1. Introduction
Immune thrombocytopenia (ITP), an acquired hematological disorder, is due to production of auto-antibodies against platelets that leads to isolated thrombocytopenia provided other causes of thrombocytopenia such as drugs, infections, malignancy, or other autoimmune diseases are absent [1,2]. It commonly affects children between one and seven years of age[3,4]. A preceding history of infection is found in about 60% of paediatric cases [5]. The following bleeding manifestations were reported in children with ITP, cutaneous (86%), oral (19%) and nasal (20%) [3,6,7]. The diagnosis of ITP in children is one of exclusion. In patients with suspected ITP Laboratory investigations are simple and include a complete blood count and peripheral blood smear. Bone marrow examination is no longer considered necessary [8]. Management options for newly diagnosed childhood ITP include; observation only, steroids, the use of intravenous immunoglobulin (IVIG), anti-D immunoglobulin, each alone or in combination [2,5]. Splenectomy may be of benefit for children who develop chronic ITP [5]. Other useful drugs in children with chronic ITP are Rituximab and thrombopoietin receptors agonist (TPO) [9,10].
The objective of this study is to describe for the first time the demographics and clinical characteristics of Sudanese children with ITP.
2. Patients and Methods
This was an observational, case finding, hospital based; retrospective study. It was carried out at Gaafar Ibn Auf, Omdurman and Ahmed Gassim pediatric teaching hospitals involving patients who were admitted during the period from 1st of January 2007 to 30 of June 2012.
Inclusion criteria: All children with age from birth-15 year who were diagnosed as ITP .
Exclusion criteria: history of ingestion of drugs known to cause thrombocytopenia, organomegally, abnormal coagulation screening, abnormal liver enzymes and history to suggest connective tissue diseases. Data was collected by reviewing the records .The retrieved data contained demographic characteristics, clinical history, clinical examination, laboratory data, medications used and outcome. The data was displayed as figures, range, median and per centage .It was analyzed using SSPS (version 16). P value <0.05 was used to indicate statistical significance. The study was approved by the ethical committee of the concerned hospitals .Platelets count below 150x109/l defined thrombocytopenia. Thrombocytopenia present for less than six months was used to define acute ITP and thrombocytopenia present for more than six months was used to define chronic ITP.
3. Results
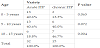
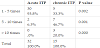
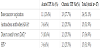
A total of 47 patients were identified, 32 (68.1%) patients with acute ITP and 15(31.9 %) patients with chronic ITP. The median age for patients with acute ITP was 6.5 years (range 0.5-14 years) and for patients with chronic ITP was 9.5 years (range 2.5-14 years). There were 17(53.1%) females children with acute ITP and 8 (53.3%) female children with chronic ITP (P= 0.989). History of febrile illness 1-2 weeks prior to presentation was common in patients with acute ITP(86.7% vs 13.3% P 0.043). The mean platelets count at presentation was ( 13.93 ± 11.74 x109/l )(range 1.0-98 x109/l) Table 1. Mean hemoglobin level was 120±38gram/L, mean leucocyte count was 6.5 ± 2.8x109/l (table 1). The Peripheral blood picture was normal in all patients. The demographic and clinical features of the study population are shown in table 1, age at presentation of patients with acute and chronic ITP is shown in table 2. The frequency of bleeding episodes in the study population is shown in Table 3. Those who had their bone marrow examined were reported to have increased megakaryocytes. Antinuclear antibodies (ANA), Direct Coomb’s Test (DAT) and HIV screening were negative in all tested children (Table 4). A family history of bleeding was present in 29.8% of patients. 14 patients (29.9%) received no treatment, 16 patients (34.0%) were treated with prednisolone, 3(6.3%) received methylprednisolone, 8 patients (7.1%)received methylprednisolone and prednisolone 2 (4.2%) had intravenous immunoglobulin (IVIG). Cyclosporine, dexamethasone and methotrexate were given to one patient (2.1%) after failure to respond to steroids and IVIG. Splenectomy was done in 2 (13.3%) patients with chronic ITP. Discussion: This is the first report on clinical profile of ITP in Sudanese children; it used the old definition and classification of the disease because that was the diagnosis given before the recent terminology. In this study patients with acute ITP were younger than those with chronic ITP, an observation similar to what had been reported before [11,12]. Males and females were equally affected ,this is similar to what had been mentioned before in many series [3,11-14]. However, in a report of 1784 children with newly diagnosed ITP males predominated [7]. A viral illness or vaccination commonly precede childhood ITP [15-17]. In this study no patient had vaccination that preceded the thrombocytopenia but one third of patients had a febrile illness 1-2 weeks before the onset of the disease . The number of patients who had an antecedent febrile illness in this study is similar to that reported from Pakistan [18] but less compared to other reports where about two third of patients had a prior viral illness [4,19,20]. The absence of history of vaccination or an infection shortly before the onset of ITP significantly correlates with a disease chronic course [21].
The cutaneous manifestations of ITP were reported to be present in almost all patients [18,22,23], our patients were not an exemption. Epistaxis was present in the majority of patients (87%). This is different from what had been reported in the literature where epistaxis occurred in 24-33% of patients [18,24,25]. Gross hematuria, considered a major hemorrhage or complication of ITP [25,26], was common in this study unlike the rare incidence (≤2.4%) reported in the literature [27-29]. Microscopic hematuria ,which was reported to occur in 27% of patients in one report [30], was not determined in this study. Hematuria was considered to be a warning sign for intracranial hemorrhage (ICH) [31]. Despite the frequent occurrence of hematuria in this study we did not encounter a single case with ICH). Hematemesis and melena were common in this study compared tothe rare occurrence (up to 2.0%) reported in the literature [27,28,31]. This high incidence of hematemesis cannot be attributed to swallowed blood since none of our patients had severe epistaxis that required intervention like nasal packing. Subconjunctival hemorrhage in ITP was not reported before in children, even in adults we encountered a single case, presented with subconjunctival hemorrhage, reported in the ophthalmology literature [32]. A family history of thrombocytopenia was reported in 2% of children [7]. In this study a family history of bleeding was noted in almost one third of patients; whether thrombocytopenia was the caused or not was not determined. The meal platelets count was 9.0X109/l. This is akin to that reported form Korea [33]. Almost two third of patients had a platelet count which was below 10.0X109/l, a count considered to predict severe bleeding [34].
The ASH 2011 evidence-based practice guidelines for immune thrombocytopenia stated that: “a bone marrow examination is no longer considered necessary at diagnosis.” Also it stated that: “We found insufficient evidence to recommend or suggest the routine use of antiplatelet, antiphospholipid, and antinuclear antibodies… etc.” [8]. In this study bone marrow examination was done in 51% of patients and the findings were consistent with the diagnosis of ITP. This rate is similar to the rate reported by Kim et al. [35]. In a study from Pakistan 64.1% has a bone marrow examination and the findings were consistent with ITP [18].
Steroids were the first line and main stay of therapy for acute ITP in this series. This result was similar to what had been reported by a survey done in south Africa in which steroids were still the first option [36]. Besides being effective steroids are cheap and this is important for a countries with low-resources like Sudan. More than one third of patients were treated conservatively, this goes with what had been recommended in the non-intervention approach [37]. Splenectomy was performed in two patients only. Kim and colleagues in a recent report had shown a high remission rate of chronic ITP in children with time. The authors suggested to delay the splenectomy for 4-5 years as long as the quality of life is not affected by the thrombocytopenia and/or therapeutic medications [35]. This suggestion might contribute in decreasing the cost associated with ITP treatment. A study had found that procedures and clinically significant bleeding were associated with higher cost when patients with ITP were hospitalized [38].
Chronic ITP was present in 31.9%, this is high compared to 23% and 18% rate reported by two studies using the same definition [39,40] but comparable to the rate reported from Qatar [41]. A systematic review and meta-analysis identified many factors as predictors of chronic ITP among them were: older age, absence of preceding upper respiratory infection or vaccination shortly before presentation, bleeding tendency, platelets count >10.0-20.0x109/L and positive ANA [42]. Older age, lack of preceding upper respiratory infection, frequent bleeding episodes and the infrequent use of IVIG were present in our study group with chronic ITP.
4. Conclusion
Sudanese children with ITP have many similarities in their clinical presentation like those reported in the literature, however they were more prone to develop major hemorrhage, subconjunctival hemorrhage and a chronic course of the disease. Implementation of more recent ITP guidelines are necessary to minimize certain laboratory tests and diagnostic procedure to help in cost reduction.
Competing Interests
The authors declare that they have no competing interests.
Author Contributions
Fathelrahman Elawad Ahmed: Contributed conception and design of the study. Also he analyzed and interpreted the data and drafted the manuscript.
Egbal Hussien Younies: Contributed in the study design, data collection, data analysis and interpretation and initial drafting of the manuscript. Both authors had approved the final draft of the manuscript.