1. Introduction
Water exercise is extensively employed as therapeutic treatment. Experts in the rehabilitation field use aquatic therapy both for the prevention of physical modifications connected with ageing processes [1], and for the functional recovery treatment after injuries or after deterioration of the musculoskeletal system [2-5] . The effectiveness of the rehabilitative and the preventive process is enhanced by the possibility to execute, in the water environment, a movement that the patients may not able to perform in dry-land (DL) condition.
From a biomechanical point of view, there are two main reasons that explain the advantages of underwater (UW) gait: i) the hydrostatic pressure yields to a clear reduction of the weight (a larger part of the body immersed produces a larger weight reduction); ii) the water density yields to an increased resistance to the movement (a larger impact surface and body movement speed produce a larger fluid resistance to the movements).
The patient performing aquatic therapy is better weight-sustained with respect to DL condition. Thus, the movement can be performed more slowly reducing the external loads at the musculoskeletal system [6]. Furthermore, there are advantages due to the rapid thermal convection of the water at high temperature [7] and due to the smaller risk of falling [8], which gives a higher self-confidence and a lower muscular stress to the patient [9].
Comparing the kinematics of the gait performed in UW and in DL conditions, small differences regarding the ranges of motion (ROM) of hip, knee and ankle joints were found [10,11]. Previous studies showed similar gait patterns in the two environments. The explanation for the small differences seems to be associated to a reduced speed (about 40% of reduction) and to a smaller step length of the gait performed in the water [11].
The injury and the consequent reconstruction surgery of the anterior cruciate ligament (ACL) of the knee yields to an altered kinematics, kinetics and movement patterns of the lower limbs [12,13]. The time and the rehabilitation procedures following the surgery are fundamental to regain the healthy gait parameters [14]. Thus, the patients tend to develop a neuromuscular reprogramming that produces a new adaptation of the gait parameters [15], in order to avoid a new lesion and to reduce pain and instability. As far as one year after surgery, 75% of the patients exhibits asymmetric gait patterns, due mainly to a smaller knee flexion and an increased external knee extension moments during the stance phase [13]. To limit the number of these cases, aquatic therapy, although not ideal for muscular strength and power restoration, reduces the joint effusion facilitating and speeding up the beginning of therapy, and yields to a larger functional awareness of the movement.
However, there is a lack of information regarding quantitative and objective data on the beneficial effects of the aquatic therapy on the joint kinematics of ACL injured patients. Thus, aim of the present study was to propose a movement analysis methodology based on inertial and magnetic sensors to provide quantitative data on the joint kinematics of an ACL injured patient, in DL and UW walking.
2. Case Study
The participant of the test (171 cm height, 85 Kg mass) had a complete tear of his left ACL occurred at the end of the landing phase of a volleyball block, during a recreational match. The injury occurred because of an unnatural external rotation of the left knee, while the left foot was motionless and in contact with the ground. Among all the knee ligaments, tendons, and cartilages, only the ACL was injured. Just after the injury the perceived pain was classified of level 6 in a range of 1-10, and the patient was treated with ice therapy, elevation, and rest. The day after the injury the patient could not walk independently, but only with the support of crutches and without putting load on the left limb. Before the surgery, the ACL knee could reach a maximum flexion of about 20°, though the extension was not compromised. Twenty eight days after the injury the patient had a reconstructive successful surgery of the ACL left knee. A graft was harvested from the patient hamstring tendons and was inserted into femoral bone tunnels to replicate his native ACL. The session test was then performed 45 days after the surgery.
3. Materials & Methods
The Outwalk protocol [16] was used to analyze the participant gait kinematics since the Outwalk accuracy is comparable to that of optoelectronic systems when using inertial and magnetic sensors. In addition, the protocol has the advantages to allow a fast set-up and to require only 3 comfortable calibration tasks. More in details, the Outwalk protocol modeled the body as an open kinematic chain constituted by 8 rigid segments (thorax, pelvis, both thighs, both shanks, both feet) and 7 joints. The thorax-pelvis, the hip and the ankle joints were considered as ball-and-socket, whereas the knee was considered as a ‘loose’ double-hinge joint. As a consequence, the joint kinematics of the lower limbs was described by 21 degrees of freedom (thorax-pelvis posterior-anterior tilting, right drop-rise, and right internal-external rotation; hips and knees flexion-extension, abduction-adduction, and internal-external rotation; ankles dorsiplantar flexion, inversion-eversion, and internal-external rotation). The joint angles were computed from the relative kinematics of adjacent anatomical reference systems computed as defined by the Outwalk protocol, using appropriate Euler sequences. The definition of the anatomical reference systems required three calibration tasks. A 20 seconds static calibration task must be performed with the participant standing in the upright anatomical posture. In the two functional calibration tasks (one per side) the subject must perform 5 knee flexion-extension cycles. If a participant is not able to flex-extend a knee actively, the calibration can be performed either through passive flexion-extensions of the knee, and through a static calibration trial with the subject lying on an examination table [16].
The participant of the test performed one static calibration task, and a functional calibration task for the healthy knee, executing 5 flexionextension cycles actively. The functional calibration task of the injured knee was performed executing 5 flexion-extension cycles passively, in order to prevent any patient pain and execute the movement correctly. After the data collection of the calibration tasks, three 10-meters-long walking trials in DL condition were acquired. The data collection of three 10-meters-long walking trials in UW condition was performed once the subject adapted to the shallow water of the swimming pool. None suggestion on the speed or technique was provided to the participant during the walking tasks, to avoid any modification of his gait patterns.
To perform the data collection, eight wearable inertial and magnetic sensors composed by a 3D accelerometer, a 3D gyroscope and a 3D magnetometer (Opal, APDM Inc., 128 Hz, Motion Studio software) were used. Specifically, the sensors were inserted in round plastic waterproofed boxes, and fixed onto the patient thorax, thighs, shanks, and feet, following the recommendations described in Cutti et al. [16] and in Fantozzi et al. [11].
The data processing was performed using Matlab® (The MathworksTM, USA), computing the lower limbs 3D joints angles, and obtaining segmented gait cycles. The gait cycles were automatically recognized and segmented using the algorithm proposed by Aminian [17], that was slightly modified in its parameters to be applied to the trials performed UW. A total amount of 50 cycles for the DL trials and 50 for the UW trials were considered. The data analysis was then completed computing angular and spatio-temporal parameters, their means and standard deviations. As angular variables, the flexion – extension ROM of hip, knees and ankles were calculated first. Then, specifically for the knees, the flexion – extension values were analyzed at the maximum, at the heel-strike and the toe-off. As spatio-temporal parameters, walking speeds (cm/s), stride times and stride lengths (s and cm, respectively), and stance percentages (with respect to the whole gait cycle) were computed, too.
As gait patterns of reference, data relative to a control group (CG) composed by eleven healthy subjects was chosen and used [11] for both the environmental conditions.
4. Results
The gait kinematics of an ACL injured patient was analyzed both in the DL and UW conditions using inertial and magnetic sensors and applying the Outwalk protocol.
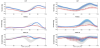
An overall graphical analysis of figure 1a suggests that, in the DL condition, the gait patterns of the patient were different from those of the CG [11]. The patient mean stride duration was longer than that of the CG (1.57 s and 1.11 s, respectively). Similarly, the patient stance phase duration (expressed as percentage of the gait cycle) was larger than that of the CG (68% and 58%, respectively). These values were observed both for the injured and the controlateral limbs. The main differences between the patient and the CG were found in both knees kinematics. The flexion-extension ROM for the injured knee of the patient was halved with respect to that of the CG, assuming a mean value of 36° and a mean maximum value of 30°. Contrarily, the ROM for the controlateral knee increased with respect to the CG up to 72°. Looking at the ankle dorsi-plantar flexion, the ROM for the injured and controlateral limbs (20° and 23°, respectively) were smaller than that of the CG (30°). Interestingly, the flexion-extension peak was found for the injured and the controlateral knee at the 63% and 77% of the gait cycle, beside the 69% of that of the CG. As well as for the knee, the minimum of the ankle dorsi-plantar flexion was found at a different percentages of the gait cycle for the CG (63%), the injured (8%) and the controlateral limb (7%).
In UW condition, the gait patterns of the patient were different from those of the CG (figure 1b), as well as observed for the DL condition. The patient mean stride duration was slightly shorter than that of the CG (2.66 s and 2.75 s, respectively), and the patient mean stance phase duration was larger for both the injured and the controlateral limbs (75% and 67%, respectively) than that of the CG (60%). Looking at the knee flexion-extension, the maximum values found were 36° for the injured and 93° for the controlateral limbs, respectively. Thus the patient showed both a reduced maximum flexion and a reduced ROM of the injured knee with respect to the CG (36° with respect to 65° and 39° with respect to 60°, respectively). A reduced ROM was observed also for the ankles (18° and 28° for the injured and the controlateral limbs, respectively) with respect to the CG value (38°). The flexionextension peak was found for the injured and the controlateral knee at the 78% and the 74% of the gait cycle, close to that of the CG (at 71%). Similarly, the minimum of the ankle dorsi-plantar flexion was found reasonably close among the CG (59%), the injured (50%) and the controlateral limb (62%) table 1.
The gait patterns and parameters obtained in UW condition were compared to those obtained in DL condition. The walking speeds were reduced in UW condition with respect to DL condition (24 and 36 cm/s for the injured limb, respectively, 22 and 38 cm/s for the controlateral, respectively). Consistently, the stride durations were longer in UW (2.66 s) than in DL (1.57 s). Regarding the joint angles, the flexion of the knees increased in UW condition with respect to DL condition at the heel-strikes and the toe-offs, and in the maximum flexion values (36° and 30° for the injured limb, respectively, 93° and 63° for the controlateral, respectively). As reported in the previous paragraphs, the temporal conformity of the knees maximum flexion peaks and of the minimum ankles dorsi-plantar flexions of the patient with respect to the CG was higher in the UW condition rather than in the DL condition.
Comparing the injured side (figure 2a) with the controlateral side (figure 2b), similar values was found for mean walking speed, mean stride time, and mean stance and swing phase durations. However, flexion angle of the injured side was halved with respect to the controlateral one at the heel-strike and the toe-off, and at the peak, in both environmental conditions. As a consequence, the overall knee ROM of the injured knee was the 47% of that of the controlateral knee in UW condition, and 50% smaller than the controlateral knee in DL condition. The same trend was obtained also for the hips: in DL condition, the ROM of the injured side was about the 72% the ROM of the controlateral one, whereas in UW condition the ROM of the injured side was about the 64% the ROM of the controlateral one. When looking at the ankles, the injured limb had a smaller flexion ROM with respect to that of the controlateral one, both in UW and in DL condition.
5. Discussion
Walking in shallow water provokes significant modifications in the musculoskeletal system [7]. As demonstrated by Micheo et al. [18] aquatic therapy allows an earlier rehabilitation in injured patients before they can walk in DL condition without crutches, and it is typically used in several pathologies, such as ACL injury. Nevertheless, there is a lack of quantitative and objective data regarding the beneficial effects of the aquatic therapy in the treatment of ACL injured patients. The method proposed appear to be suitable and effective to provide quantitative data on DL and in UW gait of musculoskeletal-injured patients. This method allow to i) analyze an ACL patient while walking in UW condition using inertial and magnetic sensors, ii) compare walking trials with respect to a CG, and iii) monitor the evolution of the treatment and support decisions of the clinicians with quantitative data.
Among the results obtained in our case-study, the flexion-extension ROM reduction of the injured knee was quantified with respect to the CG in 29° in DL condition and 21° in UW condition. This phenomena suggests that walking UW increases the flexion-extension ROM of the injured limb so that the ROM is more similar to that of the CG respect to the DL walking. Since, as suggested by Wexler et al. [13], the increment of the knee flexion-extension ROM should be one of the first functionalities to be restored in an ACL patient after surgery, aquatic therapy seems to provide beneficial effect to progress in this direction. Analyzing the gait temporal phases, a more evident conformity of the knee maximum flexion and of the ankle minimum flexion was found in the UW walking with respect to DL walking, when compared to the CG. These changes are clearly highlighted in figure 1, and suggest that the joint kinematic patterns can be assumed more similar to the CG in the UW than in DL condition. As a consequence, the walking task in UW can lead the patient to reproduce a movement more similar to that of healthy subjects, more than the same walking task executed in DL condition.
6. Conclusion
In conclusion, this case study underlines that walking in UW condition can lead an ACL patient to increase the knee flexionextension ROM, and at the same time to assume gait patterns more similar to those of the CG from the temporal gait events point of view. As consequence of these results, this case-study enhanced the usability of the method described to provide quantitative gait data in both environments, and provided preliminary information that might be considered as a first reference for further investigations on ACL patients.
Competing Interests
The authors declare that they have no competing interests.
Author Contributions
Matteo Cortesi, Andrea Giovanardi, Silvia Fantozzi: The substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data, involvement in drafting the manuscript or revising it critically for important intellectual content and final approval of the version to be published.
Davide Borra: The substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data and final approval of the version to be published.
Giorgio Gatta: Involvement in drafting the manuscript or revising it critically for important intellectual content and final approval of the version to be published.