1. Introduction
A severe behavior disorder is an umbrella term used to describe constellations of problem behaviors characterized by several factors including frequency, intensity, topography, and treatment refractory nature. Severe behavior disorders involve physical aggression (e.g. hitting, biting, choking), self-injury (e.g. head banging, head hitting, pinching, eye gouging), property destruction, and other excessive behaviors. These behaviors result in injuries to the person emitting them, injuries to others, and/or completely interfere with the person’s life. Destructive behaviors may be associated with a number of diagnoses such as autism spectrum disorder; intellectual disability; disruptive, impulse-control, and conduct disorders; bipolar and related disorders; among other diagnoses. Foxx, Zukotynski, & Williams [1] suggested that severe problem behaviors are under researched and under treated. We submit the aforementioned description remains accurate.
The effects of a severe behavior disorder are devastating. Severe self-injury can cause blindness (because of repeated head hitting or banging), deformation (because of biting, abrasions), bone fractures, hematomas, head injuries, infection (because of chronic open wounds), and death. Bergen et al. [2] found that those who presented to the emergency department with self-injury were 2 to 7.5 times more likely to die over the course of 6 years when compared to patients without self-injury. Aggressive behaviors result in harm to caregivers, law enforcement involvement, emergency hospitalization, and can be a primary factor in placing a child outside of their natural home. Aggressive behaviors may even result in death to caregivers [3]. Extreme property destruction, fecal smearing, coprophagia, and other idiosyncratic behaviors intensify treatment difficulties when combined with aggression and self-injury. Severe behaviors interfere with social development, skill acquisition, and education. Chronic severe behaviors may also lead to stress, anxiety, and other mental health problems among caregivers [4].
Severe problem behaviors require long-term residential or hospital-based treatment settings. Primary treatments include psychopharmacological interventions, function-based behavioral interventions, and various forms of restraint and protective equipment. In addition, electroconvulsive therapy (ECT) [5,6], deep brain stimulation [7], and psychosurgery [8] have been utilized.
Psychopharmacological interventions prescribed to people with severe behavior disorders include antipsychotics, antidepressants, anxiolytics, anticonvulsants, opioid antagonists, and antihypertensive agents. Psychopharmacological interventions can have some efficacy in addressing the severe behavior disorder. However, psychopharmacological interventions are often ineffective [9] and associated with negative side effects. For example, some of the side effects of antipsychotic medications include sudden cardiac death [10], neuroleptic malignant syndrome [11], tardive dyskinesia [12], weight gain [13,14] , sexual dysfunction [15], and prolactin elevation [16]. Finally, beneficial effects of antipsychotics for severe behaviors may be the result of sedation or chemical restraint [17].
A comprehensive behavioral program for a severe behavior disorder involves multiple components based on a functional assessment including combinations of the following procedures: antecedent interventions; differential reinforcement of other, alternative, and/or incompatible behaviors; extinction; satiation; punishment (excluding skin shock such as response contingent restraint or reprimands). Taken together, these interventions are often effective in reducing severe problem behaviors. However, they are not universally effective [17].
Lovaas, Schaeffer, and Simmons [18] described using skin shock as part of negative reinforcement and punishment procedures, to treat selfstimulatory and tantrum behaviors of children with autism spectrum disorder. Subsequently, skin shock has been used to treat behaviors such as dangerous climbing and aggression [19]; head hitting [20]; stomach tensions and vomiting [21]; hand to face, face slapping, eye/ tongue poking, hitting face on floor, pulling out strands of hair, skin picking, hand biting, eating inedible objects [22]; seizure induction [23]; hair pulling, attempted hair pulling, property destruction [24], biting and self-injury [25]; hand-to-head punches, head-to-object [26], among other topographies. Usually, skin shock was extremely effective in reducing the frequency of targeted problem behaviors with one exception [27]. Ricketts, Goza, and Matese [28] described instances where skin shock was initially effective but lost efficacy over time. In addition to decelerating problem behaviors, positive side effects have been noted including reductions in untreated problem behaviors, improved adaptive functioning, increased responsiveness to positive reinforcement, improved social interactions [29], higher rates of happy vocalizations [30], remission of elective mutism, improved self-care skills [25], increased smiling [31,32], less distress [33], and improved mood [34]. The primary negative side effects described include escape/avoidance responses and transient anxiety.
Although skin shock has been shown to be effective and generally associated with positive side effects [35-37], the use of skin shock has been challenged by advocacy groups resulting in what has been referred to as the “aversives controversy.” Anti-aversive advocates suggest that aversive techniques present unacceptably high risk and alternative treatments can meet the same treatment goals [38]. Additionally, some opposed to aversive interventions put forth ad hominem attacks on clinicians and families who have observed clinically significant benefit from aversives, use ad populum arguments (e.g. “The majority of the disability community opposes skin shock”), assert moral equivalence (e.g. using skin shock is the same as torture), or assert moralistic fallacies (e.g. treatment ought not to cause discomfort, aversives cause discomfort, so they cannot be beneficial). Unfortunately, such fallacious arguments are often injected into decision making processes for people with severe behavior disorders. The arguments are fueled by biased risk perception and a failure to consider the risks and benefits associated with potential treatments, against allowing the problem behaviors to continue.
Weighing benefit against risk is a commonsense way to select treatments. This process is mentioned in ethical codes [39]) and discussed by physicians who routinely use procedures that confer enormous benefit but are also associated with harm [40]. Mikklesen [41] proposed a formula that weighs the probability of success and symptom severity against the side effect profile of a psychotropic medication to aid in the decision-making process regarding psychotropic medication for people with intellectual disabilities. In addition, other fields have utilized various risk-benefit models to limit biased decision making [42].
Many of the questions associated with the controversy around aversive interventions are empirical in nature and subject to scientific inquiry. Empirical analyses can answer such questions and will provide useful information that can inform a risk-benefit analysis. Here, we summarize the effects of adding contingent skin shock (CSS), delivered through the graduated electronic decelerator (GED), to the comprehensive behavioral program of 173 individuals with severe behavior disorders. Additionally, we examine planned versus unplanned fading of treatment, reversal of treatment effects, and follow-up data spanning 15 years.
2. Method
The protocol was approved by the Massachusetts Department of Developmental Services Research Review Committee.
2.1 Participants
Of 190 individuals who received CSS treatment, 17 elected not to allow their data to be included in the study. A total of 173 (115 male and 58 female) residents, who were enrolled at the Judge Rotenberg Educational Center (JRC) in Canton, MA, participated in the study. The average age at onset of CSS treatment was 17 (range 8 - 45). Figure 1 displays the distribution of participants across the age range with most participants falling between 10 and 20 years of age. Figure 2 displays the distribution of participants across levels of intellectual functioning with over half diagnosed with no to mild intellectual disability. Figure 3 displays the number of participants associated with various diagnoses with over half diagnosed with autism spectrum disorder. Although treatment histories varied, all participants were rejected by, unsuccessfully treated in, or expelled from other settings that used a combination of behavioral interventions and psychotropic medications. Upon admission to JRC, participants were prescribed an average of 2 (range 0 - 7) psychotropic medications.
2.2 Setting
All participants were treated in JRC’s day program (i.e., school and workshop) and residential facilities (i.e., community apartments and houses). A doctoral level clinician oversaw each participant’s program. The participants’ programs in both day and residential settings were monitored directly by on-scene supervisors and remotely by supervisors who watched live and video-recorded footage across facilities. Observations were completed on a time-sampling orcontinuous basis, depending on client needs. Video cameras and microphones were mounted in appropriate locations of the school and residential halls, rooms, and exterior perimeter allowing realtime monitoring of the participant’s behavior and treatment.
2.3 Apparatus
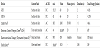
CSS was administered by the GED or GED-4. The GED device produces a current of 15 mA RMS, with a voltage of 60v when applied to a typical skin resistance of 4 kilohms. The GED-4 device produces a current of 41 mA RMS, with a voltage of 66v when applied to a typical skin resistance of 1.6 kilohms. For both devices, the electrical stimulus was a preset, 2 s train of direct current square waves with a duty cycle of 25%. The cycle consists of 3 ms of pulses at a frequency of 80 per second followed by 9 ms of no pulses. Thus, during an application, the device delivers current 25% of the time (20 pulses per second). Israel, Blenkush, von Heyn, & Rivera [43] provide complete specification forthe GED and GED-4. Table 1 summarizes and compares the electrical parameters of the GED and GED-4 with other devices.
Safeguards: The following safeguards were in effect prior to the use of CSS: (1) The parent/guardian provided written informed consent to the use of CSS that could be revoked at any time. (2) If the participant was of school age, CSS was placed in his or her Individualized Education Plan. If the participant was an adult, CSS was placed in his or her Individualized Service Plan. (3) A doctoral level clinician, with training in behavioral psychology, headed the participant’s treatment team and composed a treatment plan that included the option to employ CSS. (4) A physician and, where appropriate, a neurologist and/or cardiologist certified the absence of medical contraindications to the use of CSS. (5) A psychiatrist certified the absence of psychiatric contraindications to the use of CSS for each participant who had a mental illness diagnosis. (6) A peer-review committee, typically comprised of JRC clinicians and outside members, assessed thetreatment plan and deemed it appropriate. (7) A human rights committee, composed of JRC parents and community members unaffiliated with JRC, assessed and approved the treatment plan. (8) A Massachusetts Probate Court judge authorized the treatment plan through a "substituted judgment" petition in an individual court hearing in which the participant was represented by his or her own court-appointed attorney. (9) The court-appointed attorney retained his or her own psychologist or psychiatrist to provide advice concerning the appropriateness of the proposed treatment plan. The court-appointed attorney had the opportunity to object to any aspect of the treatment plan before and during the implementation of the plan. (10) All staff that administered CSS were trained on the relevant policies and procedures (see Procedures section) on an annual basis.
Additional safeguards were in effect after the treatment plan went into effect. Staff members who administered CSS were prompted to report any adverse effect associated with the treatment. Reports on the participant’s treatment status (including the frequency of GED applications) were submitted to the Probate Court every 3 months and the judge held a formal review each year at a minimum. If CSS was used for 3 or more years, a committee, including two independent psychologists unaffiliated with JRC, reviewed the treatment plan and its results to determine if it should continue.
2.4 Target behaviors and data collection
Two categories of behavior, aggression and health dangerous, were treated with CSS. Examples of aggressive behaviors were punch, kick, bite, head-butt, choke, and pull hair. Examples of health dangerous behaviors were hit self, bite self, head bang, choke self, pull own hair/ teeth, swallow inedible object, cut/scratch self. For some participants, the topographies treated included members of a chain of behaviors (e.g., posturing and threats) that consistently led to the ultimate behavior, attempts to engage in the behavior, and vestigial versions of the behavior. In some cases, individual topographies were added or removed from GED treatment based on individual treatment factors. Dependent on the participant’s treatment plan, other categories of behavior may have been treated with CSS including destructive (e.g., break a window or other object), noncompliant (e.g., refuse to follow a direction during an emergency), and major disruptive (e.g. scream, steal, disrobe in public) behaviors. Because participants differed in whether or not these behaviors were treated with CSS, behavior frequencies associated with these categories are not reported. However, the total frequency of GED applications, regardless of behavior category, is reported.
Behavioral observations and data collection were conducted around the clock by trained staff members. Frequency per hour was recorded by placing a tally in the appropriate cell on a recording sheet each time a client engaged in an operationally defined behavior. A charting department entered the data and conducted regular integrity checks.
Every application of CSS for targeted behaviors was recorded in a similar manner to behaviors and was verified by a second individual who was trained on relevant policies and procedures.
2.5 Design
Participants were exposed to CSS in a multiple-baseline fashion. However, displaying 173 clinical cases in a single-subject design is impractical. Instead, we present average monthly frequency data for 6 individual months pre-CSS treatment, the first partial month of treatment, 6 individual months post-CSS treatment onset, and aggregate average monthly frequency data at 1, 2, 4, 8, and 15 years. If for any reason a participant’s CSS treatment was discontinued, that participant’s data was incorporated into analyses until the point of CSS treatment discontinuation. In sum, the analysis represents the accumulation of nearly a quarter million days of objective empirical data.
A between-group visual analysis of planned versus unplanned fading of CSS treatment was conducted and a reversal (i.e., ABAB) design was utilized to display and analyze the effect of temporary removal of CSS treatment for an individual participant.
2.6 Procedure
Non-CSS: Upon admission, functional behavior assessments were completed for each participant. The functions of problem behaviors varied within and between individuals and were sometimes multiple and unknown. To account for multiple functions, all environments and staff procedures were designed to minimize inadvertent or deliberate reinforcement of problem behaviors. In particular, staff were trained to ensure that (1) positive/negative attention was minimized or avoided following problem behaviors; (2) escape/avoidance from demands was minimized; and (3) potential reinforcing tangible items or activities were not available following problem behavior. All participants were taught to gain attention, escape, and tangible items through appropriate behaviors. A data management platform enabled the participant’s clinician to review daily behavioral data for level, trend, and variability across days, weeks, and months to assess the effects of various interventions.
Treatments included antecedent manipulations, differential reinforcement of alternative (DRA), incompatible (DRI), and other (DRO) behaviors, extinction, response cost, and other procedures that, in sum, amounted to an ongoing functional analysis. Each participant had multiple overlapping DRA/DRI/DRO contracts, designed specifically for them. Speech, occupational therapy, and counseling were provided in accordance each participant’s plan of care. Psychotropic medications were eliminated or minimized.
Dangerous behaviors were contained or mitigated using approved emergency physical restraint procedures and/or health related protective equipment (e.g., helmets, arm splints, padding, etc.). In some cases, mechanical restraint (approved through a waiver or prescribed as a health-related protection) involving tethered locking cuffs or a four-point chair with a chest harness was employed to ensure the participant’s safety.
CSS: In this phase, all the behavioral procedures employed during the pre-CSS phase continued to be used and adjusted by the clinicians. However, CSS applications (GED or GED-4) were administered as soon as possible following all topographies listed under the aggression and health dangerous categories. The decision to begin with GED or GED-4 or move from GED to GED-4 was based on the individual needs of each client and approval by the probate court. The procedure for administering a CSS application required the staff member to enlist a second staff member to ensure (1) selection of the correct recording sheet for the participant, (2) the topography that occurred was listed on the recording sheet as a treatment target, (3) the consequence (i.e., CSS) was specified for said topography, (4) selection of the correct remote control for the participant, and (5) application of the CSS. These requirements introduced a short delay between the occurrence of a target behavior and the administration of the consequence but ensured treatment integrity.
Fading: We defined fading as the removal of all GED devices for any period. Fading was either planned or unplanned. Planned fading occurred by systematically removing all GED devices daily for an increasing period until the participant no longer wore devices. Unplanned fading occurred when all GED devices were removed suddenly because of some factor, most often guardian consent. Prior to planned fading, in most cases, the number of GED devices was gradually reduced until the participant reached a zero or near zero frequency of GED targeted behavior.
3. Results
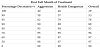
Figure 4 displays the average number of aggression and health dangerous behaviors per participant per month. During the sixmonth pre-CSS phase, aggression (M = 324, range 0-7183) and health dangerous (M = 425, range 0-23843) behaviors were observed at high, stable monthly rates. During the first partial month of CSS treatment, the monthly frequency of aggression (M = 157, range 0-3061) and health dangerous (M = 241, range 0-12805) behaviors decreased by approximately 50%. By the end of the first full month of CSS treatment, the monthly rates of aggression (M = 12, range 0-627) and health dangerous (M = 13, range 0-294) behaviors decreased by 96% and 97%, respectively, as compared to pre-CSS treatment. In the six months following the onset of CSS treatment, aggression (M = 10, range 0-990) and health dangerous (M = 12, range 0-626) behaviors were observed at low, stable monthly rates. Problem behaviors were observed at low, stable, average monthly rates at 1 year (Aggression: M = 4, range 0-112; Health Dangerous: M = 8, range 0-363), 2 years (Aggression: M = 3, range 0-69; Health Dangerous: M = 6, range 0-237), 4 years (Aggression: M = 5, range 0-917; Health Dangerous: M = 6, range 0-182), 8 years (Aggression: M = 6, range 0-172; Health Dangerous: M = 6, range 0-403), and 15 years (Aggression: M = 2, range 0-29; Health Dangerous: M = 3, range 0-37). Table 2 displays the percentage of participants that demonstrated various percentage decreases in behavior frequency during first full month of treatment.
3.1 Skin-shock applications
Figure 5 displays the average number of CSS application per participant per month. During the six-month pre-CSS phase, there were no CSS applications administered as the treatment was not in place. During the first partial month of CSS treatment, the average monthly frequency of CSS applications was 21 per participant (range 0-210). By the end of the first full month of CSS treatment, the average monthly frequency of CSS applications was 28 per participant (range 0-742). In the six months following the onset of treatment, a decreasing trend was observed in the average monthly frequency of CSS applications (M = 23, range 0-742). Across 1 year (M = 18, range 0-399), 2 years (M = 18, range 0-595), 4 years (M = 17, range 0-412), 8 years (M = 15, range 0-225), and 15 years (M = 7, range 0-105) followup, a decreasing trend was observed in average monthly rates of CSS applications. Table 3 displays the percentage of participants that received various numbers of CSS applications in the first full month of treatment.
3.2 Device fading
Figure 6 displays the average number of combined problem behaviors (i.e., aggression and health dangerous) per participant per month for planned fading (n = 23) and unplanned fading (n = 18) conditions. During the six-month pre-CSS phase, problem behaviors were observed at high, stable monthly rates in planned (M = 385, range 0-3017) and unplanned (M = 290, range 0-4215) fading conditions. During the first partial month of CSS treatment, the monthly frequency of problem behaviors decreased substantially in both planned (M = 136, range 0-1166) and unplanned (M = 120, range 0-943) fading conditions. Across the three full months of CSS treatment prior to the first unplanned fading, problem behaviors were observed at low rates with a decreasing trend in planned (M = 5, range 0-109) and unplanned (M = 5, range 0-74) fading conditions. Across the three full months prior to the first planned fading, problem behaviors were observed at low, stable rates in the planned (M = 3, range 0-41) fading condition and an increasing trend was observed in the unplanned (M = 12, range 0-213) fading condition. At 1 year (planned: M = 4, range 0-58; unplanned: M = 9, range 0-168), 2 years (planned: M = 3, range 0-98; unplanned: M = 78, range 0-2823), 4 years (planned: M = 2, range 0-130; unplanned: M = 105, range 0-2298), 8 years (planned: M = 5, range 0-435; unplanned: M = 222, range 0-4380), and 15 years (planned: M = 7, range 0-320) follow-up, fading continued in both conditions with relatively low rates of problem behaviors observed in the planned fading condition, as compared to the unplanned fading condition.
3.3 Treatment reversal
Figure 7 displays the number of aggressive and health dangerous behaviors per month for an individual participant whose behaviors received CSS treatment for three years, non-CSS treatment for nearly two years, and then returned to CSS treatment. During the six-month pre-CSS phase, aggression (M = 275, range 118-391) and health dangerous (M = 480, range 347-726) behaviors were observed at high, variable monthly rates. During the first partial month of CSS treatment, the frequency of aggression (n = 76) and health dangerous (n = 281) behaviors decreased by approximately 75% and 40%, respectively. By the end of the first full month of CSS treatment, the monthly rates of aggression (n = 5) and health dangerous (n = 83) behaviors had decreased by over 95% and 80%, respectively. In the months (n = 32) following the onset of CSS treatment, aggression (M = 1, range 0-5) and health dangerous (M = 10, range 0-83) behaviors were observed at low, stable monthly rates. A decrease in aggression and health dangerous behaviors by over 95% was observed, as compared to pre-CSS treatment. During the first three months of CSS treatment removal, a steep increasing trend was observed in aggression (M = 119, range 2-253) and health dangerous (M = 35, 28-154) behaviors. In the months (n = 22) following the removal of CSS treatment, aggression (M = 171, 2-381) and health dangerous (M = 223, range 11-592) behaviors were observed at high, variable monthly rates. In the months (n = 98) following the reintroduction of CSS treatment, aggression (M = 3, range 0-26) and health dangerous (M = 7, range 0-94) behaviors were observed at low, stable monthly rates with a downward trend in the number of CSS applications per month (M = 9, range 0-33).
4. Discussion
We summarized the effect of adding CSS to a comprehensive behavioral treatment for 173 participants with a range of diagnoses presenting with severe treatment refractory problem behaviors. In total, we reported approximately 350 years of real-world clinical data. The introduction of CSS resulted in a 97% reduction in aggressive and health dangerous behaviors after the first full month of CSS treatment, followed by continued deceleration at the molar level of data analysis. This aggregated total underestimates the efficacy for most individuals. When individual effects were classified, over half of participants demonstrated a 99% to 100% reduction in treated behaviors. These results are similar to Salvy, et al. [33], Foxx, [45]), and Linscheid, et al. [29] who demonstrated a rapid reduction in targeted behaviors in the days and weeks after the introduction of CSS. The immediate efficacy of CSS has also been summarized in previous reviews [46]. Taken together, the data presented here represents 173 replications of the durable effect of CSS on various problem behaviors, lasting 15 years for one participant. Nearly 80% of the participants received 1 or less CSS application per month while receiving treatment. The CSS treatment effect was exemplified by an analysis of individual data that included a reversal design and supports planned systematic fading when appropriate.
For 23 participants in the planned fading group, wherein CSS was systematically faded, a 99% reduction was maintained (98% across 15 years for one participant). For 18 participants in the unplanned fading group, problem behaviors accelerated after 3 months when CSS was discontinued. Various outcomes associated with CSS fading have been described in the literature. For example, Barrera, Violo, and Graver [47] and Israel et al. [34] described an immediate increase in CSS targeted behaviors upon fading. On the other hand, Fox [45] and Salvy et al. [33] described the systematic fading of CSS without a concomitant acceleration in problem behaviors. Both outcomes, deceleration and acceleration of the target behaviors, are possible and may depend on how CSS is faded. Planned fading is more likely to be successful because only cases the attending clinician believes are likely to succeed are selected for fading. In such cases, the participant likely demonstrated low rates of problem behaviors over extended periods of time, higher rates of alternative behaviors, and the acquisition of new skills. Unplanned fading is unlikely to be unsuccessful because the decision to terminate the treatment is based on other factors.
The findings indicate that for some individuals, CSS may serve as a prosthetic treatment [48]. With any treatment intervention, the goal is to eventually reduce or eliminate the treatment without a return of the problem behavior, thus “curing” the patient. However, maintaining long periods of low frequency problem behaviors is an enormous benefit. Many behavioral procedures (e.g. differential reinforcement, extinction, satiation) are prosthetic in nature. In addition, other treatments for severe behavior disorders (e.g. psychotropic medications, ECT, restraint, protective equipment) are often prosthetic. We suggest that the prosthetic nature of a treatment be viewed as a problem to solve rather than a barrier to initiating treatment. The effects of a severe behavior disorders are devastating. Treatments that are temporarily effective, yet not curative, are preferable to the continuation of treatments that have failed, are unlikely to confer benefit, or do not substantially reduce the risk of harm.
Linscheid and Reichenbach [32] described the effective use of CSS over a 4-year treatment period. Duker and Seys [49] described the use of CSS for 12 people for up to 47 months and found the procedure was effective, moderately effective, and ineffective for seven, three, and two participants, respectively. Linscheid, Hartel, and Cooley [50] described long-term suppression of up to 5 years for three participants while two others appeared to adapt to the CSS stimulus. Here, we present up to 180 months of follow-up data. In some cases, GED lost efficacy or was only partially effective and was substituted for a more intense stimulus (GED-4). This is consistent with the finding of Williams, Kirkpatrick-Sanchez, and Iwata [25], who found a more intense stimulus may be necessary to eliminate self-injurious behaviors for some individuals.
5. Limitations
The data represents a retrospective analysis of participants who received skin shock as part of their comprehensive behavioral treatment plan. The analysis lacks a high degree of experimental control. During treatment, a given participant may have received additional treatments including psychotherapy, psychopharmacology, and/or various behavioral interventions. Although voluminous, the frequency data lacks interobserver reliability. However, those collecting the data received a significant amount of training and were monitored via digital video recording to maintain treatment integrity.
The participants lacked homogeneity outside of the uniting factor of behavior problem severity and refractory nature. The participants carried a variety of diagnoses and may have responded differently because of their diagnostic classification. Additionally, the problem behaviors treated varied across individuals and were maintained by various and often multiple operant functions. There was a wide range of behavior topographies targeted that were associated with aggression and self-injury. Various pathophysiological and environmental determinants may lead to such behaviors.
Although the participants were monitored for side effects, a standardized a priori system was not employed. Anecdotally, the most common side effects observed were temporary anxiety during the period between the occurrence of the behavior and the programmed consequence as well as escape/avoidance responses. Anecdotal positive side effects were observed such as improvements in social behavior, relaxation, reduction in other untreated problem behaviors, and improved affect. These anecdotal reports are similar to what other researchers have noted historically [31,51]. Future research should be devoted to the systematic evaluation of side effects.
6. Conclusion
The results of this and other studies suggest that skin shock is rapidly effective in reducing the most intractable problem behaviors. The frequency and magnitude of the deceleration has ethical implications for treatment selection. Treatment refractory behavior disorders exist and cause severe harm to the patient, the patient’s family, and others. The existing treatments can sometimes cause iatrogenic harm and are not universally effective, yet often are accepted by the community at large. On the other hand, contingent skin shock has been shown to be routinely effective with few negative side effects, and yet is often rejected by the community at large. Thus, the current state of affairs places the needs of the general public above the treatment needs of the person emitting the behaviors, encountering the debilitating effects of their untreated condition, and experiencing the negative effects of treatments that confer minimal benefit.
Competing Interests
The authors are employed by the Judge Rotenberg Educational Center which manufactures the Graduated Electronic Decelerator (GED). The authors have not and do not receive compensation for use or sale of the GED.