculoplastic section of the Department of Ophthalmology at Hospital de l'Esperança - Hospital del Mar between July 2010 and January 2017. We conducted a search in our institution health records system using International Disease Classification, Ninth Revision Procedure codes 08.11 (Biopsy of eyelid), 08.2 (Excision Or Destruction Of Lesion Or Tissue Of Eyelid),08.22 (Excision Of Other Minor Lesion Of Eyelid) and 08.24 (Excision of major lesion of eyelid, full-thickness) [8] . Patients with benign neoplasms or not attended in the Department of Ophthalmology where excluded. Periocular malignancies were those concerning the medial canthus, lateral canthus, upper eyelid, lower eyelid or a combination of these locations with or without eyelid margin involvement. Primary lesions were defined as those that had not occurred previously, whereas recurrent lesions were those that had been excised previously by other surgeons and had reappeared, requiring further excision by the oculoplastic section.
2.2 Patient management
Patients were referred by comprehensive ophthalmologists and dermatologists for assessment of periocular lesions. Informed consent was obtained for excision of all lesions. Excision was performed under monitored local anesthesia. Surgery was executed by two oculoplastic surgeons (A.M.P and M.C.P.) in an ambulatory surgery schedule in the Hospital de l’Esperança. Surgical technique involved excising periocular tissue with the incisions perpendicular to the eyelid margin and maintaining 2-to 4-mm clearance on all sides of the tumor macroscopically. The histopathologic diagnosis of all nonmelanoma skin malignancies was established at the Hospital del Mar.
Intraoperative section examination of tissues handle involved the following key steps. First, the pathologist was contacted to discuss the case with the surgical team before the removal of the periocular skin lesion. Second, cardinal margins were identified using sutures and the specimen was represented in diagram to provide proper orientation of the specimen by the pathologist. Third, critical margins (i.e. margins adjacent to canaliculi and conjunctival surfaces and clinically suspicious margins) were sampled to ensure entire margin inclusion. Forth, tissue samples were processed and stained with hematoxylin and eosin. The tumor was identified and any parts of tumor involvement at the margins were indicated. Finally, the margin areas with tumor involvement were revealed to the surgeon and surgeon and pathologist discussed the need for further excision. Re-excision of margins was performed, again with perpendicular incisions to the eyelid margin.
Reconstruction was executed by oculoplastic surgeons (A.M.P and M.C.P.) with direct closure where possible, or with flaps, or grafts if required, the same day of tumor excision once free margins were confirmed (Figures 2 and 3).
3. Results
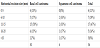
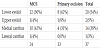
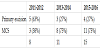
This study involved 37 patients (20 females and 17 males). The median age was 72 (range 39-99) years. The pathological diagnoses included basal cell carcinoma (BCC) in 30 patients (10 morpheaform, 1 nodular, 1 not assessed), squamous cell carcinoma (SCC) in 6 patients and sebaceous gland carcinoma (SCG) in 1 patient. In both BCC and SCC groups, most of the patients were 75 years or older (53% and 100%, respectively). Six (16%) patients (5 BCC and 1 SCC) had recurrent tumors. The original tumor in these cases had been treated by simple excision. Two patients with lower lip basal cell carcinoma had another primary basal cell carcinoma (1 supraciliary and 1 in the upper lip). MCS was performed globally in 24 (65%) cases (18 BCC, 5 SCC and 1 SCG). The lower eyelid was the most common tumor location for BCC (57%) and the medial canthus for SCC (67%). Surgical excision technique frequency depending on anatomical site is shown in table 1. Temporal evolution of excision surgical technique rate during study period is shown in table 2. Mean horizontal excision size was 13 mm, detailed tumor excision size and histopathological type distribution is shown in table 3. Flap and flap and graft combination were the most frequent reparation types (24% each), detailed reparation technique frequency depending on anatomical site is shown in table 4.
4. Discussion
The clinical incidence of cutaneous cancers is increasing with population aging. This is most significant for nonmelanoma malignancies [4] . In our study global mean age was 72 years, which is an older age group than previous literature [5,9-13].
Several studies have found the incidence of both SCC and BCC to be higher in males than in females [5,12]. In our retrospective review, there was a male:female ratio of 1 in both BCC (14:16) and SCC (3:3) subgroups. This could be explained by a small sample size.
In our series, tumor characteristics were in accordance with previously published being basal cell carcinoma the most commonly excised tumor (81%) followed by squamous carcinoma (16%) and sebaceous gland carcinoma (3%) [4,5, 9-11,13].
The anatomic location of BCC tumors in this series was similar to other previous reports being the lower eyelid (54%) the most common site for tumors. Lateral canthus was the least common location (3% of BCC subgroup), which is consistent with the literature. The medial canthus was the most common tumor location for SCC (67%), which differs from the previously reported [10,12].
The most commonly performed surgical procedures for the management of nonmelanoma skin malignancies are primary surgical excision and Mohs micrographic surgery (MMS), which is a MCS technique [7] . In our study, MCS was performed globally in 65% of cases but there was an upward trend in the use of the MMS technique during the study period, going from 38% of cases at the beginning (2011-2012) to 73% of cases at the end of the study period (2015-2016).
Due to its highly complex anatomy and function, reconstruction of the eyelids is one of the greatest challenges in facial plastic surgery. In our study, flap (24%) and flap and graft combination (24%) were the most frequent reparation techniques. O'Halloran et al. found differences between oculoplastic surgeons and Mohs surgeon repairs being combination repairs more often used by oculoplastic surgeons [5] . Our study has some limitations. This study was a retrospective study, the sample size was small and the follow-up duration was relatively short. Prospective randomized controlled trials to compare proper management of periocular nonmelanoma malignancies should be necessary. In conclusion, microscopically controlled surgery for the management of periocular malignancies has increased in our hospital during 2011-2016. It confirms histopathological diagnosis and free margins of excision allowing periocular reconstruction on the same day. Microscopically controlled surgery safes healthy tissues which are essential in the eyelid and it decreases patients’ morbidity.
Competing Interests
The authors declare that they have no competing interests.
Author Contributions
Study conception and design, acquisition of data and analysis and
interpretation of data: AMP, FDG
Drafting of manuscript and critical revision: AMP, FDG, MCM,
MCP.