1. Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a novel coronavirus that causes the condition known as Coronavirus Disease 2019 (COVID-19) [1]. Since its discovery, COVID-19 has spread rapidly and has been declared a pandemic by the World Health Organization. As of March 2021, unpublished data indicate that there have been over 116 million cases and 2.5 million deaths worldwide, illustrating the devastating impact of this disease [2].
Common symptoms of COVID-19 include those often seen in respiratory infections. In severe cases, mortality may result [1]. While some infected individuals may display only minimal or no symptoms, others may experience long-term symptoms and persistent functional deficits [1,3] . Some researchers have referred to this phenomenon as “long COVID” [3].
While there is a paucity of evidence on the issue of “long COVID”, preliminary data from Carfi et al. (JAMA 2020) suggest that many patients report continued symptoms or deficits - weeks or even months after the onset of symptoms [3,4] . In such instances, patients may benefit from a structured rehabilitation program to facilitate safe and effective participation in activities of daily living (ADLs) and to prevent further complications. In this paper, we assess one instance of such a program.
2. Methods
The study is a retrospective single-subject design. The study complies with the Declaration of Helsinki and has previously been waived by a research review board. We obtained written informed consent from the participant. We have complied with the Health Insurance, Portability, and Accountability Act requirements of the institution for disclosure of protected health information.
The patient is a 77-year-old female who was referred to an outpatient physical therapy center for continued deficits after COVID-19. She was initially hospitalized for 7 weeks with acute respiratory distress syndrome and subsequent intubation. Over the duration of her care, she also experienced kidney failure, sepsis, and a deep vein thrombosis in her right upper extremity. She then stayed for 5 weeks at a long-term rehabilitation facility. She was medically cleared to begin outpatient rehabilitation 20 weeks after her initial hospitalization. At baseline, she reported increased fatigue with ADLs and required assistance from a caregiver for household chores and mobility. She reported that she was previously able to complete all ADLs independently.
The patient participated in 8 outpatient physical therapy visits over 5 weeks. This program was designed by a large provider of outpatient services specifically for individuals after COVID-19 infection. The outcomes measured in the program included the following: the 6-minute walk test (6MWT), 5 times sit-to-stand test, single-limb balance, manual lower extremity muscle testing, and the Patient- Reported Outcomes Measurement Information System (PROMIS) Global-10. Due to time constraints, the 6MWT was collected at the second session. These measures were selected as they have been previously studied in older individuals or individuals with cardiopulmonary complications [5-11].
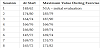
Between the initial and final visits, the patient participated in six one-hour sessions consisting of: (1) aerobic exercise, (2) progressive gait training, (3) lower quarter strengthening exercises, (4) functional task training, and (5) balance exercises. Sample exercises can be found in Table 1. Heart rate and oxygen saturation were monitored during each exercise, while blood pressure was measured at the beginning and end of the session and after a position change.
Two physical therapists were involved with patient care. With the exception of the 6MWT, which was deferred to the second session, the baseline and final measurements were conducted by the same physical therapist. Prior to patient care, both physical therapists completed a standardized program consisting of 4 hours of didactics regarding recovery and reconditioning for individuals affected by COVID-19 to increase safety and efficacy of care. Competency testing was performed to ensure the learning objectives associated with the training were achieved by the treating clinicians.
3. Results
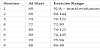
The 6MWT measures the distance that a patient can ambulate in 6 minutes and is a reliable assessment of aerobic capacity and potential cardiopulmonary dysfunction [12]. The patient improved the 6MWT by 79 meters, which exceeds a minimal detectable change of 58.21 meters that has previously been reported [5]. At baseline, she required the use of a front-wheeled walker, but she was able to complete the task without any assistive device when measured again at the penultimate session.
The 5 times sit-to-stand test measures the speed at which an individual stands and sits 5 times. It is a reliable measure of functional strength and potential fall risk [7,8] . The patient did not demonstrate a meaningful change in her test results [8], as she scored 1 second slower at the re-evaluation than at the initial evaluation. However, she initially required upper extremity assistance to rise, whereas she performed this test without upper extremity support during re-evaluation.
Single-limb balance is another measure to determine potential fall risk [9]. At baseline, the patient was unable to perform the test on either limb. At discharge, she was able to complete 4 seconds on the left limb and 8 seconds on the right limb. She did complete up to 16 seconds on the left leg and up to 12 seconds on the right leg during the treatment sessions. Because patients who score less than 5 seconds are associated with an increased fall risk [9] we can surmise that the patient may have decreased their risk of falling.
The physical therapist used the standard procedures for manual muscle testing (MMT) as described by Kendall and McCreary [13]. The primary motions tested were hip flexion, knee extension, knee flexion, and ankle dorsiflexion. The patient scored at least 4+/5 with each MMT at discharge. Existing research suggests appropriate testretest reliability of MMT [10]. Because the same examiner performed testing at the re-assessment, there is increased confidence that the patient demonstrated improvements in their strength. The results of all outcomes are in Table 2.
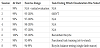
The PROMIS Global-10 is a 10-item survey that assesses quality of life measures and can be divided into physical and mental health subscales [11]. The patient improved her physical T-score by 17.90 and her mental T-score by 9.80. Existing evidence has identified a minimal clinically important difference to be 1 standard deviation from the mean - or a T-score of 10 points [14]. Her detailed scoring is displayed in Table 3.
The patient demonstrated a predictable heart rate response over the course of the program. Although she demonstrated hypertensive blood pressure readings, she was within acceptable measurements for exercise and did not demonstrate any abnormal responses. Her oxygen saturation measurements remained within 97-100% with inconsistent decreases to 92-94% (not associated with specific heart rate increases) on 4 occasions. During each of these 4 instances, her oxygen saturation recovered back above 95% and within 3% of her resting level within 1-2 minutes of occurrence. The recorded values for the patient’s vital signs can be found in Table 4-6.
The patient reported being at 95% of her full capacity at the reevaluation. She described fatigue with prolonged activity to be her main limiting factor. However, she also stated that she initiated a home exercise program with regular walking, felt more energetic, and could participate in all of her ADLs. She also transitioned from the use of a front-wheeled walker to walking unassisted at all times.
4. Discussion
We described a patient who experienced long-term symptoms from COVID-19 and persistent functional deficits, all of which is consistent with “long COVID” [3,4] . As more individuals report these signs and symptoms, utilizing some of the methods in this study may assist providers in helping patients return to their premorbid level of function after COVID-19 survival.
The patient in this study demonstrated either quantitative or qualitative improvements in each outcome measure. Interestingly, she demonstrated near clinically meaningful improvements in the mental T-score on the PROMIS Global-10 despite a primarily physically focused program. This is consistent with other findings that shortduration cardiovascular exercise programs (e.g. 6 weeks) can result in significant benefit to psychological measures such as depression [15].
Although the patient did not improve her 5 times sit-to-stand score, allowing her to push from her legs at re-test could have provided a more accurate comparison to her baseline. Her ability to stand without upper extremity assistance after requiring it at baseline does represent a functionally useful improvement in lower extremity strength. This conclusion is strengthened with the improvement in MMT scores. Similarly, although the patient did not exhibit meaningful change for single-limb balance, her ability to perform the test 5 weeks after being unable to indicates improved balance. Furthermore, she had demonstrated higher scores when performing the task during treatment sessions and reported feeling more fatigued due to sleeping less the previous night. This may suggest that she underperformed at the final session.
We also cannot draw significant conclusions from the cardiovascular response. One contributing factor may be a lack of standardization of measuring vitals and documenting the measurements. For example, there was no measured resting time at the start of the session prior to taking blood pressure. Regarding oxygen saturation changes, the patient’s response to exercise was inconsistent and cannot guide our conclusions. Furthermore, COVID-19 results in restrictive pulmonary deficits[16] and cannot be reliably compared to existing literature on oxygenation during exercise that has focused on obstructive disease. Finally, some variables (such as peak) that may change following a relatively short duration exercise program [15] could not be feasibly measured during this program. Nevertheless, her improvement with the 6MWT and transition to walking unassisted indicates that she was able to improve her aerobic endurance and gait efficiency.
Although the patient did still demonstrate some functional deficits by the final session, she reported significant improvements and wanted to discharge from the program. She demonstrated an appropriate understanding of recognizing when to stop exercise and how to continue to progress her function. This, along with her subjective and objective improvements, contributed to the physical therapists’ decision that the patient could safely discharge from the program.
5. Conclusions
Limitations of this study include that this study is retrospective with only one patient and should therefore be interpreted with caution. Randomization and comparison with a control was not possible. It is therefore difficult to exclude the possibility that the patient may have improved over time without any intervention. Furthermore, the inability to perform blind data collection and interventions introduces the possibility of bias in the results. Based on the single-limb balance score, we also must consider that the patient underperformed during the final data collection, inhibiting the conclusion of even more significant improvements. Finally, we could not objectively quantify her function prior to contraction of COVID-19, so we cannot state how close she is to her prior baseline. Additional evidence with a greater number of subjects and with a control group is required to form stronger conclusions about the benefits of physical therapy interventions in COVID-19 survivors.
There is growing evidence to suggest that additional care may be needed for some patients affected by COVID-19 [3,4] . To our knowledge, this is one of the first studies describing a short duration outpatient physical therapy program specifically designed to improve the function of a patient after COVID-19 survival. The results of this study suggest that addressing aerobic exercise, gait, lower extremity strength, functional task training, and balance can improve functional outcomes and ADL participation in an individual affected by COVID-19. The interventions may also lead to diminished likelihood of further complications such as reduced risk of falling.
Competing Interests
The authors declare that they have no competing interests.
Author Contributions
Roshan N. Devarakonda: The substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data, involvement in drafting the manuscript or revising it critically for important intellectual content, and final approval of the version to be published.
Andrew Piraino: Involvement in analysis and interpretation of data, involvement in drafting the manuscript or revising it critically for important intellectual content, and final approval of the version to be published.
Acknowledgments
The authors thank MelissaB. LaMond, PT, DPT, who assisted with treatment design and data collection of this study. They also thank Brad Ciccolella, PT, DPT and Alan Evans, PT, DPT for reviewing the paper and providing feedback on the content. Finally, they acknowledge the organization of Select Physical Therapy for facility use and management and for development of a Recovery and Reconditioning program designed specifically for individuals after COVID-19 recovery.