1. Introduction
Majority of patients with endometrial cancer present in the early stages and have a favourable prognosis. Approximately 15 % of women have extrauterine disease at initial presentation and a further 5% have extension to the bladder or bowel mucosa or distant metastases. Women who present with advanced disease have a poor prognosis and limited data exists to guide treatment [1,2].
Although there is no agreed standard treatment for patients with advanced endometrial cancer, optimal surgical cytoreduction is highly correlated with prolonged survival [3-6]. Women with stage III/IV serous endometrial cancer for example have a median survival of 9.6 to 14 months after suboptimal cytoreduction and 26.2 to 51 months after optimal cytoreduction [3,5,6]. Extensive surgery may be required in order to achieve this optimal debulking but many women at advanced age with additional comorbidities, higher disease burden and presence of extra-abdominal metastases may not be suitable surgical candidates.
Neoadjuvant chemotherapy (NACT) and delayed primary or interval debulking surgery has emerged as an alternative for patients with advanced ovarian cancer who have unresectable disease or poor performance status [7]. Whilst multicentre randomised controlled trials have compared the role and survival of patients having neoadjuvant treatment for ovarian cancer, there is a paucity of data analysing survival and surgical outcomes in patients who have received neoadjuvant chemotherapy for advanced endometrial cancer [8]. Our gynaecological cancer centre database has provided the cohort of patients who were individualised to receive NACT and the primary objective of the study was to analyse survival and surgical outcomes in women who had neoadjuvant chemotherapy followed by delayed primary surgery compared to those who had primary cytoreductive surgery.
2. Material and Methods
2.1 Study eligibility
Retrospective review of treatment records of all consecutive patients diagnosed with FIGO Stage IIIC/IV endometrial cancer between January 2010 and December 2016 was undertaken. This patient group was identified from the cancer services database. Inclusion criteria for this dual cohort, single centre study were women with FIGO (2009) stage IIIC/IV primary endometrial cancer who were discussed at the cancer centre multidisciplinary team meeting and scheduled to receive either neoadjuvant chemotherapy or undergo upfront primary cytoreductive surgery. All pure epithelial histological types were included in the study database. Patients who received palliative chemotherapy or hormones and all those with sarcomatous histology such as uterine carcinosarcomas were excluded. Women who had stage IIIA/IIIB disease were excluded as adnexal or parametrial involvement seldom constitutes an indication for Neoadjuvant treatment.
The criteria for choosing neoadjuvant treatment at the multidisciplinary meeting was radiological impression of unresectable disease, presence of extra-abdominal metastases (both parenchymal and thoracic metastases) and poor performance status. Three cycles of neoadjuvant treatment were administered prior to assessment of chemotherapeutic response with interval imaging. RECIST criteria were used to grade response to chemotherapy and regimen change was advocated if there was disease progression with first line chemotherapy [9]. Women who showed disease progression with 2nd line neoadjuvant chemotherapy did not undergo surgery and continued treatment with palliative intent. Some patients had an extended course of 4 to 6 cycles before being suitable for cytoreductive surgery. Surgical procedures performed included a total hysterectomy, bilateral salpingo-oophorectomy, pelvic and para aortic nodal dissection and omentectomy. Extended and radical surgery was undertaken to achieve R0 (nil residual disease) and included bowel resections, parametrectomy, inguinal node resection, abdominal and pelvic peritonectomy, diaphragmatic stripping and partial cystectomy.
2.2 Clinical characteristics
Clinical data on patient demographics, stage of disease, date of diagnosis, preoperative disease distribution, histological subtype and grade of tumour, comorbidities, WHO performance status, details of neoadjuvant and adjuvant chemotherapy regimens and response to chemotherapy was obtained from review of electronic patient records and radiological reports. Review of operative notes and postoperative charts facilitated data entry on date of surgery, intraoperative assessment of tumour volume, extent of surgery, intraoperative blood loss and visceral injury, residual disease status, duration of postoperative stay in days and postoperative complications such as sepsis, readmission and postoperative mortality. Duration of followup, progression-free survival, overall survival and cause of death were recorded.
2.3 Study definitions
Patients with intraparenchymal liver metastases, thoracic disease in paracardiac lymph nodes, supraclavicular lymph nodes and lung parenchyma were included in the extra-abdominal disease group. Optimal debulking was defined as residual disease equal to or less than 1 cm and no residual disease was indicated by absence of any gross visible disease. Sub-optimal cytoreduction was defined as residual disease greater than 1 cm. Progression-free survival was defined as the interval from initiation of treatment until the date of clinical or radiological recurrence or progression. Overall survival was calculated from date of initiation of treatment until death from any cause.
2.4 Statistical analysis
Demographics and surgical outcomes were described in the 2 groups using risk ratios, mean differences or median differences as appropriate. Overall survival & progression-free survival were described using Kaplan Meier survival curves. The statistical package Stata, version 14.2 (Stata Corp, College Station, Texas) was used for all statistical analysis. 95% confidence intervals and significance at p< 0.05 were used throughout.
3. Results
Database analysis revealed 1335 cases of endometrial cancer over a period of 7 years. Surgical and survival outcomes were analysed for 16 women who had neoadjuvant chemotherapy followed by delayed primary surgery for stage IIIC /IV endometrial cancer and examined alongside the outcomes of 28 patients who had primary cytoreductive surgery followed by chemotherapy in the period extending from January 2010 to December 2016.
3.1 Patient demographics and disease distribution
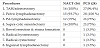
Table 1 demonstrates the patient demographic factors and disease stage in the 2 groups. Median age of the NACT group was 62.9 years and that of the primary cytoreductive surgery group was 62.4 years. There was no difference in the ethnicity distribution, incidence of all comorbidities (75% NACT vs 81% PCS) or performance status between the 2 groups. White caucasian women comprised 33 (75%) of the 44 patients in the study. Hypertension as a comorbidity was more prevalent in the PCS group and history of thromboembolic disease was more common in the NACT group. There was no significant difference in the distribution of histological variants of endometrial cancer. There was however a significant difference in stage distribution with a higher proportion of patients with stage 4 disease belonging to the NACT group.
3.2 Surgical procedures / perioperative and cytoreductive outcomes
Surgical procedures, outcomes and residual disease status are described in Table 2 and Table 3. There was no difference in the mean estimated blood loss (946.9 ml NACT vs 790ml PCS) between the 2 groups (p value 0.47). The incidence of major intraoperative blood loss and visceral complications was similar between the 2 study cohorts as were the postoperative complication rates. The mean duration of postoperative stay was 5.63 days in the neoadjuvant chemotherapy arm whilst those in the PCS group had a mean length of stay of 5.61 days. 68.8 % of patients in the NACT arm had optimal debulking in comparison to 60.7% in the PCS group. This did not reveal any significant difference in the cytoreductive status between the 2 treatment groups.
3.3 Chemotherapy and radiotherapy treatment
Patients in the NACT group (87.7%) predominantly received Carboplatin and Paclitaxel chemotherapy (Table 4). 1 patient was treated with Cisplatin and Doxorubicin and another received Carboplatin and Paclitaxel initially followed by Cisplatin and Doxorubicin chemotherapy due to a poor response to the first regimen. Of the patients who received Carboplatin and Paclitaxel, 3 patients received 3 cycles of chemotherapy, 9 patients received 4 cycles and 2 women received greater than 4 cycles to a maximum of 6 prior to surgery. 15 of the 16 patients (93.7%) in this group showed at least a partial response to chemotherapy by RECIST criteria. External beam radiotherapy (EBRT) +/- vaginal vault brachytherapy were given to 50% of women in the NACT group if there was no extra-pelvic disease following chemotherapy.
In the PCS cohort, 57.1% (16) of patients received chemotherapy following surgery with Carboplatin and Paclitaxel, 28.6 % [8] received Cisplatin and Doxorubicin and 7.1% (2) received initial Carboplatin and Paclitaxel which was then converted to Cisplatin and Doxorubicin due to a poor chemotherapeutic response with the former regimen. There was no difference in the incidence of chemotherapy associated complications such as grade 1 or greater peripheral neuropathy and tinnitus between the 2 groups (Table 4). EBRT was delivered as postoperative treatment to 78.6% women in the PCS group.
3.4 Survival analysis
The median period of follow-up was 24 months (range 14 - 72 months). 13 out of 16 (81.3%) patients in the NACT group had relapsed or shown progression of disease and 7 out of 16 (43%) women were alive at the endpoint of this analysis. The cause of death of all patients in the NACT cohort was disease progression. 21 out of 28 (75 %) patients in the PCS group had evidence of disease relapse or progression and 11 out of 28 (39%) women were alive at the conclusion of the survival assessment. The cause of death was disease progression in all but one out of 21 women. She died following a cerebrovascular accident.
Median progression free interval was 12 months in the NACT group vs 15 months in the PCS group (p value 0.59). Median overall survival was noted to be 33 months in patients who received NACT and 27 months in the PCS group (p value 0.77). There was no statistically significant difference in both progression free survival and overall survival between the 2 groups in the study.
4. Discussion
Advanced endometrial cancer accounts for more than 50 % of all uterine cancer related deaths, with 5 year survival rates as low as 5-17.5% [10]. Conventionally, patients with advanced disease are treated by aggressive cytoreduction followed by adjuvant chemotherapy or with systemic treatment alone [11]. The use of an alternative strategy incorporating NACT followed by interval debulking surgery was first reported in 1996 by Resnik et al. in a case of presumed unresectable uterine papillary serous carcinoma (UPSC) [12]. Vandenput et al. reported that high rates (80%) of optimal cytoreduction were achieved when neoadjuvant chemotherapy was used to treat patients with extensive intraabdominal metastases in UPSC [8]. Rabinovich in 2016 summated that only 106 cases of NACT were documented in the last 2 decades [11]. Our study adds to this limited body of evidence and represents a retrospective analysis of the survival and surgical outcomes of patients who were individualised to receive NACT versus outcomes of patients who had upfront cytoreductive surgery followed by chemotherapy/EBRT for treatment of stage IIIC/IV endometrial cancer.
Our study represents a small number of patients and is consistent with the rare presentation of advanced stage disease. The cohort is comparable to the sample size of Wilkinson-Ryan et al. who reported on similar outcomes in 10 patients with UPSC and Vandenput et al. who presented results of a prospective study of 30 women who received NACT [8,13]. We included all histological variants of endometrial cancer in contrast to the 2 studies above as Ayeni et al. demonstrated that histologic subtype was not an independent predictor of survival in stage III/IV disease for both serous and grade 3 endometrioid tumours, suggesting similar biologic aggressiveness and parallel responses to therapeutic algorithms [14]. Studies showed longer median overall survival with endometrioid tumours but in our study, there was a comparable distribution of grade 1 and 2 endometrioid tumours in the 2 groups (18% NACT vs 21% PCS) [15].
Optimal cytoreduction to microscopic residual status has been reported to be the single most important variable influencing the survival outcomes of patients undergoing treatment of advanced endometrial cancer [4,16-18]. No significant difference was noted in the residual disease status between our 2 groups (31.2 % NACT vs 39.3% PCS). The rate of optimal cytoreduction to less than or equal to 1cm residual disease was noted to be 69% in the NACT group in our study, which is approaching the 80% optimal cytoreduction achieved in the study of Vandenput et al. [8]. No overall significant difference was noted in surgical outcomes between the 2 groups.
An important rationale for adopting a neoadjuvant approach is to limit serious operative morbidity associated with undertaking surgery with radical intent. Vandenput et al. reported a minor postoperative morbidity rate of 13% which is comparable to the 18% (3 patients) noted in the NACT cohort in our study. We had no serious postoperative morbidity. However, the incidence of serious postoperative morbidity was 4% in Vandenput study and 13% in the study of Bristow et al. This higher incidence of serious morbidity in the Bristow study is directly attributable to the radicality of surgical work i.e. small bowel resections, partial hepatectomy and splenectomy [4] undertaken with primary upfront surgery.
Doxorubicin-based regimens were the mainstay of chemotherapy treatment for advanced endometrial cancer for more than 2 decades [19]. GOG 209 is a phase III randomised trial that revealed similar PFS and OS rates but a statistically significant reduction in the incidence of grade 2 or greater toxicity with the usage of Carboplatin and Paclitaxel regimens [20]. Currently, the combination of Carboplatin and Paclitaxel is considered the standard treatment for advanced endometrial cancer with response rates of 50% or higher. Vandenput et al. showed that a high chemotherapeutic response score correlated strongly with better progression-free survival and overall survival in patients with endometrial cancer [8]. The chemotherapeutic response as judged by RECIST criteria in our group was not significantly different to the Vandenput study for the demonstration of at least a partial response (93% NACT group).
There was no significant difference in progression-free survival between the 2 groups and the finding of 12 months PFS in the NACT group is similar to that of Wilkinson-Ryan et al (10.4months PFS in NACT vs 12 months in PCS) and that of Vandenput et al. (13 months PFS). However, the median overall survival was 33 months in our NACT arm of the study compared to 23 months in the study of Vandenput et al. This higher median survival might be attributable to the inclusion of all epithelial histological types in our study. Whilst the numbers in this study are small to make definitive conclusions it can be stated that the OS compares favourably to data in available literature on OS in patients who have had either PCS or NACT for advanced endometrial cancer. This includes data from the Eto study showing a median overall survival of 21 months [21].
5. Conclusion
This study has shown that women considered inoperable due to advanced disease are able to undergo surgery with cytoreductive intent following NACT and indeed achieve equivalent rates of cytoreduction as those with upfront surgery. It might be extrapolated that similar rates of cytoreduction have translated into similar overall and progression free survival rates in both groups. The limitations of this study are its retrospective nature and small sample size from a single institution. This study adds to the growing evidence exploring and comparing the survival and operative outcomes with use of neoadjuvant chemotherapy in advanced endometrial cancer. Prospective clinical trials investigating the role of NACT in isolation and in comparison with upfront surgery are recommended to provide conclusive evidence [22].
Competing Interests
The authors declare that they have no competing interests.
Author Contributions
S Rajkumar was responsible for the concept and design of the article, performed the literature search, collected the clinical data, performed the final analysis and wrote the manuscript. A Winship supervised data interpretation, contributed to study design, critical analysis and final revision of manuscript. R Nath and G Lane contributed to study design, critical analysis of final manuscript. A Sayasneh, G Mehra , V Mullassery contributed to interpretation of data and critical revision of manuscript and Paul Seed to statistical analysis and interpretation of data in this study.