1. Introduction
Neonatal sepsis has become a global health problem due to its high morbidity and mortality [1]. Worldwide, approximately 0.6 million newborns die from sepsis each year, which accounts for 22% of neonatal deaths. This is a serious challenge for clinicians in the diagnosis of sepsis in neonates because there is no specific clinical manifestation to be considered in sepsis diagnosis [2]. At present, the indicators commonly used in the clinic are white blood cell (WBC), and C-reactive protein (CRP) levels, procalcitonin (PCT) and blood culture which play important roles in the diagnosis of neonatal infection. The accuracy of WBC counts in distinguishing between infectious diseases and non-infectious inflammatory disorders is very low [3]. Early diagnosis and treatment of neonatal infection is an important guarantee to prevent sepsis however the blood culture which is a confirmatory test for sepsis usually takes 42-72hours to obtain a result. Therefore, it is of great significance to find a new biomarker for the early diagnosis of neonatal bacterial infection and to carry out objective clinical evaluations [4].
CD64 can be used as an indicator in the early diagnosis of neonatal sepsis as it has no physiological changes and is unaffected during the perinatal period or by complications, gestational age, and its expression is similar in normal preterm infants, full-term infants, babies and adults [5].
With the development of flow cytometry, CD64 can be measured quickly and accurately. This measurement only uses a small amount of whole blood cells which avoids iatrogenic anemia. Therefore, it is convenient for the early diagnosis and treatment of neonatal infections. CD64 molecules are known as Fc-gamma receptor 1 (FcγR1), is mainly distributed on the surface of macrophages, dendritic cells and monocytes [6]. It is constitutively expressed on monocytes and macrophages; however, it is expressed at low concentration on nonactivated neutrophils but can be markedly upregulated at the onset of the sepsis process [7]. However, previous studies have produced conflicting findings regarding the sensitivity, specificity and cutoff of CD64 for the early diagnosis of neonatal infection [8].
The present work aimed to: detect the relation between CD64 and neonatal sepsis, and to compare the differences in the CD64 index and with some laboratory parameters which are WBCs, CRP, PCT, (HSS) and the conventional clinical indicators among the control and sepsis group among the control and sepsis group.
2. Patients and Methods
2.1 Technical design
A case control study was carried out in the neonatal intensive care unit and clinical pathology department at Zagazig University Hospital, during the period from January 2019 to December 2019.
2.2 Sample size
Assuming that CD64 index mean±SD in sepsis and control group was 3.5±0.66 and 9.8±0.63. So, the sample size was 30, 15 cases in each group using INFO-EPI, CI 95% and Power 80%.
2.3 Subjects
This study was conducted on 15 cases had neonatal sepsis and 15 controls considering the inclusion criteria in sepsis group (the study group) was (positive blood culture, negative blood culture who were clinically diagnosed with sepsis) and control group (15 apparently healthy subjects cross matched with age and sex) while exclusion criteria included neonatal asphyxia, neonatal respiratory distress syndrome, fetal fecal aspiration syndrome, pulmonary hemorrhage, congenital deformity, and antibiotic treatment before admission.
2.4 Methods
Upon suspicion of neonatal sepsis, all patients were subjected to the following: history talking, clinical examination, complete blood count with differential count done on peripheral blood film, quantitative measurement of the level of CRP, PCT, blood culture and Hematological sepsis score (HSS) [9]. Total score more than 3 suggestive of sepsis as shown in Table 1.
Complete blood count: were done on automated cell counter by Sysmex XS_500i device with the differential count done on Leishmania - Giemsa stained peripheral. Then, quantitative measurement of the level of C-reactive protein (CRP) using Roche Cobas c501 device, and Procalcitonin (PCT) levels were analyzed by using Roche Cobas c411 device. Both are using dedicated reagents from analyzer vendor (Roche diagnostics, Switzer land). The total volume of blood required for CBC is 1.5 ml in tube with EDTA and 1.5 ml blood for CRP and PCT in plain tube. 1 ml blood for Blood culture were systematically collected before initiation of any treatment and done on BaCT/ ALERT 3D 60. CRP levels start in raising within 6 to 8 hours during the infectious episode in neonates and peak at about 24 hours and repeating CRP at 18_24 hours.
At that time, flow cytometric detection of CD64 MFI and calculation of the CD64 index were done by using FACSCaliur Becton Dickinson, San Joe USA) CellQuest soft BD Bioscience FACSCalibur (BD; SanJose, CA). Blood samples were collected in tubes with EDTA anticoagulant. Whole blood was stained with anti-human CD64 phycoerythrin (CD64-PE; Beckman Coulter, USA). After staining, red blood cells were lysed with Erythrocyte Lysis Buffer (BD Biosciences USA) to obtain peripheral blood mononuclear cells (PBMC). PBMC stained with fluorescent antibodies were examined by flow cytometry (FACSCaliur Becton Dickinson, San Joe USA) CellQuest soft BD Bioscience FACSCalibur (BD; SanJose, CA). Plot was drawn with forward and size side scatter (FSC/SSC) and then neutrophils and lymphocytes were gated to acquire their CD64 MFI. To ensure the quality of data analysis and quantification, CD64 expression in lymphocytes was used as a negative control lymphocyte do not express CD64.CD64 index was determined by the ratio of the CD64 MFI of granulocytes to that of lymphocytes. Gating was done for 10.000 events and considered positive for cut off more than 20% of cells expressed that marker [10]. For example, Figure 1 and Figure 2.
2.4.1 Administrative considerations
Written informed consent was obtained from all participants after clear explanation of the study and the study was approved by the research ethical committee of Faculty of Medicine, Zagazig University (Institutional Research Board “IRB”). The work has been carried out in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki) for studies involving humans.
2.4.2 Statistical analysis
The collected data were tabulated and analyzed using SPSS version 24 software (SPSS Inc, Chicago, ILL Company). Categorical data were presented as number and percentages. Chi square test (X2), were used to analyze categorical variables. Quantitative data were expressed as mean ± standard deviation, median and range. Student "t" test was used to analyze normally distributed variables among 2 independent groups. Spearman’s correlation coefficient was used to assess correlation between non parametric variables. ROC curve was used to detect cutoff values with optimum sensitivity and specificity. The accepted level of significance in this work was stated at 0.05 (P <0.05 was considered significant and P value < 0.001 is highly significant (Figure 3).
3. Result
This study was conducted on 15 cases had neonatal sepsis and 15 controls considering the inclusion criteria in sepsis group (the study group) was (positive blood culture, negative blood culture who were clinically diagnosed with sepsis) and control group (15 apparently healthy subjects cross matched with age and sex) while exclusion criteria included neonatal asphyxia, neonatal respiratory distress syndrome, fetal fecal aspiration syndrome, pulmonary hemorrhage, congenital deformity, and antibiotic treatment before admission.
Upon suspicion of neonatal sepsis, all patients were subjected to the following: history talking, clinical examination, complete blood count with differential count done on peripheral blood film, quantitative measurement of the level of CRP, PCT, blood culture and Hematological sepsis score.
There was no statistically significant difference between cases and control regarding Gestational Age (weeks), Postnatal Age, Sex and mode of delivery showed in (Table 2). On examination there was no statistically significant difference between cases and control regarding Hypothermia. On examination there was statistically significant difference between cases and control regarding prolonged capillary refill rate, Hyperventilation, Tachycardia, Activity and suckling showed in (Table 2).
There was statistically significant increase in CD64 Index, CRP, PCT and Hematological sepsis score, among Cases than control showed in (Table 3). There was no statistically significant difference between cases and control regarding HB, RBCs and HCT showed in (Table 3). There was statistically significant decrease in platelets among cases than control showed in (Table 3).
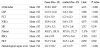
The Accuracy of CD64 in comparison with PCT, CRP, HSS and WBCs in diagnosis of neonatal sepsis showed in (Table 4).
There was statistically significant positive correlation between CD64 Index and (hypothermia, WBCs, HSS, CRP, PCT), while there were statistically significant negative correlations between CD64 Index and (Systolic Bl. pressure and RBCs), and there was no statistically significant difference between CD64 Index and other numerical data showed in (Table 5).
4. Discussion
Early diagnosis of neonatal sepsis is essential to prevent severe and life-threatening complications. However, Laboratory confirmation of neonatal sepsis is usually a problem as blood culture report takes a long time. So, we require a test which can be used for the early diagnosis of neonatal sepsis as there is also a possibility of having clinical neonatal sepsis with negative blood culture report. For the diagnosis of early onset sepsis in clinical practice, the sensitivity of any test is more important compared to the specificity, as immediate management is recommended to reduce morbidity and mortality [11].
CD64 has been identified as a high affinity Fc- gamma receptor of IgG antibody involved in the process of phagocytosis and intracellular killing of opsonized microbes [12]. Flow cytometric analysis has the advantage over conventional immunological assay methods for being able to localize the activated markers to a specific cell type. Expression of the CD64 antigen on neutrophils has been under investigation f and P value < 0.001 is highly significant or some years as a biomarker of infection and sepsis. On resting neutrophils, CD64 expression is low and after activation it is significantly up regulated within few hours. Also, in the current study cut off value for CD64 expression was calculated as 4.2 MFI with high sensitivity (96%) and specificity (86%) and its expression was high both at the time of sepsis evaluation, and at 72 hours after sepsis evaluation even though empiric antimicrobial treatment was started. Hence, this test can be used for detection of sepsis from 0 hours to 72 hours. Also, CD64 is relatively stable after blood collection and the assay is straightforward and needs only small specimen volume. Since most clinical laboratories in the developed and some developing countries have flow cytometry technology. Furthermore, standard cell counters which use flow cytometry have the potential to incorporate anti-CD64 antibodies and software to provide an even more rapid enumeration of CD64 indices nearly simultaneous with CBC results [13,14]. Currently used parameters for diagnosis of neonatal sepsis, such as CBC, CRP, PCT and, HSS were compared with CD64 expression and evaluated for their utility in diagnosis of neonatal sepsis specimen volume.
In the current study, there was no significant difference between both groups concerning age or sex. Also, there was significant increase in HSS in sepsis group than controls group which was in agreement with El-Gendy et al. [15] who reported that HSS was significantly higher in septic neonates than those with no sepsis.
Regarding, CRP was found significant increase in patients than controls which agrees with Shalaby et al. [16] and Krishnaveni et al. [17].
However, Naher et al. [18] have reported that CRP is not necessarily diagnostic for sepsis as elevations may elevate due to the physiologic rise after birth or non-infection associated conditions.
In present study showed that, there were statistically significant increase in PCT among cases than control which was in agreement with Mohsen et al. [19].
In our study, there were statistically significant increase in CD64 Index among cases than control ,and these results were in agreement with Bassuoni et al. [20] who found, there was a high statistically significant difference in mean CD64 expression levels among the studied groups (P< 0.001), and these findings are in agreement with Herra et al. [21], Tang et al. [10] and Du et al. [22] who found that the CD64 indices of the sepsis were significantly higher than those of the control group. Therefore, it provided evidence for the early and rapid diagnosis of neonatal infections and of the value of the CD64 index in clinical practice.
In our study, there were statistically significant positive correlation between CD64 Index and CRP which agrees with Tang et al. [10] and Bassuoni et al. [20].
This study showed that, there were statistically significant positive correlation between CD64 Index and WBCs and these results were in agreement with Bassuoni et al. [20] who revealed Positive correlations were found between CD64 and CRP and total leukocyte count of patients. But there were no significant correlations between Hb of the patients and CD64 expression in this study which are in agreement with those reported by Livaditi et al. [23].
In present study, CD64 Index has a valuable role in the diagnosis of neonatal sepsis. This is in agreement with Lee et al. [24] and Ng et al. [25] who showed very high sensitivity and specificity for CD64 in early-onset sepsis (about 97 and 89%, respectively); however, another study showed that sensitivity and specificity of CD64 in early-onset sepsis was 97 and 72%, respectively [13]. Also, Du et al. [22] study, who found that CD64 had the highest AUC and its sensitivity and negative predictive value was 81.82% and 75.4%, respectively.
The blood culture remains the gold standard for sepsis diagnosis, even though its result is usually delayed for more than 48 hours. Additionally, there are false-positive results due to the impossibility of excluding contamination, besides its false-negative results which are frequently encountered in the neonatal population due to small unsatisfactory blood sample volume encountered in many circumstances in neonatal intensive care units (NICUs). The antibiotics administration before blood culture withdrawal adds another diagnostic obstacle increasing its false-negative results [26].
Among other proposed markers, procalcitonin, an acute phase reactant has shown the most promise in detecting sepsis in the neonatal population [27].
We sought to evaluate the neutrophil CD64 index as a possible hematologic marker of sepsis for a variety of reasons. First, several studies have investigated the usefulness of this index in the NICU population, albeit in much smaller cohorts, but with promising results in both the preterm and term populations, as well as in cases of both EOS and LOS. Secondly, testing can be done on the same sample sent for a CBC evaluation as it requires only 50μl of blood. Thirdly, the CD64 results can be made available within hours of the CBC, since most clinical laboratories in the developed and some developing countries have flow cytometry technology. Furthermore, standard cell counters which use flow cytometry have the potential to incorporate anti-CD64 antibodies and software to provide an even more rapid enumeration of CD64 indices nearly simultaneous with CBC results [13].
5. Conclusion
CD64 index is a valuable sepsis marker. Because CD64 index is a highly sensitive marker in the diagnosis of neonatal sepsis. In addition, it has the added advantage of requiring low blood volumes which is always an advantage in neonates. However, for this test to become commercially available, we need to establish cut off values and use uniform CD64 expression parameter.
6. Recommendations
Further studies on large geographical scale and larger sample size to emphasize our conclusion.
Further studies are required involving multiple centers to establish a specific CD64 index for diagnosis and predicting clinical outcome.
Focused research is necessary to prevent and treat neonatal sepsis to improve clinical outcomes in the susceptible neonates.
Competing Interests
The authors declare that they have no competing interests.
Acknowledgments
We are grateful to clinical pathology & paediatric department teams / Faculty of Medicine, Zagazig University Hospitals. For their help and support throughout our study.