1. Background
Breast cancer remains the common cancer to target women in Australia [1]. Adjuvant radiotherapy (RT) has become the mainstay treatment after breast conserving surgery for invasive cancer and postmastectomy radiotherapy, boasting a reduction of local recurrence from 26% to 7% at 5 years follow-up. This same study revealed an absolute risk reduction of 5.4% in breast cancer-related mortality with radiation therapy after breast conserving surgery (BCS) compared to BCS alone [2]. As with any treatment, radiation therapy has its side-effects – multiple studies have linked left breast irradiation to increased cardiac mortality and morbidity [3–5]. Darby et al. found that the relative risk for ischaemic heart disease increased by 7.4% for every 1 Gray (Gy) increase in mean heart dose in a population base study involving 2168 patients [3].
There are many treatment techniques that have been used to minimize exposure to organs at risk (OAR) such as prone positioning, intensity-modulated radiotherapy (IMRT) and proton therapy. One of the most promising of these is the Deep Inspiration Breath Hold (DIBH). This involves the patient inspiring to a specific volume and holding their breath whilst receiving radiotherapy which displaces the heart and subsequently reducing the radiation it incurs. This technique has been widely recognized as an effective means of reducing radiation exposure to the heart without compromising the therapeutic dose to breast cancer tissue [6-15].
There are several different breath-hold techniques that have been utilized all over the world. One of the most common methods is via the spirometry-based Active Breathing Coordinator (ABC) system made by Elekta (Stockholm, Sweden). This device is a mouthpiece attached to a spirometer, the patient’s nose is pegged to prevent nasal respiration. The radiotherapist (staff member who runs the linear accelerator) is then able to monitor the patient’s inspiration volume and when it has reached a predetermined threshold pinch-valves activate to prevent the patient from exhaling or inhaling and the radiation dose is administered. This technique has been proven to be an effective method for DIBH [16–33].
One of the difficulties with this system is its cost, not only in the machine itself but with new mouthpieces and specialized training for staff. For some years this prevented widespread implementation of the Breath Hold Technique. The Voluntary Breath Hold was then conceived as a simple and inexpensive alternative to the ABC DIBH. The protocol that Bartlett et al. developed was the method we implemented in our study for VBH. There is considerable data comparing DIBH against free breathing radiotherapy in left sided breast cancer however there are limited trails comparing the efficacy of varying DIBH techniques. Bartlett et al. compared ABC assisted DIBH and voluntary DIBH in terms of setup reproducibility, normal tissue sparing and feasibility of delivery. Our study looks to further compare the efficacy of two different techniques of DIBH investigated in our centre – Active breathing coordinator (Elekta) and Voluntary breath hold with dosimetric endpoints.
2. Methods and Materials
Selection criteria involved women who were 70 years old or less, of performance status 0 or 1, with left sided breast cancer. Patients with poor function were excluded. They had to be fluent in English, had no hearing impairments and must be able to fit through the planning CT scan (size dependent). Patients had to be able to undergo device training and hold their breath at 50% greater capacity than their resting lung volume. 20 patients in total were selected, 10 assigned to ABC and 10 assigned to VBH.
Of the ABC cohort patients were able to receive adjuvant left breast or chest wall irradiation, and where indicated, supraclavicular, axillary, or internal mammary nodal (IMC) irradiation. VBH patients were only able to receive left breast orchest wall radiotherapy as we were unable to ensure an accurate setup in those patients that were recommended nodal irradiation.
Two comparable techniques were introduced - active breathing coordinator (using specialised Elekta equipment) and voluntary breath hold (without equipment following the Bartlett et al. protocol). All twenty patients underwent two CT simulation scans one in ‘Free Breathing (FB)’ and the other in ‘Breath-Hold’ (ABC or VBH). Treatment plans were generated using a tangential radiation therapy technique. A dosimetric comparison was made between the two plans for the heart, left lung and contralateral breast as per EviQ guidelines [34,35] . Measurements were collected for Lung V20 (%), Ipsilateral Lung Maximum Depth (cm), Heart V25 (%), Heart (Gy), and Contralateral Breast V3 (%). 9 patients had LAD mean values measured. Comparison was made, firstly, for FB against DIBH and then for ABC against VBH.
The Bartlett et al. protocol involved using the distance moved by anterior and lateral reference tattoos away from the treatment room lasers whilst in breath-hold. This allowed staff to monitor the consistency between the CT-planning stage and the treatment setup stage [36].
Patient suitability was first assessed with the aforementioned criteria. They were then asked to practice holding their breath at home whilst lying down, initially for 5 seconds building up to 20 seconds. During the planning CT scan stage, tattoos and CT markers were placed on the patient’s midline in free breathing and approximately half way along the likely field edges. Then lateral markers were added to the patients in free-breathing. The maximum duration for which the patients can hold their breath was measured. The position of the anterior and lateral tattoos was marked in relation to the lasers in breath-hold to help establish reproducibility. The light fields were measured and marked in the medial and lateral borders whilst in free-breathing and breath-hold. The field borders were marked on the skin to help with reproducibility. When administering radiotherapy the patient was instructed to breath hold and treatment was delivered when the light fields aligned satisfactorily with the marked field border. Twenty consecutive patients were offered and agreed to participate. They were randomly selected to either of the 2 study arms.
Radiation related clinical characteristics data were collected from a total of 20 patients (N=20). The clinical characteristics were recorded for all 20 patients after subjecting them to one of the DIBH techniques (ABC or VBH) in addition to Free breathing. Out of the 20 patients who were subjected to DIBH, 10 patients each were assigned to both the ABC and VBH techniques.
The Wilcoxon signed-rank test is a non-parametric statistical hypothesis test used when comparing two related samples. This test was used to compare the median values of the patient’s clinical characteristics for DIBH and Free breathing as both the techniques were used on the same set of patients.
The Mann-Whitney U test was used to compare the patient’s median values of the clinical characteristics for the ABC and the VBH techniques as both the techniques were used on a different set of patients. Only the statistically significant results have been reported.
Clinical characteristics have been described using summary statistics (mean and standard deviation (SD) or median and interquartile range (IQR)) depending on the distribution of the variable.
3. Results
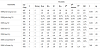
The results from the Shapiro-Wilk test of normality are summarised in tables 1 and table 2. These indicate that a substantial number of variables listed in table 1 and table 2 cannot be assumed to be from a normally distributed population (as the p-value of the Shapiro-Wilk statistic is less than .001). Therefore, subsequently, non-parametric statistics (i.e. Medians and Inter-quartile range) and techniques (e.g. Mann-Whitney U test) have been used to address the aims of the data analysis.
The summary statistics for the clinical characteristics of the patients for the DIBH and Free breathing techniques, and results from the Wilcoxon signed-rank test are shown in Table 3 below. The Wilcoxon test found that: the median Ipsilateral Lung maximum (cm) with the DIBH technique (Median=2.6, IQR=.58) was significantly more (Z=- 3.072, p=.002) than that of the Free breathing technique (Median=2.3, IQR=.78); the median Ipsilateral Lung V20 (the percentage of the lung volume which receives radiation doses of 20 Gy or more) with the DIBH technique (Median=12.33%, IQR=4.24%) was significantly less (Z=-2.576, p=.01) than that of the FB technique (Median=13.92%, IQR=11.03%); the median Lung V20 with the DIBH technique (Median=5.84%, IQR=1.34%) was significantly less (Z=-2.296, p=.022) than that of the FB technique (Median=6.45%, IQR=3.56%); the median Heart V25 (the percentage of the heart volume which receives radiation doses of 25 Gy or more) with the DIBH technique (Median=.26%, IQR=.46%) was significantly less (Z=-3.921, p<.001) than that of the FB technique (Median=2.41%, IQR=2.86%); the median Heart (Gy) with the DIBH technique (Median=1.43, IQR=.68) was significantly less (Z=-3.921, p<.001) than that of the FB technique (Median=2.7, IQR=1.78); and the median LAD mean (Left anterior descending artery measured in Gy) with the DIBH technique (Median=7.7, IQR=6.18) was significantly less (Z=-2.201, p=.028) than that of the FB technique (Median=23.4, IQR=9.7). There was no statistically significant difference between the median Contralateral Breast V3 (the percentage of the contralateral breast volume which receives radiation doses of 3 Gy or more) values of the DIBH and FB technique groups.
The summary statistics for the clinical characteristics of the patients for the ABC and VBH, and results from the Mann-Whitney U test are shown in Table 4 below. The Mann-Whitney U test found that: the median Heart (Gy) with the ABC technique (Median=1.44, IQR=.60) was significantly less (U=15.000, p=.008) than that of the VBH technique (Median=1.75, IQR=1.15); and the median Contralateral Breast V3 with the ABC technique (Median=0.00%, IQR=0.00%) was significantly less (U=24.500, p=.035) than that of the VBH technique (Median=0.31%, IQR=0.89%). None of the other differences between the median values for the clinical characteristics were significantly different between the ABC and VBH technique groups.
4. Data Analysis Summary
The results of the data analysis indicated that the Ipsilateral Lung maximum (cm) is significantly higher for the DIBH group implying DIBH to be a better technique compared to Free Breathing. This assertion is further supported by the following clinical characteristics being significantly lower for the Free breathing technique group: Ipsitlateral Lung V20, Lung V20, Heart V25, Heart (Gy), and LAD mean (Gy).
Additionally, the results of the data analysis indicated that the Heart (Gy) and the Contralateral Breast V3 (%) values were significantly higher for the VBH technique group compared to the ABC technique group. This indicates that ABC is a more effective technique compared to VBH as far as these clinical characteristics are concerned.
5. Discussion
Multiple population based studies have demonstrated the increased risk in cardiac mortality in patients who undergo left sided breast cancer radiotherapy [5,37-39]. The most recent Early Breast Cancer Trailists’ Collaborative Group meta-analyses showed that adjuvant RT after BCS reduces the rate of breath cancer mortality compared to surgery alone [40,41] . The significant reduction in breast cancer mortality that has been cited appear to diminish over time due to cardiotoxicity related to radiotherapy exposure. This has historically been difficult to assess since cardiac and pulmonary toxicities associated with radiotherapy are late-stage effects and lag decades after treatment has occurred. These results would not take into account the benefits accrued from modern radiotherapeutic techniques but also the deleterious effects of cardiac toxicity from chemotherapy [42]. This has led to the development of techniques to help reduce the radiation doses toadjacent organs-at-risk – including the deep inspiration breath hold.
Our study’s primary aim was to compare the efficacy of Active Breathing Coordinator (ABC) against Voluntary Breath Hold (VBH). There is minimal data present in the literature that compares these two techniques. Bartlett et al. studied 23 patients, who completed both VBH and ABC, and used Electronic Portal Imaging (EPI) values to determine positional reproducibility. They also measured heart, leftanterior descending coronary artery and lung doses and found that there was no statistical difference present. They found that VBH was preferred by patients and radiographers, takes less time to deliver and is cheaper than ABC [43]. The authors of this study also conceived the protocol that we used for our VBH.
We studied 20 patients who underwent both FB and DIBH. These patients were split randomly into 2 groups, 10 undertaking the ABC technique and 10 undertaking the VBH technique. Our data revealed similar results when comparing the efficacy of DIBH in reducing radiation doses to organs-at-risk against free breathing. There was, however, a statistically significant difference between the Heart (Gy) and Contralateral Breast V3 (%) between ABC and VBH. This showed that ABC was a more effective breath hold technique than VBH.
ABC is a more expensive technique when accounting for the equipment and the need to use a new mouthpiece for each patient. Specialized training is also required for radiotherapists to use the machinery and software. Patients must be able to follow commands and understand the concepts involved. This technique also has patient dependent limitations including claustrophobia and poor lung function. In contrast VBH is a simpler and cheaper technique to implement and is better tolerated by patients. In our cohort patients tolerated ABC DIBH very well and had no issues with compliance.
Our study’s results suggest that DIBH should be implemented as routine clinical practice for left sided breast cancer patients receiving radiotherapy as there is a clinically relevant dose reduction to cardiac structures. In addition to this ABC has been shown to be a superior breath hold technique and should be the technique of choice for DIBH. We found that using ABC was a more efficient approach once staff were trained adequately, the time taken per fraction was approximately 18 minutes compared to 25 minutes for VBH.
Deep Inspiration Breath Hold Technique reduces ipsilateral lung dose via inflation causing less tissue to remain in the irradiated region. It has been previously shown that the use of deep inspiration breath hold technique in breast cancer patients can reduce the mean lung dose by 15% and the Lung V20 by 17%, when compare to free breathing techniques [44].
Limitations to this study were population size and the single-centre nature of the study. Also at the time of writing this article measurements of LAD doses had not been determined in all 20 patients. The implications of potentially cardiotoxic chemotherapy can confound the data and was not considered in our study. Given that this was a dosimetric study, cardiac morbidity and survival were not evaluated. Clinical correlation with cardiac dose-volume parameters is required in the future to accurately predict the dose needed to reduce cardiac morbidity and mortality. It was demonstrated by Darby et al. that the rate of coronary event increases by 7.4% for every 1 Gy irradiated to the heart [4,45] .
There has been an impetus to measure radiotherapy related cardiotoxicity using Single Photon Emission Computer Tomography (SPECT) scans which allows us to detect adverse changes earlier. Prosnitz et al. demonstrated in one study that patients receiving left sided adjuvant radiation for breast cancer had detectable SPECT scan changes evident 3 to 6 years post-radiation therapy [46]. Most other cardiotoxic effects develop several yearsafter the initial radiotherapy. In the future this may be an option for more accurate measurements of irradiation of innocent structures.
Mittauer et al. showed that an Optical tracking system can be a valuable tool for real-time quality control of ABC-assisted DIBH [47]. This method will help increase precision and reproducibility of DIBH in turn reducing the irradiation of the heart.
Further studies are required to confirmthis data including larger study populations with varying co-morbidities and body habitus. Comparison of other breath-hold methods will help practitioners to select appropriate treatments amongst the myriad of options. Long term follow-up is required to fully determine the clinical outcomes associated with irradiation to the heart and lung. Additionally, further research should help develop more stringent patient-selection criteria. These studies should also target patient coaching and treatment verification protocols which will improve the efficiency and reproducibility of the technique.
6. Conclusion
In our study consisting of 20 patients undergoing left sided breast cancer radiotherapy we showed that DIBH was a superior means of administering radiotherapy than free breathing. In addition to this we demonstrated that ABC was a superior breath hold technique when compared to VBH. Future studies are required to confirm our findings.
Competing Interests
The authors declare that they have no competing interests.