1. Introduction
The introduction and rapid development of digital radiography imaging systems include an understanding of a wide range of topics related to computer-based technologies. These include, for example, characteristics of digital images, computer components (input and output devices, central processing and arithmetic logic units, magnetic and optical data storage), digital detector construction and function, digital image processing and analysis, and picture archiving and communication systems (PACS) and computer network topologies. Therefore, when transitioning from film-based radiography to digital radiography, appropriate training and education are essential needs for successful implementation of the new imaging tools. In this regard, the ICRP provided an outline for a “general education and training aspects in digital radiology” in publication 93: “Managing Patient Dose in Digital Radiography” [1]. The literature clearly lacks such materials [2-4].
It is clearly apparent from these topics that a new paradigm for understanding digital radiographic imaging technologies was needed. The transition from film-based to digital radiography and the resulting lack of education/training created a state of confusion for technologists and radiologists alike [5]. Subsequently, the lack of understanding the essential physics and technology of digital radiography prompted various recommendations on the need for relevant education and training in this technology [3,4,6-11].
A recent research of the literature for studies exploring the nature and scope of digital radiography education for technologists revealed only two recent studies and one in 2005 [2-4]. The two most recent studies recommend that-there is a clear and widespread need for comprehensive education in digital image technology at a practical level for radiologic technologists [2] and findings from this study suggest that there is a need for formal education, continuing education, and manufacturer training [3].
2. Literature Review
CR is a complex technology and requires an understanding not only a certain degree of physics, but also technical concepts as well, as described earlier in this chapter. For example, the nature of the wide exposure latitude, the physics of Photostimulable Phosphers (PSP) and Photostimulable Luminescence (PSL), image processing algorithms, EIs, and the problem of exposure creep [12] all require a good knowledge and understanding to use the CR system. Such understanding is essential for the correct and appropriate use of the CR system in an effort to optimize dose and image quality, to ensure the ALARA philosophy is adhered to in routine daily operation [13].
During the transition from film-based radiography to digital radiography in the early years, coupled with the subsequent rapid development of Digital Radiography, user education and training have been identified as critical components in dose-image quality optimization [1,2,5,14-17].
In 2004, the ICRP discussed the education and training needs for radiographers, radiologists, and medical physicists. In this regard, the ICRP [1] supported the outline of topics for the general education and training aspects of digital radiology as proposed by the European DIMOND consortium [4]. These topics include image acquisition, transfer, and analysis; quality control, digital visualization, workstations, image presentation, transfer and archiving; and patient dose management.
A search of the literature using the sources mentioned in the beginning of this chapter and search terms such as CR/DR, education and training in CR, use of CR in clinical practice, and survey of technologists revealed only two studies. The first study is one by Nyathi et al. [3] who conducted a survey of digital radiography practice in four South African hospitals for the purpose of capturing information on radiographers ‘familiarity and preferences with digital radiography. A questionnaire was designed to capture data on familiarity, preferences, knowledge, and workmanship of radiographers working in a digital radiology department, using a cross-sectional research design.
The questionnaire included closed and open-ended questions and was sent to 205 participants including qualified and student radiographers. It was first sent to the medical physicist at each of the four hospitals surveyed (via email), who made hard copies and subsequently distributed it to all participants. The response rate was 31% (63 out of 205), 10 students and 53 radiographers. Descriptive statistics including summary measures and frequency tables were used to analyze the data. Of the four hospitals, only two used CR systems; the other two used DR (flatpanel systems) from manufacturers such as Philips, Siemens, General Electric, Toshiba, Agfa, Fuji, Kodak, and Konica-Minolta. Of the 31% who completed the questionnaire, only 15% (8) has four or more years of experience with FS radiography.
The questionnaire focused on “three-factors of interest,” namely; training, comparison between digital and PSP radiography, and preference in digital radiography. The training factor included responses to formal education in digital radiography (61%); formal training in digital radiography quality control (QC) (16%); reading of the digital radiography system manual (23%); and easier to perform retakes in digital radiography (55%). In comparing digital radiography with FS radiography on superior spatial resolution, superior image quality, more doses to the patient, and wider dynamic range, the responses were 71%; 74%; 51%; and 91% respectively. Furthermore, preference in digital radiography for collimation rather than cropping and the use of grids were 89% and 100% respectively.
The authors conclude that while radiographers are familiar with digital radiography in terms of advantages and disadvantages in clinical practice, QC procedures for digital radiography are lacking in radiology departments. Additionally, the authors emphasize that there is a need for “formal education, continuing education, and manufacturer training with respect to QC as institutions make the transition from conventional FS radiology to digital radiology” [3].
The second survey study on digital radiography education is one by Morrison et al. [2]. The goal of this study was to “evaluate knowledge of image quality and dose management in pediatric digital radiography among radiologic technologists in the US”. The authors noted that the survey was sponsored by the American Society of Radiologic Technologists (ASRT) and the Education subcommittee of the Image Gently Computed Radiography/Direct Radiography committee.
A 23-item questionnaire designed to capture data on the nature of the education received by technologists on image quality and dose management in digital radiography particularly in the pediatric population, was sent to 493 registered technologists. These individuals were selected from both dedicated children‘s hospital and hospitals serving the needs of both adult and pediatric patients. The questions focused on image acquisition, QC workstations, quality assurance (QA), radiation exposure, and education in digital radiography.
The results of this survey study showed that for image acquisition, 38.6% use grids for thicker patients such as adult patients. Furthermore, technologists who worked with pediatric patients were less likely to use automatic exposure control (AEC). 76% of technologists use lead markers compared to 74% who used electronic markers 25% or less of the time. For the use of the QC workstation, the response indicates that electronic collimation is used regularly. 69.9% of technologists indicate that electronic collimation has no impact on the exposure indicator (EI) value. For quality assurance (QA), the focus was on monitoring repeat rates, and in this respect participants identified patient motion, poor positioning, “clipping of anatomy,” and artifacts as common causes of repeats.
In addition, respondents stated that repeat rates are few. 90.6% of participants indicate that radiation exposure values were predetermined for patients at the respective hospitals. The causes of increased exposure dose to patients were identified as patient motion and poor positioning, as well as incorrect exposure technique selection and incorrect gonadal shielding. Furthermore, technologists received their education from on-the-job training and from equipment vendors. Hospital dose reduction methods varied. 42.8% noted that dose reduction methods were emphasized all of the time, while 11.4% noted that dose reduction methods were never emphasized. 27% on the other hand reported that dose reduction was emphasized most of the time. There was a statistically significant higher percentage of technologists who worked in a children‘s hospital, who reported that dose reduction was emphasized all of the time (p < 0.05). The authors conclude that there is a clear and widespread need for comprehensive and practical education in digital image technology for radiologic technologists, especially those engaged in pediatric radiography [2].
In summary, only two research studies were found that investigated education and training issues in digital radiography. These studies were lacking specifically in the following areas relating to CR Physics and Technology knowledge components; the use of CR technology in practice; confidence in using the CR imaging system in practice; attitudes towards CR use in practice and specific use of the EI in practice.
3. Purpose of the Study
The purpose of this study was to explore the physics and technology knowledge components of CR, as well as the confidence and attitudes of technologists in using the CR imaging system in clinical practice. This investigation uses the survey research design to capture data from a purposeful (convenient) sample of technologists in British Columbia, Canada. Furthermore, this survey approach captures data on the specific use of the EI in clinical practice.
4. Materials and Methods
The data collection for the survey study used an instrument to capture data on the degree of knowledge of CR physics and technology, the level of confidence and attitudes of radiographic technologists in using CR systems for imaging adult patients in clinical practice. this objective, a non-probability sampling approach, specifically the qualitative purposeful sampling referred to as snowball sampling was used.
The following procedures were used to in the conduct of the survey:
- The revised survey questionnaire (as a result of the pilot test) was prepared for online electronic distribution using the Vovici survey software (www.vovici.com).
- The researcher of this thesis met face to face with 19 clinical instructors (registered radiologic technologists with a wide range of clinical experience) who are involved in the BCIT Medical Radiography program. These instructors are associated with 19 hospitals in British Columbia which are all clinical sites for the program.
- They were informed about all aspect of this research and were asked to participate in the survey phase of the study. In addition, they were each asked to solicit the participation of technologists who use the CR imaging system in each of their radiology departments.
- They all agreed to participate and provided their email addresses. Later they were all contacted and reminded to seek other technologists who would agree to participate. 5. Subsequently, 103 technologists agreed to participate in this survey.
- Using their email addresses, the online electronic survey was sent to each individual for completion. Three reminders were then sent to those who did not respond in the first request. This was done during a 94-day period from Tuesday, October 19, 2010 to January 21, 2011.
- Seventy-one participants completed the survey, which was subsequently analyzed by the Vovici survey software.
The ethics approval for this study was obtained by the Ethics in Human Research Committee, Charles Sturt University (CSU). In addition, the following statement was written on the questionnaire:
“… By completing this survey you will have provided us with your consent to use your responses for this research. Please be ensured that any information or personal details gathered from this survey are confidential, and that neither your name nor any other identifying information will be used, or published without your written permission”
Finally, all data collection forms have statements regarding the participation of individuals in the study to assure them that confidentiality is strictly maintained. Descriptive statistics are used to analyse the data collected from surveys and present the results in a meaningful way. In this study, the specific descriptive statistics used to analyse the data sets collected from the survey, were the number of individuals (N) who participated in the study, the mean and the standard deviation. It is important to note that the results obtained from the sample will not be used to generalize to the population, a fundamental limitation of descriptive statistics.
Since a questionnaire could not be found in the literature that reported validity, face validity for this particular instrument was obtained by asking three expert digital radiography physicists to review it and all agreed that it met the validity requirement for this study. To measure the reliability Cronbach‘s alpha is used and it has become the most widely used objective measure of reliability [18]. Cronbach‘s alpha was used to provide a measure of the internal consistency of the survey instrument used in this thesis. Such consistency indicates the extent to which all items on the instrument measure the same concept or construct and hence it is connected to the inter-relatedness of the items….reliability estimates show the amount of measurement error… [18]. This error is the correlation of the test instrument with itself. If this correlation is squared and then subtracted from 1.00, the result is the index of the measurement error. Cronbach‘s alpha is expressed as a number between 0 and 1. Tavakol and Dennick [18], provides a simple example to calculate the alpha. They note that if a test has a reliability of 0.80, there is a 0.36 error variance (random error) in the scores (0.80 x 0.80 = 0.64; 1.00 – 0.64 = 0.36) (p 53). Acceptable alpha values may range from 0.70 (acceptable) to 0.95 (excellent) [19]. All descriptive statistics were calculated using the SAS statistical package. Furthermore, the written responses to the last question (number 15) on the survey questionnaire:
“As a user of CR equipment in the clinical environment, what other topics do you believe are essential for effective use of CR imaging systems in the hospital?” was analyzed only for CR topics that are not listed in question 11 (knowledge components) and question 14 (use of the EI).
5. Results
5.1 Response Rate
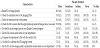
An online questionnaire was sent out to 103 technologists in several regions in BC including 27 urban and rural hospitals. The response rate was 68.9%. This response rate was attributed to three email reminders to those who did not complete the questionnaire, the first and second times. A detailed breakdown of the demographic characteristics of the study population is shown in Table 1.
Based on the results presented in Table 1, the majority of the study participants were female (77.5%). In addition, most of the participants were within the age range of 40 and above (47.9%), followed by 18.3 % who were within the range of 26–30 years old. The educational level of the participants varied, with the majority (38%) having a diploma of radiology followed by 21.1% who had a ongoing continuing education. Furthermore, the majority of the respondents worked 16 years or more (39.4%) as a registered technologist, while 60% of respondents worked in a medium scale hospital. 47.1% indicated that their current job title was ‘Grade 1 technologist’.
The number of years worked in CR clinical practice ranged from 8.7% (1 year) to 44.9% who worked 4–6 years. The most common educational method received by 50.7% of the sample was delivered by the vendor, with the majority of respondents receiving less than 2 hours of instruction in CR theory with hands-on training on the system (48.6%), followed by 22.9% of those who had 2–4 hours of theory/hands-on training in CR.
Finally, the demographic characteristic of the year in which participants received their training showed that one technologist had training in 1992, while the majority of technologists (18.6%) received training in 2004, followed by 12.5% in 2005, and 7.8% in 2007. The most recent training was received in 2009 by 6.25% of technologists. Seven participants did not complete this question.
5.2 Degree of knowledge of CR physics and technology results
This section of the survey questionnaire listed 28 items intended to capture data on the degree of knowledge of CR physics and technology, using a 4-point Likert scale (to limit the participants from consistently providing ‘neutral responses’).
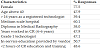
The frequency distribution of the responses to the CR physics and technology knowledge components are shown in Table 2.
The participants were asked how much information they received in their education/training on the topics listed in Table 2. In this regard, respondents indicated that:
- A good amount of information was received on exposure techniques for different body parts, selection of the correct body part, selection of the correct processing algorithm, image display on the monitor, image post-processing operations (windowing), exposure indices, and vendor acceptable ranges of EIs for body parts. The only topic in which the majority of respondents indicated greater than 50% was selection of the correct body part.
- Little information was received on the CR Reader and its major components, how the CR Reader detects and digitizes the PSP signal, image pre-processing, EI exposure standardization, image quality descriptors, Detective Quantum Efficiency (DQE). CR artifacts, optimization of Image Quality and Radiation Dose, and the effects of fogging.
- No information was received on the Physics of Photostimulable Luminescence, types of CR phosphors, how to use the EI for managing patient dose, DQE and its relationship to image quality and dose, exposure “creep”, and Quality Control (QC) tools, Reject Analysis, and QC Tests for CR.
Cronbach‘s alpha for this question on the knowledge components of CR was 0.96 which indicates a high measure of consistency, meaning that the respondents have answered the question in the same manner.
5.3 Confidence in using the CR system results
Question 12 of the survey questionnaire was designed to obtain data on the level of confidence in using the CR system, using a 5-point Likert scale. The ratings were labelled “very high”; “high”; “moderate”; ”low”; and “very low.”
The frequency distribution results for question 12 dealing with the level of confidence in using the CR imaging system on several items is shown in Table 3.
- Majority of participants rated their confidence as high to very high for using the CR workstation software to perform processing on the image such as windowing, annotation, etc., using the CR workstation hardware, using the CR system in general, using the CR reader to process the IP, and using the CR IP in positioning the patient and x-ray parameters in the radiography room.
- Approximately 27%, 26%, and 20% of respondents indicated a moderate confidence level on using the software to process QC tests, using the EI as part of a QC program, using the EI to reduce radiation dose respectively.
- The item with low (30%) and very low (21%) was item k (Table 3) that is using the software to process QC tests.
Cronbach‘s alpha for the same question was 0.91, indicating a high measure of consistency. In all of the ANOVA analyses for Q3, Q4, Q7, and Q9 on the dependent variable Q12 , the p-value (Pr > F) is greater than 0.05, meaning that there is no statistical evidence to reject the null hypothesis. The conclusion drawn, therefore, is that there is no statistical evidence to suggest that there is a difference in mean scores for question 12 between levels of question 3, question 4, question 7, and question 9. The calculated p-values were 0.81, 0.19, 0.43, and 0.70 for questions 3 (education level); question 4 (years worked as an RTR); question 7 (years worked in CR); and question 9 (hours of education received in CR) respectively.
5.4 Attitudes: Extent of agreement/disagreement results
The purpose of question 13 of the survey questionnaire (to what extent do you agree or disagree with the following statements?) was to capture attitudes of the respondents to 14 items related to CR imaging. A 5-point Likert scale was used, with ratings that ranged from “strongly agree” and “agree” to “disagree” “strongly disagree”; and “no idea.” The responses to the 14 items will be reported in terms of frequency distribution, internal consistency, and analysis of variance (ANOVA).
The frequency distribution results for the responses to question 13 are shown in Table 4. A strong agreement (> 50%) was indicated for items a, d, i, and j. Additionally, strong disagreement (> 50%) was indicated only for item f. Furthermore, while 60.6% of respondents indicated “no idea” for item m, 52.1% had “no idea” for item n Cronbach‘s coefficient alpha for question 13 was 0.54 indicating a low level of reliability, suggesting that one or some of the questions were not answered consistently for all participants.
Question 13 of the survey also sought to examine whether age (Q2), level of education (Q3), years of working as a registered technologist (Q4), years of working in CR (Q7), and hours of CR education/training received (Q9) had any effect on attitudes of the study participants. The ANOVA analyses were used to compare the mean total scores for Q13 responses between levels of Q2 (age range for example), Q3, Q4, Q7, and Q9; and the results provided no statistical evidence to reject the null hypothesis (the mean total scores for all levels of Q2, Q3, Q4, Q7, and Q9 are equal) since the p-value (Pr > F) is not less than 0.05. The conclusion, therefore, is that there is no statistical evidence to suggest that there is a difference in mean total scores for Q13 between levels for Q2, Q3, Q4, Q7, and Q9.
The intent of question 14: How often do you use the CR Exposure Indicator (EI) in Clinical Practice? was to explore how respondents used the EI in routine daily work in the hospital. A Likert scale was used to rate 9 items on a 5-point scale ranging from “often”; “sometimes”; and “seldom” to “never” and “no idea. The responses to the nine items will be reported here with respect to frequency distribution, internal consistency, and analysis of variance (ANOVA) similar to questions 11, 12, and 13.
The frequency distribution results for the responses to question 14 are shown in Table 4.
It is quite clear from the results in Table 4 that the respondents often check the EIs to ensure that the appropriate exposure technique (mAs) was used (78.9% rated this item (d) as “often”) and that the EI is used often to relate it to image quality (item a) as rated by 60.6% of the respondents. Furthermore most of the respondents had “no idea” of item f – use of the EIs in dose audits (54.3%); item h – use of the EI to calibrate the CR imaging system (56.5%); and item i – use of the EI in dose-image quality studies in their departments (49.3%). In addition, Cronbach‘s alpha for question 14 was 0.80 indicating a high level of reliability or consistency in the way subjects responded to the items.
Question 14 of the survey was also concerned with relating the responses to age (Q2); education level (Q3); years of working as a registered technologist (Q4); years of working in CR (Q7); and hours of CR education/training received (Q9). ANOVA was used to compare the mean total scores for Q14 responses between levels of Q2, Q3, Q4, Q7, and Q9, and the results show that the overall test for the ANOVA was significant (p < 0.05) but the analysis failed to detect a difference between any two levels of hours of education/training received. This means that there is some linear combination or levels that are different, and that there is no evidence of difference in the levels.
5.5 Other uses of the EI in clinical practice results
Question 14 of the survey questionnaire also included an openended statement ‘Please state any other uses of the EI in your department. There were only four responses as follows:
- We have a QC program although I do not personally take part in the program.
- To my knowledge there isn‘t a lot done with our CR QC since I stopped doing it last year.
- The EI is a useful tool to help determine different factors of an image.
- Our new fluoro/CR room gives us the skin entrance dose for each image.
It appears from these responses that numbers 1 and 2 above indicate that the EI is used in QC? Responses 3 and 4 above do not appear to have any clarity of meaning.
5.6 Other uses of importance in CR education/training
The final question (Q15) of the survey questionnaire included the following format:
“The following are some of the important topics in CR education/
training.
Physics of Photostimulable Luminescence (PSL);
The CR Reader and its major components;
How the CR Reader digitizes the IP;
Image pre-processing (e.g., histogram analysis);
Image post-processing operations (e.g., windowing);
Exposure Indicators (EI) for your system;
Relationship of the EI to the radiation dose used;
Vendor acceptable ranges of EIs for various body parts/views;
Guidelines for the use of EIs in Quality Control;
Exposure “creep”;
Optimization of the Image Quality and Radiation Dose;
Quality Control Tools, Reject Analysis, and QC Tests for CR.
As a user of CR equipment in the clinical environment, what other topics do you believe are essential for effective use of the CR imaging system in the hospital?
The responses are provided below as follows:
The survey study results showed a 68.9% response rate. The demographic results indicated that the respondents were mostly female above 40 years of age and registered technologists with a varying number of years of work experience in CR. Most of the respondents indicated that their CR education/training was provided by the vendor for less than two hours of theory/hands on training. The degree of knowledge of CR physics and technology varied from little information to no information received on certain topics. No information was received on the physics of photostimulable luminescence, types of CR phosphors, using the EI to manage patient dose, the Detective Quantum Efficiency (DQE) and its relationship to image quality and exposure creep for most of the respondents.
The internal consistency (Cronbach‘s alpha) results of 0.96, 0.91, 0.54, and 0.80 for questions 11 (how much information was included in the knowledge of CR education and training), 12 (level of confidence in using elements of the CR system), 13 (extent of agreement/disagreement with attitude statements), and 14 (use of the EI in clinical practice) respectively showed that the respondents answered the questions in the same manner, except for question 13.
The ANOVA results showed that there was no evidence to suggest that there is a difference in mean scores for questions 12 and 13 between levels of questions 2 (age), 3 (level of education), 4 (years of work as a registered technologist), 7 (years of working in CR), and 9 (hours of education/training received in CR). For question 14, the overall test for ANOVA was significant (p < 0.05) but the analysis failed to detect a difference between the two levels of hours of education/ training received. Finally, no significant issues/ideas for other uses of the EI in practice and other topics of importance to CR education/ training (beyond those given in the questionnaire) were expressed by the respondents.
6. Discussion
The results of this survey will be discussed with respect to the response rate, demographics, knowledge components of CR, confidence in using the CR system, attitudes toward CR imaging, specific uses of the EI in clinical practice, and other topics of importance in CR education/training other than those given in the survey questionnaire.
The high response rate of 68.9% could be attributed to use of a strategy whereby three sets of reminders were sent via email to those participants who did not respond to the first, second, and third requests. The reminders stressed that participation in the study was vital and important to providing recommendations for improving the education/training in CR and particularly its use in clinical practice. Furthermore, the reminders also stressed that since they were practitioners using the system they were in a good position to suggest ideas that would contribute to the development of the knowledge components of CR technology and its practical use in the hospitals.
The goal of capturing demographic data was to provide the background variables and the results are not surprising for this sample of the population of diagnostic radiology technologists. In order to capture data on the survey questions relating to knowledge components of CR, confidence and attitudes in using CR in clinical practice, the variables of age, level of education, years working in CR, and hours of CR education/training received were critical when examining any associations between independent and dependent variables.
The demographic characteristics with the highest percentage of responses are shown Table 5.
The data above provides insights into the responses provided to other questions listed in the survey questionnaire. It is not surprising that the respondents were mostly female, since more females than males tend to work in this profession. Although only 38% of the respondents have a Medical Radiography diploma, the remainder (62%) have a wide range of education from advanced certification from the professional association (Canadian Association of Medical Radiation Technologists = CAMRT) and continuing education to degrees in science and degrees in radiography. The question of whether this range of education would influence confidence in using the CR system and attitudes toward CR imaging will be explored later in this chapter.
It is interesting to note that most of the respondents were from medium scale hospitals (compared to large scale urban centers and small scale rural centers). This is not surprising since there are more medium scale centers in the province of British Columbia (BC).
The percentage of responses from Grade 1 technologists (47.1%) would indicate that CR imaging is performed more than any other radiological examination on a routine basis by these technologists who are often also classified as "entry level" technologists.
Finally, it is not alarming that most participants received their education/training in CR from the vendor (manufacturer). This is common practice in BC hospitals and indeed a routine practice of vendors. It is understandable, however, that vendors cannot dedicate long training periods when the equipment is installed, and this could explain why most respondents received less than 2 hours of instruction (48.6), followed by those who received 2–4 hours of theory and hands-on training (22.9%). These findings appear to parallel those of Morrison et al. [2] where the majority of respondents indicated that their primary source of education in CR was mainly the vendor (23.5%). Furthermore, it is interesting to note that in a study by Peer et al. [4] that when technologists were asked to indicate the amount of training hours in CR reasonable for initial and continuing education on a 2–3 year basis, most respondents indicated 25+ hours maximum to a minimum of 5–10 hours. This perception is clearly worthwhile when considering the length of time for adequate education/training of technologists in a new imaging modality before use in clinical practice.
The literature review identified only three papers that attempted to capture data on the knowledge components of CR education [2-4]. These studies did not address in any detail the knowledge components of the physics and technology of CR essential to clinical practice. This study was designed to capture more knowledge components than those of the previous three studies mentioned above.
Question 11 of the online survey questionnaire addressed 28 topics which in the opinion of the author of this dissertation are topics that have been emphasized in review papers and classical textbooks (for example, Seeram [12]) on digital radiography (as detailed in Chapter 2). These topics range from physics concepts, equipment, image quality and dose management considerations, and exposure indicators to CR artifacts, quality control (QC) issues including QC test tools, QC tests, and reject analysis for CR systems.
It is interesting to note from the results for question 11 that the topics with the highest percentage of responses did not include any physics topics outlining the basis of how CR works, but rather topics such as exposure techniques for different body parts, selection of the correct body part, and correct processing algorithms. In addition, other topics included image display on the monitor, vendor acceptable ranges of EIs for different body parts. Perhaps this finding could be attributed to the fact that most vendors provide this education/training via their applications specialist who is generally not a medical physicist or a biomedical engineer but rather a technologist who has received special training on the vendor‘s equipment. These training sessions are usually more “hands-on” training rather than a description of the more physical principles and technology knowledge components of CR. Furthermore, since most of the respondents indicated that their training was less than two hours, it is not surprising that there is not enough time to cover the range of topics identified in Table 2.
Most of the respondents noted that little information was received on selected topics such as the CR reader and its components and function, EI standardization, image quality descriptors, DQE, CR artifacts, and optimization of image quality and dose. These are important topics essential to understanding how CR works and how it can be optimized to meet the ALARA philosophy. This is a concept often stressed by vendors in an effort to encourage users to establish their own range of EIs for the various examinations done in their departments.
Finally, most of the respondents indicated that no information was received of topics such as the physics of photostimulable luminescence, phosphor types, how the EI can be used to manage patient dose, the DQE and its relationship to patient dose and image quality, exposure creep, QC test tools, QC tests, and reject analysis. These findings are somewhat similar to only a few topics, such as image quality-dose relationship, physical properties of the system, and the basics of image acquisition explored by Peer et al. [4]. Furthermore, the Morrison et al. [2] study identified a lack of “comprehensive and practical education in digital image technology for radiologic technologists” (p. 602). This finding is consistent with the findings of this study.
Question 11 showed a high measure of internal consistency or reliability (Cronbach‘s alpha = 0.96). This is an important finding in that it showed that all respondents answered the question in the same manner. This also supports the notion that all respondents in BC hospitals appear to have received similar degrees of the knowledge components of CR imaging systems.
It is clearly apparent that these findings for question 11 have highlighted a notable lack of knowledge (knowledge gaps) in the theory of CR (physics and technology) and equally a lack of hands-on training time for practical use of the system. This is a significant finding that has implications not only for formal educational programs (at universities and colleges, for example) but also for training programs provided by both the vendor and the hospital, in the form of “inservice” method of delivery.
The literature review revealed that this is the first study to explore the level of confidence in using the CR imaging system in clinical practice. The level of confidence was captured by question 12 using a 5-part Likert scale to rate 11 items on the survey questionnaire. In addition, one of the goals of the survey was to explore whether education level (question 3), years of work as a registered technologist (question 4), years of work in CR (question 7), and hours of education/training in CR (question 9) made any difference to the level of confidence in using the CR system.
The percentage in decreasing order of specific use characteristics (extracted from Table 3) for which most of the respondents rated “very high” on the Likert scale are shown in Table 6.
The “very high” degree of confidence in using the items in the above Table could be attributed to the fact that these tasks are embedded within the daily routine practices when using the system. This finding is consistent with those of Eley et al. (2008) who reported that confidence in Information Technology (IT) (which is related to digital radiography including CR) has been associated with the frequency with which it is used. On the other hand, tasks that are not a part of routine daily activities such as the ones related to a QC program were obviously rated with a “low” level of confidence. Additionally, those tasks rated as “high” to “moderate” level of confidence, such as using computers (45.7%), assessing CR image quality (42.9%), and using the vendor‘s recommended EI values for different body parts, are all embedded in the routine daily activities of the CR technologist.
It appears then that performing routine tasks on a daily basis seems to create an individual who becomes “well versed” in these skills. This obviously has a profound impact on their level of confidence in performing the skills.
The ANOVA statistical test to examine whether education level, years of work as a registered technologist, years of work in CR, and hours of education/training received in CR have any impact on confidence levels showed no evidence of this. For example, those who worked less years as a registered technologist and in CR, had a higher education level, and had more training time in CR, had the same confidence level as those who worked longer in CR and as a registered technologist, had a lower level of education, and less education/ training time in CR. The conclusion here is that a link between the above independent variables and the level of confidence in using the CR system in practice was not found.
This is the first study of its kind to explore the extent of agreement/ disagreement to 14 items on the survey questionnaire to capture attitudes (question 13) of technologists using the CR imaging system in clinical practice, using a 5-point Likert scale.
The extent of agreement/disagreement or “no idea” is linked to the education/training received by the participants. Since most participants had < 2 hours of training (48.6%) by the vendor (50.7%), it is not surprising that topics such as dose audits and calibration of the automatic exposure control system were not addressed, perhaps due to the “complexity” of these topics?
A close examination of the results indicates that most participants (> 50%) showed agreement with several items. These include the decreasing order of the percentage of participants rating items as “strongly agree” and “agree”:
- The EI is a useful tool to assist in controlling the radiation dose to patients (86.3%)
- The EI should always be used to assess image quality (74%)
- CR improves patient care because of its ability to adjust a low exposure to produce an image that appears to be acceptable to the technologist (72.8%)
- Technologists should not change the EIs as they appear on displayed images (62.9%)
- Technologists must always use the correct image processing algorithm for the body part and view under examination (60.5%)
- CR technology makes imaging patients more interesting compared with film-based imaging (57.1%), and
- Technologists must perform image post processing before sending displayed images to the PACS (54.9%).
It is understood that the first three items above showed agreement among the vast majority of respondents, since the EI is always displayed on the monitor for every image. In addition, Table 5-2 indicates that a good deal of information on the EI and EI ranges for body parts was provided to respondents during their education/training by the vendor. Furthermore, such a strong response to the extent of agreement on items relating to the EI is due to the fact that the EI provides the technologist with a visual cue as to the use of appropriate exposure factors. This is a daily routine activity of the technologist. Another point with respect to the level of agreement with the item regarding the use of the correct image processing algorithm for the body part stems from the fact that respondents indicated that very much information on this topic was received during their education session.
Finally, it is not surprising that since very much information was received on image display on the monitor, there was agreement on the image post processing of displayed images before sending images to the PACS. The level of agreement on the items mentioned above could have been influenced by the extent of the coverage during education/ training sessions.
The level of disagreement was strong and rated by most participants (> 75%) for three items on the survey questionnaire. Specifically, these are:
- CR does not require the use of correct exposure technique factors (kV, mAs) (90%)
- A shoulder algorithm can be accurately used to process a chest body part (86.9%)
- CR "exposure creep" is not considered a problem for the patient, since the radiologist must always obtain high quality images (74.6%)
- One possible explanation of the above results could be linked to the notion that since very much
- Radiation dose audits are always conducted using the EIs (60.6%)
- The automatic exposure timer is calibrated to the exposure class of the CR system (52.1%)
- EIs are always calibrated as part of a QC program (45.1%)
- CR QC tests are a routine part of imaging in my department (21.9%)
Since the above are more complex topics in CR education, they might not be covered in the short training sessions (< 2 hours) for most of the respondents and thus have an impact on the attitudes of technologists using the CR system.
The ANOVA test showed that age, education level, years of work as a registered technologist, years of work in CR, and hours of CR education/training received had no statistical impact on attitudes of the respondents. A possible explanation of this finding is perhaps related to the notion that the tasks in performing a CR examination is purely mechanical in nature, requiring more psychomotor skills rather than cognitive skills.
The major steps requiring mechanical skills (the act of performing a motor task) are illustrated in Figure 1.
The internal consistency for question 13 (addressing attitudes) was 0.5 (Cronbach‘s alpha) indicating a low level of reliability in how respondents answered this question. It is quite clear, however, that respondents have a good level of agreement on the use of the EI and on using the correct processing algorithm for the body part under study. Furthermore, respondents also appeared to have a grasp of the item that states "CR exposure creep is not considered a problem for the patient…" since there was a strong level of disagreement with this statement.
To date no studies have explored in detail the use of the EI by technologists in clinical practice and, therefore, this study can be viewed as the first study of its kind.
The responses of the participants were captured by question 14 of the survey -“How often do you use the CR EI in clinical practice?” A Likert scale was used to rate nine items on a 5-point scale ranging from “often, “sometimes, and “seldom” to “never” and “no idea”. Cronbach‘s alpha for this question was 0.80 reflecting a high level of reliability or consistency in the manner the participants responded to the nine items. It is clear that there were two major findings from the analysis of the results:
(a) A greater percentage of respondents (95.8%) use the EI to relate
it to image quality and to ensure that the appropriate exposure
technique (mAs) was used.
(b) A good majority of the respondents had no idea of whether the
EI was used for dose audits (54.3%), for calibration of the CR system
(56.6%), and for dose-image quality optimization studies (49.3%).
The finding noted in (a) above would appear to reflect that vendors stressed the concept of EI with respect to image quality and the use of appropriate exposure factors. Additionally, these two tasks are done routinely on a daily basis and hence have become an "automatic" response during the conduct of the CR examination.
On the other hand, the response of "no idea" to the finding labelled as (b) above should provide to employers and educators alike that these are important concepts for users to be familiar with, and should be included in a curriculum of studies for CR.
Finally, the overall test of ANOVA was significant (p < 0.05) for this question, but the analysis failed to detect a difference between age, education level, years of work as a registered technologist, years of work in CR and the method of CR education received, and the frequency of use of the EI in clinical practice. Could these findings be due to the notion that the use of the EI to assess image quality on the monitor and to check whether the appropriate exposure factors were used are simple tasks and performed routinely on a daily basis? Perhaps the more complex tasks of using the EI in calibration of the CR system and in dose audits require much more comprehensive coverage in education/training programs.
This is the first study to explore this topic reflected in question 14 of the survey. An analysis of the responses showed there were no additional uses (other than the ones listed in question 13) provided by the respondents. Perhaps the respondents felt that the uses listed in question 13 were already exhaustive.
This is the first study to capture additional topics (content) on CR education/training from those who use the system in the hospital (clinical practitioners) on a daily basis.
The responses were captured in an open-ended question (question 15) of the survey, and stated as:
- "As a user of CR equipment in the clinical environment, what other topics do you believe are essential for the effective use of the CR imaging system in the hospital?"
Only 22 of the 71 respondents provided written statements. These statements did not identify any additional topics than were listed in question 11 (28 topics related to the knowledge components of CR physics and technology), with the exception of “basic troubleshooting” identified by one respondent. Another written statement by one respondent was “more in-depth training for CR”.
It is clear from these responses that the range of topics identified in question 11 captured the full scope of the knowledge components for CR education, and that respondents could not think of additional topics. The topic of “basic trouble-shooting” (from one respondent) could be considered in future curriculum for CR education; however, this task is usually a function of biomedical engineers either employed by the hospital or by the vendor.
7. Major Findings
There were two major findings of the survey study. First, the results showed that CR education and training are lacking and there are significant and important knowledge gaps in several specific content areas. These include, for example, the physics of photostimulable luminescence, phosphor types, the use of the EI in practice, the detective quantum efficiency (DQE) and its relationship to image quality, and exposure creep. Secondly, the survey results also showed that age, education level, years of work as a registered technologist, years of work in CR, and the method and hours of CR education and training did not have any statistical impact on confidence and attitudes in using the CR system and on use of the EI in clinical practice.
The survey study needs to be repeated with a larger sample size, perhaps on a national scale (a Canada-wide study) to include different CR imaging systems, using a random sample instead of a convenient purposeful sample (a valid sampling tool in survey research) of technologists. Such a study should sample not only hospitals but educational institutions to capture data on the knowledge content of CR physics and imaging technology. The results of such a study would validate and perhaps enhance the recommendations for CR curriculum based on the findings of this study. Furthermore, such a study should also focus on how technologists acquire additional skills and how improvement of current skills in CR system use may be recognized.
8. Recommendations
That CR education/training includes the following topics to ensure a comprehensive understanding of the physics and technology of CR imaging:
- Limitations of Film-Screen Radiography
- Terms Synonymous with CR
- A Brief History of CR
-
The CR Imaging System: Basic System Configuration
-Image Acquisition
-Image Processing
- Image Display, Storage, and Communications -
Basic Physics of CR Image Formation
-Nature of Photostimulable Phosphors (PSPs)
-Latent Image Formation
-Physics of Photostimulable Luminescence (PSL)
-RSL Characteristics -
CR Technology
-The CR Imaging Plate (IP)
-The IP Imaging Cycle
-The CR Reader: Types
-The CR Reader: Scanning Technologies
-The CR Workstation: Characteristic Features
-Computer Networking and CR -
Digital Image Processing in CR
-Preprocessing Operations
-Postprocessing Operations -
Exposure Control in CR
-IP Response to Exposure
-Exposure Indicators
-Exposure Indicator Standardization
-Exposure Indicator Guidelines for Quality Control (QC) -
Image Quality Descriptors
-Spatial Resolution
-Density Resolution
-Noise
-Detective Quantum Efficiency (DQE) -
Image Artifacts
-Definition
-Sources of Artifacts
-Artificial Reduction -
Continuous Quality Improvement (CQI)
-Quality Assurance (QA)
-Quality Control (QC)
-Tools and Phantoms for QC Testing
-Parameters for QC Monitoring in CR
-Tolerance or Acceptance Limits
-Specific Examples of CR QC Tests
-Dosimetry Fundamentals
-Dose-Image Quality Optimization Strategies
In view of the development of the standardized EI followed by clinical implementation, vendors should establish a detailed plan to educate technologists and radiologists alike, about the standardized EI specifically by:
- Training technologists on how to use the vendor‘s software to implement the EI standardization,
- How to compensate when the DI values is not within the acceptable range,
- How to approximate the dose to the patient.
9. Conclusion
The third useful insight relates to the knowledge gaps identified in the survey study. The survey results provided a clear view of the various topics needed for an understanding of the physics and technology of CR imaging. These topics could be used to a "curriculum" for CR at the technologist level.
The final insight offered by the results of this study is that even though factors such as age, method and hours of CR education/ training, and experience in working in CR imaging did not have a statistical significance on the confidence and attitudes in using the CR system, a good understanding of the knowledge components of CR identified herewith can only lead to a wise and effective use of the CR imaging system in clinical practice.
Competing Interests
The authors have declared that no competing interests exist.