1. Introduction
Surgical wound complications encompass a broad spectrum of adverse events including superficial wound separation, seroma or hematoma formation, fascial dehiscence and surgical site infection (SSI) [1]. These complications can result in unplanned hospital readmission and in some cases reoperation. Additionally, wound complications are a significant financial burden for both patients and hospitals [1-3]. Abdominal hysterectomy is one of the most commonly performed operations by both gynecologist and gynecologic oncologist. In the United State, approximately 600,000 hysterectomies are performed annually [4]. The rate of wound complication associated with this procedure ranges broadly, from 1.8 to 12.2% [5-8]. More specifically, 1-4% of all hysterectomies are complicated by SSI [9,10]. Hysterectomies performed by laparotomy carry the highest risk for post-operative wound complication, with SSI rates of up to 6.7% [9]. Additionally, obesity (BMI >30 kg/m2), diabetes and age >45-years have been associated with increased risk for the development of wound complications, including SSI [7,8].
The wound dressing is a critical, yet often overlooked, component of wound closure and therefore a key last-step in any major abdominal procedure. Moisture retention is vital to the healing process. Natural fluids within the wound contain important tissue growth factors that facilitate epithelialization and promote autolytic debridement [11,12]. The ideal wound dressing should maintain moisture and warmth to facilitate healing. Additionally, the dressing should absorb excess fluid and exudate without leakage and be impermeable to both water and bacteria [13]. While the concept appears simple, implementing these “ideal” dressing conditions in everyday practice can be exceptionally challenging. Traditional surgical dressing are often comprised of basic woven-gauze and tape dressing which are easily dislodge by minor movement, quickly soiled by excess drainage and are not changed at appropriate intervals. These factors facilitate the accumulation of debris and growth of bacteria; leading to the development of wound complications and SSI.
Recently, there has been investigation into technologies to improve traditional surgical site dressings in an attempt to decrease the incidence of wound complications and SSIs [2,3,5,6]. Noninvasive negative pressure wound therapy (NNPWT) takes the place of a traditional surgical dressing and is placed immediately following primary skin closure in the operating room. NNPWT promotes wound healing by improving cutaneous blood flow and microcirculation, protecting the incision from the environment, increasing oxygen saturation, and decreasing the incidence of seroma formation [14]. Additionally, the use of NNPWT has been found to be a cost-effective alternative to traditional wound dressing in patients considered to be a high risk of wound complication, particularly obese patients [2,5,15]. Existing literature on the efficacy of NNPWT has focused primarily on patients undergoing gastrointestinal, trauma, vascular and obstetric surgeries [15,16]. To our knowledge, there are no published studies examining the impact of NNPWT in gynecologic or gynecologic oncology patients. In the current report, we evaluate effect of NNPWT on overweight and obese patients undergoing major abdominal surgery via vertical midline laparotomy, performed by a gynecologic oncologist.
2. Methods
We conducted a multi-center retrospective review of overweight (BMI 25-29.9 kg/m2) and obese (BMI >30kg/m2) patients undergoing surgery via vertical midline laparotomy by a gynecologic oncologist from September 2012 to December 2017. Participating institutions included SUNY Downstate Medical Center – University Hospital of Brooklyn and King’s County Hospital Center. Internal review board (IRB) approval was obtained by participating institutions. Patients undergoing vertical midline laparotomy for hysterectomy, with or without bilateral salpingo-oophorectomy, staging procured (including pelvic +/- paraaortic lymphadenectomy), cytoreduction or gastrointestinal surgery were identified. Complex surgery was defined as patients undergoing lymph node dissection or cytoreductive surgery. Operative reports were reviewed to confirm the type of wound dressing applied. NNPWT was defined as the use of an occlusive, one-time use, non-invasive negative wound pressure therapy system for up to 7-days post-operatively. Traditional dressing was defined as the use of any variation of woven-gauze material with tape (silk or paper tape). Medical records were reviewed for demographic data (age, race, BMI) and post-operative outcomes, including SSI, 30-day hospital readmission and length of hospital stay (LOS). SSI was defined as either superficial or deep space wound infection requiring antibiotic therapy, with or without additional intervention (debridement, drainage or reoperation). Patients were included in the final analysis if they underwent vertical midline laparotomy by gynecologic oncologist, BMI >/= 25 kg/m2, skin was closed primarily (staples or subcutaneous suture), underwent standard antimicrobial preparation with chlorhexidine abdominally and betadine vaginally, and received routine intravenous prophylactic antibiotics as per the American College of Obstetrics and Gynecologic recommendations.
Key exclusion criteria included; patients with a BMI <25 kg/m2 and surgery performed by incision other than midline vertical incision. Additionally, patients were excluded if NNPWT was removed within the first 24-hours of placement. We compared the 30-day SSI rate, 30-day hospital readmission rates and LOS between patients receiving NNPWT versus those receiving traditional wound dressing. Additional analysis included comparison superficial and deep SSI, incidence of fascial dehiscence, superficial wound separation and superficial wound collection between treatment arms. Superficial wound collection was defined as either seroma or hematoma leading to spontaneous skin opening or requiring intervention to drain the collection. Superficial wound separation was defined as separation of the skin and exposure of the subcutaneous tissue, requiring healing by secondary intention. NNPWT became universally available at both participating institutions in September 2016, and were applied based on the surgeon’s digression. Patients receiving a traditional wound dressing prior to were designated as the pre-intervention cohort. Patients receiving NNPWT were designated as the post-intervention cohort. A one-way ANOVA test was used to compare differences in mean age, BMI and LOS between treatment arms. Differences in the frequencies of race, pre-existing comorbidities, type of surgery, surgical wound classification and outcomes variables were identified using Pearson’s chi-square test. A p-value of 0.05 was used to indicate statistical significance. Statistical analysis was performed using SPSS version 25.0 (IBM, Armonk, New York).
3. Results
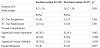
Final analysis included 192 patients; 155 (80.7%) patients received a traditional wound dressing (pre-intervention) and 37 (19.3%) received NNPWT system (post-intervention) placed immediately post-operatively. The mean BMI of the entire cohort was 32.1 kg/m2 (25.0-58.0). The mean BMI of patients receiving NNPWT system was significantly greater than that of the traditional wound dressing cohort (34.8 vs. 31.6, p<0.005). Other demographic characteristics including age and race did not differ between treatment groups. There was a non-significant trend toward a higher incidence of diabetesmellitus in the NNPWT cohort (24.3% vs. 18.7, p=0.441). The 76.8% of patients underwent laparotomy for gynecologic malignancy and 18% of patients underwent gastrointestinal resection during surgery. The majority of operations were classified as clean-contaminated based on the CDC surgical wound classification system. There was no difference in the percentage of patients with a diagnosis of cancer (p=0.572), surgical site wound classification (p=0.129) or the complexity of surgical cases between treatment cohorts (p=0.235) (Table1).
The median LOS was significantly shorter in the NNPWT cohort (5.6 days vs. 9.6 days; p=0.001). The use of NNPWT was also associated with a significant decrease in SSI at 30-days postoperatively compared to traditional wound dressing (0% vs. 9.6%; p<0.001). Compared to traditional wound dressings, patients receiving NNPWT experienced significantly less fascial dehiscence (0% vs. 3.75%; p=0.025) and superficial wound collections requiring intervention (18% vs 5.4%; p<0.001). There was no significant difference in 30-day reoperation rates, 30-day hospital readmission rates between the treatment groups (Table 2).
4. Discussion
Post-operative wound complications are a significant source of morbidity in patients undergoing laparotomy. Wound complications lead to prolonged wound care, need for antibiotics and in some cases, even surgical intervention. This contributes to longer LOS, decreased mobility and increase incidence of venous thromboembolism [17]. All culminating in increase cost to both healthcare systems and patients [18]. Decreasing the wound complication and SSI rate has been a recent focus of many societies and institutions. As a result, multiple societies, including the American College of Surgeons and the Expedited Recovery After Surgery (ERAS) society, have implemented guidelines to decrease SSIs and the associated cost [19-21]. Although these guidelines offer a multi-disciplinary approach and both pre- and post-operative guidelines, there are no specific recommendations for the type of surgical wound dressings, even in the highest risk patients.
Many factors contribute to, and increase the risk of wound complications, including advanced age, obesity, diabetes, active malignancy and peripheral vascular disease [5-8,22,23]. NNPWT help combat these facts by creating a favorable wound healing environment for up 7-days; the most critical period for initial wound healing [12]. Despite the theoretical benefit of NNPWT, there is lack of consensus in literature regarding the role of routine NNPWT. Several small retrospective studies have observed an improvement in post-operative outcomes with NNPWT, including shorter LOS and decrease wound complications in gastrointestinal, trauma and vascular surgery [24-28]. However, a recent randomized controlled trial of patients undergoing laparotomy for gastrointestinal, pancreatic and peritoneal surface malignancy failed to demonstrate any benefit to the use of NNPWT compared to traditional wound dressings [22]. These findings were recently confirmed by a large Cochrane Database review which included 30 trials and 2957 patients [15].
Gynecologic oncology patients typically represent a high-risk group of patients with multiple co-morbidities in addition to active cancer. Cancer itself is known to impair wound healing [20]. This is especially true in the case of advanced disease and poor nutritional status leading to impaired immune function and long delays in wound healing. Blackham and colleagues reviewed their experience with NNPWT in high risk surgical oncology patients. They found the use of NNPWT was associated with significantly fewer SSI and superficial wound separations [7]. The vast majority of oncology patients are >55-years of age. Pellino et al. found that advanced age alone was an independent risk factor for post-operative wound complication and observed a significant decrease in wound infections with the use of NNPWT in this patient population [8]. Importantly, the avoidance of post-operative wound complication in the oncology population also leads to faster receipt of necessary adjuvant therapy (chemotherapy and/or radiation therapy). Based on our findings, in concert with those of Pellino et al. and Blackman et al. we believe overweight and obese gynecologic oncology patients undergoing laparotomy pose significant risk for wound infection and should be managed with NNPWT when available.
Our study has several important strengths. Although this is a multicenter review, the same surgical team, consisting of attending, fellow and resident physicians, performed all surgeries at both institutions. Surgical techniques and decisions were all determined by the attending physicians, who remained constant throughout the study period; minimizing variability between patients and treatment groups. The key limitations to our study are its retrospective nature and relatively small sample size. Additionally, although the NNPWT systems were intended to remain in place for 7-days, in some instances the system was removed earlier due to malfunction or patient removal before instructed date. We are unable to account for the differences in the length of NNPWT use in all patients. Despite these limitations, this is the first report to observe improvement in outcomes with NNPWT in a cohort of patients undergoing laparotomy for gynecologic or gynecologic indications.
5. Conclusion
NNPWT significantly decreased the SSI rate and hospital LOS in overweight and obese patients undergoing major gynecologic surgery via vertical midline laparotomy. Minimizing post-operative complications is key to the delivery of prompt postoperative adjuvant therapy in gynecologic oncology patients. These findings warrant prospective confirmation as well as the evaluation of NNPWT in nonobese gynecologic surgical patients.
Competing Interests
The authors declare that they have no competing interests.
Author Contributions
Jennifer McEachron: Manuscript writing, statistical analysis
Sasha Sabir: Data collection, manuscript writing
Michelle Bennett: Data collection, manuscript writing
Lila Marshall: Data collection
Yi-Chun Lee: Study design, manuscript review
Margaux J. Kanis: Study design and conceptualization, manuscript
review, oversight of project