1. Introduction
The rupture of the ACL is often traumatic and will cause a disturbance in the stability of the knee, highly requested articulation during the activities of the daily life and during the sport practice. In 2012, 41,000 surgeries were performed in France, mainly affecting young sporting adults and more particularly women [1], therefore making the rupture of the ACL, the most frequent sports pathology [2]. In 2011, a poll found that 26.7% to 43.2% of injuries take place in football and 13.2% to 17.4% during winter sports [3].
Following a rupture, it is recommended to perform a surgical treatment with the objective of restoring the bundles in order to restore the function of the knee by minimizing the symptoms and the risk of complications [4]. The most performed surgery in the world is that of the Gracilis and Semi tendinous graft also called STG [5,6].
87% of ACL surgery are uncomplicated [7] but it is possible to find joint, muscle, neuromuscular or proprioceptive ... These changes will have an impact in the regulation of bipodal posture [8,9-11] and unipodal [12-20] statically and / or dynamically. The sports recovery is generally done around six months postoperatively through subjective criteria (answers to questionnaires, absence of feeling of instability) and unspecific [21]. Today, 75.3% of people who have had surgery return to sport at the same level as before the injury and a certain percentage did not recover after one year due to lack of confidence, fear of recidivism, or by a feeling of instability [22].
Nowadays, life expectancy continues to increase. The scientific literature agrees that physiological aging is associated with impaired postural control, caused by impairment of the various balanceregulating systems, with an increase in potentially deleterious falls in 50% to 60% [23] cases in this population with a state of "fragility" [24,25]. These consequences are one of the main causes of the reduction of activities of daily living and the quality of life of the elderly [23]. Stabilometric assessment is the study of pressure center displacement (COP) [26] on a force platform by means of static and / or dynamic measurements. This evaluation and its follow-up seem necessary and represent a certain social and economic stake to allow to refine the reeducation with the objective of resuming a sport activity identical to the previous stage in the subjects having benefited from an ACL surgery but also among the aging people in preventing the risk of falls.
However, the use of such material is not common practice and would require a large database of healthy patients to best analyze patient outcomes [27]. The literature has shown the existence of postural disorders after ACL surgery with STG and physiological aging.
This study aims to compare this disorder, of different origin, present in these two types of population, and determine if they are assimilated through the use of a platform of force.
2. Materials and Method
The study was conducted between July 2018 and November 2018. It was submitted to the ethics committee of the center which validated it.
The participants are informed of the progress of the measures through an explanatory document acting as informed consent after signature. The data obtained during the study are anonymous. No feedback on the data and protocol was made to the subjects.
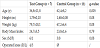
Two groups of subjects participated in the study; a first of eleven asymptomatic subjects presenting no involvement in the lower limb and a second of seven subjects who had undergone ACL surgery with STG after isolated rupture of the ACL at three months postoperatively. The characteristics of each group are presented in Table 1.
To integrate the study, the subjects of the test group had to meet the following inclusion criteria: having benefited from ACL surgery with STG after isolated rupture [8,14], be at least 15 years old, understand French, be at three months post-operative at the time of the assessment and maintain unipodal support eyes open and closed for at least ten seconds. Men and women are included in this study. Older subjects should have a BMI less than 35 kg / m2 and be able to perform unipodal support for at least 10 seconds. In order to have objective, analyzable and comparable results, the following exclusion criteria are added for the selection of the two populations: presenting central or peripheral neurological pathologies [11,12,16,17], cerebellar or vestibular disorders [16], acute dental disorders, visual uncorrected [16] (heterophobia, strabismus, amblyopia) but also otorhinolaryngology disorders, presenting a traumatic history of sprained or ligament rupture in both lower limbs during the last six months [14-17], presenting cognitive disorders [11]. The use of drugs or alcohol, 24 hours before the start of the acquisition of the measures, excluded the patients of the study [16].
An AMTI AccuGait® force platform (Advanced Mechanical Technology Inc., Watertown, MA, USA) associated with the software BalanceClinic® (version 1.4.2) was used in this study.
Prior to data acquisition, subjects were asked to hold bipodal support for 50 seconds and then unipodal for 10 seconds. Failure in one or both tests excludes subjects in the study.
A personalized support database has been created for each subject before the acquisition of the data and will be kept for the realization of the different tests.
Each participant performed four tests, in agreement with the literature data evaluating static postural balance on stabilometry platform. The protocol includes two bipodal tests (50 seconds) and two unipodal tests (10 seconds) performed with open eyes and eyes closed, knee extension. The order of performing the tests was randomized for each subject.
During tests, patients stand, barefoot, arms along the body, looking horizontally [16-18,20]. During the unipodal tests, no positions were imposed on the subjects for the non-wearing limb. Visual and auditory stimuli have been reduced to avoid distracting the patient. Three attempts are granted for each of the tests. In the third unsuccessful attempt, the test is considered impracticable.
The measures taken are the COP displacement amplitude along the medio - lateral axis (Xamp) [12,13,16,17] and along the anteroposterior axis (Yamp) [12-14,17], the displacement surface of the COP containing 95% of the recorded points (Ellipse 95) [8,12], the variation of the length traveled by the center of pressure (PathLengh) [8,12,13,16,19] as well as the average speed of displacement of the COP (Vmoy) [8,11,13,14,16].
2.1 Statistical analysis
Statistical analyzes were performed on R® software (R Development Core Team 2011, Bell Laboratories, Murray Hill, NJ, USA) after exporting the data to Excel®. The confidence level is predefined such that C = 95% and the level of significance is α = 0.05. Since the number of participants in the study is less than 15 in the test and control group, it is accepted that the values obtained do not follow a normal distribution. Mann-Whitney tests were performed to allow comparison of the results obtained.
3. Results
The age and test groups did not show a statistically significant difference for the height, weight, body mass index and sex variables (p-value >0.05). For the age variable, both groups have a statistically significant difference (p-value <0.05). An absence of a statistically significant difference (p-value >0.05) is found between the two populations for all the variables studied when during the bipodal tests. A statistically significant absence of difference (p-value >0.05) is found when comparing the two lower limbs in the control population. Randomly, it was decided to compare unipodal support on the injured side to the unipodal right support of the elderly group and to compare the unipodal support on the healthy side of the ACL group to the left unipodal support of the elderly group . Statistical analysis revealed a statistically significant difference (p-value >0.05) for all the variables studied when comparing unipodal support on the injured side of the ACL group and the right side of the elderly group. Significant p-values (p-value <0.05) are found for the variables Xamp, Yamp, and Area 95 during the comparison between the healthy side of the ACL group and the left side of the old group.
4. Discussion
Static postural balance and its study tend to develop today with the appearance and improvement of new tools such as force platforms. The purpose of the study was to compare the postural alteration present after ACL surgery with STG at 3 months postoperatively to that caused by physiological aging. The objective of this study is therefore not to evaluate the quality of the ACL surgery with STG on the postural parameter but to allow the reeducators to acquire information on the possible postural imbalances present after surgery and to be able to compare them with another population also presenting balance disorders.
This study used a customized support base compared to selected studies that use a standardized support base. In their study, Mouzat et al. [28] demonstrated that the increase in the spacing of the opening angle of the feet is correlated with an improvement of the static equilibrium. The use of a personalized support base is therefore sensible to allow subjects to place themselves in a position where they feel stable rather than constrain them in a potentially unbalanced position. The results obtained will focus more precisely on the personal and functional characteristics of each individual.
This study is the only one to compare the postural balance after ACL surgery with STG to a healthy and elderly population.
Numerous studies have investigated the quantification of postural disorders following ACL surgery compared to an asymptomatic population. The results are not identical because of the difference in the postoperative time of the subjects included.
Dauty et al. [12] studied postural disorders after ACL reconstruction, 15 days postoperatively. The results of the bipodal tests, knees extended or flexed, show a significant increase in the displacement of the center of pressure in the group having benefited from an ACL surgery compared to the control group. In unipodal opened eyes and knee extension, the study revealed a significant difference in Area95 measurement and complete COP displacement between the two lower limbs of the ACL population (both injured and healthy side) and those in the healthy population. The failure rate in closed eyes and knee flexion tests makes it difficult to analyze the results correctly. This study shows an increase in bipodal test results. Failure in some of the unipodal tests demonstrates the difficulty of performing this test and may imply a unipodal postural disorder.
Parus et al. in 2015 [9] highlighted in their study the presence of postural disorders in bipodal and tandem position at 2 months postoperatively, which is in agreement with the Dauty study. However, this disorder is no longer found at 1 year post-operative according to Sugimoto [19], at 3 years post-operative according to Henriksson [20] and at 5 years post-operative according to Lysholm [18].
The analysis of unipodal tests agree that following ACL surgery, a postural disorder is found on the injured leg but also on the healthy leg up to 2 years postoperatively [17,19,29,30] or up to 5 years according to the studies [17].
Howells et al. [13] published a systematic review in 2011 to evaluate the influence of ACL surgery on postural balance. Four studies have shown interest in postural bipodal disorders. Two studies have evaluated this disorder statically and none of them is in favor of a postural bipodal disorder at one and a half years and three years postoperatively. Also in this same review, six articles agree to put forward a unipodal postural imbalance during tests performed.
Postural alteration following ACL surgery may be primarily related to proprioceptive system involvement as well as the muscular system resulting in increased COP displacement during postural testing.
Kosy et al. [31] published a systematic review in 2017 in order to make an inventory in the field of proprioception in relation to the rupture of the ACL and its repair. Schulz and his collaborators are the first to highlight the presence of mechanoreceptors in the ACL in 1986. These mechanoreceptors form a real network up to the central nervous system in order to transmit proprioceptive. The ACL injury will result in a decrease in the number of mechanoreceptors correlated with the attenuation of proprioception accuracy.
The purpose of the surgery is to tend to recover this proprioception by replacing the native ACL by a graft that does not have the same mechanoreceptors. The phenomenon of ligamentization is a long process extending up to 1 year when it is estimated that at 6 months the neo-ligament seems identical to an ACL [31].
The role of the ACL, in the function of the knee and more particularly in its proprioception thanks to the many mechanoreceptors it contains, is certain. Its lesion will necessarily lead to a proprioceptive disorder that can be translated with postural consequences. Surgical treatment is therefore intended to improve proprioceptive recovery but it is a process that can last several months.
The scientific literature agrees that rupture of the ACL will lead to a decrease in strength that can be found preoperatively but also postoperatively. Kim and colleagues [32] published a meta-analysis in 2011 to evaluate the impact of ACL rupture on thigh muscle strength. Thus, a decrease in quadriceps strength averaged 22.3 N compared to the opposite side and a decrease of approximately 7.4 N in the strength of knee flexors. The decrease in strength of the knee extensor can be likened to a protective mechanism to prevent excessive translation of the tibia relative to the femur following rupture of the ACL and which could cause some instability. The lower attenuation of the hamstring muscle strength is not surprising, however, as they have a protective role at the knee by limiting the anterior drawer.
The degradation of the muscular system is probably associated with a decrease in the mobility of the subject then leading to a loss of muscle capacity. In their study, Thomas et al [34] highlight the effectiveness of rehabilitation for one year in improving the strength of the extensor and adductor muscles of the hip, plantar flexor muscles. However this reeducation is not sufficient for the quadriceps and the IJs because a significant difference is always present between the injured side and the healthy side after reeducation. The lack of strength of all these muscles can be at the origin of instability related to an active defect of stability and it is therefore necessary to be able to offer a rehabilitation adapted to overcome this weakness.
Studies have evaluated the strength deficit after ACL surgery and after rehabilitation. In his study, Lautamies et al. [33] evaluated the effects of surgery with STG or KJ at 5 years postoperatively. In the case of both operations, there is a decrease in strength at the level of the injured side compared to the healthy side that can influence the ability to jump and therefore the sport. This imbalance between the 2 lower limbs could then lead to the appearance of possible other lesions [35].
The state of "fragility" caused by aging has consequences for systems allowing the regulation of postural balance. The main consequence of this disorder is the fall. Its origin can be multiple but the deterioration of the postural balance is a major cause. Thus, the scientific literature has focused on the study of this disorder.
In their study Masui et al [23] put forward a significant increase in Area95 values as well as the speed of COP displacement for all age groups (55-64, 65-69, 70-74 and 75-84), for men and women in opened eyes and closed eyes bipodal tests. This increase is correlated with the age parameter.
Bird et al. [32] evaluated the evolution of postural balance, muscle strength and falls in three years in an elderly population. The results of this study show a significant increase in the COP displacement along the medio-lateral axis in static, opened eyes and closed eyesand with the presence or absence of a foam. Moreover, a degradation of the physical and functional capacities of the subjects is to be pointed out. The study did not show any significant results on the muscle strength factor in three years, but King et al [24] noted a decrease in maximum isometric strength for the upper and lower limb following a comparison between an elderly and a young population. The alteration of the postural parameters is also confirmed by da Silva et al [25]. All of these factors (strength deficit, postural disorders, physical and functional capacity deficit) then lead to a significant increase in the number of falls as well as the number of fallers in the Bird et al study [32].
Postural alteration in the elderly is caused by a set of microscopic processes that will have macroscopic repercussions impacting all the systems governing the posture system.
During aging, muscle function will undergo structural and functional changes [36,37] These changes are responsible for a decrease of 18% to 27% in muscle mass [37] resulting in a loss of strength [36,37], a decrease in endurance capacity [36] and generally associated with an increase in reaction time and a decrease in the rate of contraction [36,37]. All of its alterations are involved in the process of frailty of the elderly and will result in a decrease in the physical capacities of the elderly person associated with an impairment of his functional abilities [36,37].
The sensory system also undergoes involutions during aging that are visually reflected by a decrease in contrast sensitivity, accommodation capacity, and / or acuity degradation [38,39]. The elderly person will then have difficulty in perceiving the textures, the shapes and the colors of the objects but also the orientation and the speed of the movements [28].
Regarding the proprioceptive system, all receptors undergo a change with age. Morphological changes in neuromuscular spindles and Golgi tendon organs will result in a decrease in the statesthetic and kinesthetic capacities of the subjects, with repercussions on the functional and equilibrium capacities of the elderly subjects [40].
The postural alteration found in the two populations studied is certain but of distinct origin. In the population with ACL surgery, the postural disorder is caused by the association of a proprioceptive and muscular deficiency whereas in the elderly population this deficit is related to a progressive cellular aging which will have repercussions on the systems governing the postural balance.
Comparing the results and data from the literature, it appears that the alteration found during the unipodal support on the injured side of the population having benefited from ACL surgery with STG is similar to that related to the physiological aging during unipodal support right side. The large Vmoy in both populations shows the additional energy cost to maintain their balance with an increase in COP displacement in the different plans. Postural alteration following ligamentoplasty affects the injured side as well as the healthy side [16-18]. The comparison of the two populations shows a significant difference for Xamp (p-value = 0.01), Yamp (p-value = 0.04) and Area95 (p-value = 0.02). The lack of significant difference for the PathLengh value does not seem to agree with the previous results. The oscillations, related to the postural alteration, present on the healthy side of the ACL group are therefore lower than those related to aging with no significant difference for Vmoy.
The comparison of bipodal tests does not show a significant result. However, the literature asserts the presence of a postural imbalance linked to aging when comparing a young and elderly population. Thus, we can therefore compare the postural balance after ligamentoplasty to that related to aging and therefore affirm that there is a postural disorder in the ACL population which is in agreement with the study of Dauty et al. and Parus et al.
We can then make two hypotheses within the ACL group following the unipodal analyzes, ie the subject tries to compensate by transferring his support to his healthy side, but this would not be enough to improve his postural balance or the patient does not compensate. The answer to these two hypotheses could be allowed thanks to the study of the distribution of supports in bipodal which was not realized in the present study.
5. Limitations
However, this study has limitations that can influence the results obtained and therefore the conclusions that follow.
It is important to report the small number of participants within each group that can influence the significance of the results obtained. We cannot claim that the results of the study are representative for a larger sample.
Isolated rupture of the ACL is a rare lesion [4] and is generally associated with cartilage and / or meniscal involvement. The addition of a population with surgery to repair these lesions would then allow a more representative analysis of the population with ACL rupture.
The position chosen for the bipodal and unipodal flexion tests during the study is 20°. This position has been described by various authors during their work [12,14,17,29,30]. The completion of the 20° flexion tests, in the scientific literature and in this study, is based on the position of the Lachman test. In order to evaluate postural disorders accurately after surgery after ACL rupture, it would be interesting to position the subject in a position where this ligament would be in maximum tension and therefore where it plays its main action in the stability of the knee.
During this study, no rest time was proposed to the subjects between the different tests and a single measurement was recorded during the acquisition of the data. The majority of studies evaluating postural disorders after ligament reconstruction include a rest period of between 20-30 seconds [7,10] up to several minutes [12,14,18,20,17,30]. The common goal of this rest period is to prevent fatigue that could affect the quality of the results [16,18]. Pinsault et al. [41], in 2009, determined that the achievement of 3 measurements for each postural bipodal test made it possible to obtain excellent reliability for the results obtained. As for Da Silva and his collaborators [25], the reliability obtained after 3 unipodal tests seems correct.
In order to improve the quality of the results, it would be advisable to integrate during a future study a rest period of 30 seconds between each test in a sitting position [41] associated with a measurement of 3 measurements for each test to obtain a good reliability of the results.
6. Conclusion
The analysis of bipodal and unipodal test results highlights major results. The postural alteration found in unipodal support on the injured side for the ACL group is similar to that of an elderly population whereas for unipodal support on the healthy side the postural alteration appears lower. A lack of significant differences is found in the analysis of bipodal tests between the two populations that may indicate an absence or insufficient compensation by the ACL group during these tests.
The integration of a postural assessment associated with a muscular evaluation, of the walk and the laxity of the transplant at different stages of the reeducation would make it possible to adapt it for a fast sports recovery and to avoid the appearance of complications but also to evaluate its effectiveness in post-surgery management.
The ACL lesion is mainly found in athletes and, in view of the growing interest in stabilometry, it would be wise to evaluate postural disorders in dynamics.
7. Ethics
The application of the research protocol has been approved by an ethics committee.
Competing Interests
The authors declare that they have no competing interests.
Abbreviations
ACL: Anterior Cruciate Ligament
BMI: Body Mass Index
COP: Center of Pressure
STG: Semitendinosus and Gracilis
graft