1. Introduction
The increase in the experience of depression, stress, and anxiety, is reflected in many segments of the population [1]. Anxiety and stress impair quality of life among working-age populations, and impede academic achievement for university students. The percentage of students experiencing anxiety or depression-related disorders is estimated to range from 13% to 21% [2,3], while, in some samples, 31% of employees report that most work days involve stress [4]. Estimates of student anxiety and depression are high in New Zealand, with 20% of university students experiencing anxiety and 39% reporting disturbed sleep patterns due to anxiety and depression [5]. The cost to employers of mental illness is estimated to be extremely high, third only to hypertension and heart disease, according to data from a large American sample [6].
University students diagnosed with depression and anxiety achieve poorer academic outcomes compared with other students [7,8]. For employees, prolonged high-intensity stress can ultimately lead to burnout [9], which interferes with a person’s performance at work [10]. Anxiety also predicts depressive symptoms [11]; individuals who suffer from long-term anxiety may develop depression [12].
People suffering from anxiety may attempt to avoid, or escape from, anxiety-provoking thoughts and situations, which may serve to maintain the anxiety [13]. Prolonged anxiety may make it difficult for people to recover from negative emotions, resulting in the inability to regulate their moods, which exacerbates anxiety [14].
While Cognitive Behavioral Theory (CBT) has been a common treatment for a variety of psychological disorders, there is increasing interest in mindfulness-based alternatives [15]. Acceptance and Commitment Therapy (ACT) is one attempt to incorporate the concept of mindfulness into treatment [16]. Similar to CBT, the preliminary focus of ACT is to educate people to recognise negative internal events [17]. However, where CBT focuses on diminishing negative internal events, ACT promotes opening up to those negative thoughts. For instance, anxiety is negatively viewed, and, as a result, people may attempt to replace anxiety-provoking thoughts with other behaviours to create distraction, to suppress the disturbing thoughts, or to avoid situations that lead to unwanted experiences [18]. However, thought suppression is generally ineffective [18] and can actually increase the frequency and saliency of thoughts [10]. ACT, then, promotes psychological flexibility through reducing experiential avoidance; the avoidance of experiences, such as anxiety, associated with undesired personal events [18]. Fletcher and Hayes [20] describe psychological flexibility as the ability to be fully present and aware of the internal thoughts and feelings, including those that are negative, the ability to accept the experiences and avoid escaping from them, but to commit to actions that are consistent with one’s values.
Case studies, multiple-baseline treatment studies, single randomized clinical trials, and meta-analyses have provided evidence for the efficacy of ACT for a variety of problems, including anxiety and depression [21-24], stress [25-29], insomnia [30], substance abuse [31], social anxiety [32], panic disorder [22], and posttraumatic stress disorder [33].
Given that university students and employees likely face a range of issues, a transdiagnostic intervention suitable for a broad array of mental disorders would be very useful [34]. ACT could be an appropriate tool because the approach is not limited by diagnostic presentations, severity and duration of the disturbance, or demographic difference [35].
Universities often offer student health services including counselling support. However, those counselling sessions are limited as they are often understaffed or staffed by less qualified therapists [36], and students may not have time to avail themselves of these services if their study schedule is tight [3]. Moreover, many students do not seek psychological services for various reasons [2,37-40]. Similarly, an estimated two-third of Australian adults who meet the criteria for a mental disorder do not consult a mental health professional [41].
The development of smartphone applications (apps) for mental wellbeing has escalated in recent years [42]. Smartphone healthcare apps present a global, cost-effective, and convenient approach to increasing demands for mental healthcare [43]. Apps can provide programmes which positively affect those with mental health conditions, such as stress reduction [44], depression [44], and anxiety reduction [45].
Despite the rapid pace in smartphone app development and growing empirical support for their utility, few studies have specifically explored the implementation of self-help apps based on ACT within populations experiencing stress and anxiety. In the current research, we provided the ACT CompanionTM app to participants from two distinct populations; undergraduate university students and employees in various industries to examine whether the app was helpful in reducing anxiety. We used a single-subject approach where we monitored daily anxiety levels before, during, and after app use. Additionally, we administered a battery of questionnaires to assess aspects of anxiety, depression, and psychological flexibility before and after app use. We hypothesised, firstly, that scores of anxiety, stress, depression, and negative affect would decrease as a result of app use. Secondly, we predicted that participants’ mindfulness, psychological flexibility, and acceptance and wellbeing would increase following app use.
2. Method
2.1 Participants
To be eligible for inclusion in the study, participants had to have a mobile device (smartphone or android), not be undergoing psychological treatments or taking psychoactive medications, and score at or above 50 on the Daily Assessment of Symptoms-Anxiety (DAS-A). The cut-off score was set at 50 in order to enable detection of reductions in anxiety over time.
Students: One male and eight female students of psychology at the University of Waikato, labelled S1 - S9, aged between 19 and 33 years, met the inclusion criteria and completed the study.
Employees: Four male and six female people, labelled E1 - E10, aged between 25 and 60 years met the inclusion criteria and completed the study. Three were teachers or vocational or occupational consultants, two were solicitors, two were support workers, one a sales manager, one a resource planner, and one worked in information technology.
2.2 Materials
Participants were given free access to the full version of the ACTCompanion® app on their own mobile device.
2.3 Measures
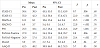
Table 1 lists the measures we used in the study. We asked participants to complete the DAS-A throughout the study to monitor the daily change in anxiety level. We used the State-Trait Anxiety Inventory for Adults (STAI), Hospital Anxiety and Depression Scale (HADS), Perceived Stress Scale-10 (PSS-10), and The Positive and Negative Affect Scales (PANAS) to measure participants’ anxiety, stress, and depression, and the Mindful Attention Awareness Scale (MAAS), and the Acceptance and Action Questionnaire (AAQ-II) to measure psychological flexibility and acceptance at pre- and post-intervention.
2.4 Design
We used a single-subject A-B design with two main phases; baseline (A) and intervention (B). For six participants, we obtained 2 - 3 days’ of DAS-A scores a minimum of 6 months after they finished using the app; Follow-up (C).
2.5 Procedure
Ethical approval for the research was given by the School of Psychology Research and Ethics Committee under delegated authority of the Human Research Ethics Committee of the University of Waikato. Potential participants contacted us in response to advertisements placed at the University of Waikato, large workplaces in the region, and on social and news media. Once they made contact, we supplied them with an information sheet and, if they were still interested in participating, we met with them either in person or via skype to explain the study and obtain informed consent. Participants who consented first completed the battery of questionnaires on Qualtrics®. We asked them to complete the DAS-A every day for a minimum of 3 days.
During the intervention phase, we gave participants access to the app and asked them to use the app as much as they wanted to, but to complete at least one activity per day. We asked them to continue to complete the DAS-A each day. While we received scores less often than daily for some participants, all participants completed the daily questionnaires regularly.
2.6 Data analysis
We analysed the data initially using single-subject graphical analysis by plotting DAS-A scores across phases. We fitted straight lines to the data from Baseline (A) and Intervention (B) phases separately using the linear regression function in Sigmaplot 12.5®. We conducted mixed Analyses of Variance (ANOVA) using IBM SPSS 25® using the slope parameters as a dependent variable and, in a separate ANOVA, scores on the pre- and post-questionnaire measures, to determine whether there was any improvement in dependent variable scores as a result of app use.
3. Results
3.1 Pre-post questionnaire results
Using the scores from each questionnaire as a dependent variable, we ran a series of mixed ANOVA with participant type (student vs. employee) as a between-subjects independent variable and administration time (pre- or post-app use) as a within-subject independent variable. Every test met the assumption of equality of error variances, according to individual Levene’s tests. The results of each ANOVA were similar. Specifically, for every measure, there was a significant effect of administration time, with post-app scores improving in every instance from pre-app scores, but no main effect of participant type, and no interaction between participant type and administration time. This means that, in every case, scores improved to a similar degree for both students and employees following app use. The statistical results for each measure are given in Table 2.
3.2 Daily anxiety scores
Daily scores on the DAS-A across phases for students consistently showed that, prior to app use, anxiety scores were increasing. During app use, anxiety scores, although variable, decreased gradually over time. Graphed results showed patterns for employees that were less clear. For two employees (E2 and E4), anxiety scores were increasing in baseline, while for three (E1, E5, and E7), they were neither trending upwards or downwards, and for the remaining five, scores were decreasing prior to app use. During app use, for some participants (E1, E2, E3, E6, E7, E8, and E10), daily anxiety scores decreased relatively steadily during app use. For others (E4, and E9), anxiety scores dropped almost immediately and then remained low and stable across the intervention phase. For E5, app use appeared to have little effect on DAS-A scores. Figure 1 shows the data for the six participants for whom we have follow-up data (S2, S5, S7, E6, E7, and E10). The data for these participants reflect patterns not dissimilar to those found for the remaining participants (not shown).
There was a significant effect of administration time (pre- and during-app use) on the slopes of straight lines fitted to daily data, MPre = .82, 95% CI[.18, 1.46], MPost = -.29, 95% CI[-.40, -.17], F(1, 17) = 14.32, p = .001, r = .67. Mean slopes were positive prior to app use, showing that daily anxiety levels were increasing on average across baseline, and mean slopes of lines fitted to daily scores during app use were negative, showing that anxiety levels were decreasing. There was also a significant effect of participant type on slope values, MEmployee = -.29, 95% CI[-.76, .19], MStudent = .82, 95% CI[.32, 1.32], F(1, 17) = 11.59, p = .003, r = .64, indicating that student slope values were overall more positive than were employee slope values. The interaction between participant type and administration time was also significant, F(1, 17) = 16.84, p = .001, r = .71. The interaction indicated that for employees, slopes changed little across administration time, but that slope values decreased for students from pre- to during-app use periods.
We calculated the mean of the last 3 days of DAS-A scores for baseline and intervention phases and used these means as dependent variable scores in a mixed ANOVA with phase (baseline vs. intervention) as a within-subject independent variable and participant type (student vs. employees) as a between-subject variable. There was a significant main effect of phase, F(1, 17) = 68.79, p< .001, r = .90, with baseline mean scores being significantly higher, M = 61.02, 95% CI[57.49, 64.56], than the mean scores recorded for the last 3 days of the intervention phase, M = 33.19, 95% CI[27.12, 39.28]. There was no main effect of participant type on mean daily DAS-A scores, F(1, 17) < 1, and no significant interaction between phase and participant type, F(1, 17) = 1.21, p = .29, r = .26. These results support those from the pre- and post-intervention measures showing that anxiety scores had decreased at the end of the intervention phase compared to those at the end of the baseline phase for both employees and students. Similar results were obtained when the mean follow-up DAS-A scores were entered into a mixed ANOVA with mean baseline DAS-A scores (results not given), showing that DAS-A scores remained low at follow-up, M = 36.42, 95% CI[26.78, 46.06] compared to at the end of baseline (mean and CIs already given).
4. Discussion
We aimed to investigate the efficacy of a smartphone app for relieving anxiety among nine university students and 10 employees. For every measure used in the questionnaire battery, scores improved significantly following app use relative to baseline levels. There was no effect of participant type, and no interaction between participant type and the time that the tests were administered, showing that app use resulted in consistent positive outcomes for both university students and employees. The tests were designed to measure a variety of constructs, including state and trait anxiety and daily anxiety, stress, depression, positive and negative effect, and psychological flexibility. As the scores of all these tests improved, we conclude that use of the ACTCompanion® can result in improvement in a number of areas of people’s lives. Similar improvements have been achieved through the use of other smartphones apps, such as an improvement in anxiety, depression, and psychological flexibility scores as a result of using the ACT Daily app [46].
Similar to the findings for the pre- and post-intervention measures, we found that daily scores of anxiety decreased significantly as a result of app use and remained low up to 9 months after the end of the study. Of the six participants who provided follow up data, only one reported that they were still using the app, suggesting that improvements engendered through app use were maintained in the absence of app use and potentially that the participants had learned to incorporate the app activities into their everyday lives.
Our finding that individual engagement with a widely available app had reliable and sustainable positive effects on people from two different populations is encouraging. As argued earlier, many people who require an psychological intervention do not receive one [2,37-41], so effective interventions that have the potential to reach large numbers of people before their problems become overwhelming are extremely valuable.
One potential limitation of our study is related to the self-reported nature of the data, and, therefore, the possibility that participants reported improvements because of expectation effects. While we acknowledge this possibility, we doubt that the positive results found here were entirely attributable to such an effect. Evidence to support our position come from the follow-up data, as participants could not be reasonably expected to have remembered the way they were answering the DAS-A up to 9 months since they last completed it. Hence, we tentatively accept the improvements reported by the participants here as accurately reflecting their experience.
We used a single-subject, non-concurrent-baseline design across multiple participants which offers many advantages over other approaches [47]. A concurrent, multiple-baseline design requires that individuals begin the baseline condition at the same time, however, using a non-concurrent design made recruiting participants more convenient as each participant could start as they were recruited. This design was practical and flexible as not all individuals were available at the same time. In addition, each individual served as their own control, reducing variability and increasing validity. As argued by Singh, Starkey, and Sargisson [48], single-subject designs “hold great promise for evaluating the outcomes of mHealth behavioural interventions” (p. 8). Particularly, removing the requirement for large sample sizes enables evaluations which are much quicker to complete - an important consideration in the rapidly evolving field of mHealth [48].
Competing Interests
The authors declare that they have no competing interests.
Ethical Approval
We gained ethical approval from the School of Psychology Research and Ethics Committee under delegated authority of the University of Waikato Human Research Ethics Committee.
Acknowledgments
We would like to thank the developers of the ACTCompanion® app, Anthony Berrick and Dr. Russ Harris, for supporting the study with free apps for our participants.
Abbreviations