1. Introduction
Sepsis is a major healthcare problem, with high incidence and poor mortality outcome [1]. The Surviving Sepsis Campaign (SSC) was first launched in 2002 with the goals of increasing clinician and public awareness of the sepsis problem, enhancing the standard of care and decreasing mortality [2]. The SSC Guidelines for management of severe sepsis and septic shock were first published in 2004 [3], providing recommendations that are intended to guide clinical practice. In order to facilitate the implementation of the guidelines, the key elements in the treatment of sepsis were organized into two bundles of care, the “resuscitation” and “management” bundle, including interventions to be accomplished within specified timeframes [4]. A bundle is a set of diagnostic or therapeutic processes that when implemented as a group may act synergistically, providing a greater survival benefit than each individual component.
Several published data show that performance improvement or implementation programs on compliance with sepsis bundles was associated with lower risk of death in patients with severe sepsis and septic shock [5,6]. Thus, On May 1, 2013, NYSDOH Title 10 New York Codes Rules and Regulations (NYCRR) Sections 405.2 and 405.4 were amended to require that hospitals have in place evidence-based protocols for the early recognition and treatment of patients with severe sepsis and septic shock that are based on generally accepted standards of care. Medical staffs were responsible for the collection, use, and reporting of quality measures related to the recognition and treatment of severe sepsis for purposes of internal quality improvement and hospital reporting to the department.
However, consistent adherence to sepsis bundles in the management of patients has remained a challenge. The purpose of this quality improvement project was to examine the outcome implications of implementing a sepsis intervention protocol to increase adherence to 3-hour and 6-hour bundle, and the impact on mortality in our emergency department.
2. Methods
2.1 Design, overview and setting
This quality improvement study was performed in the emergency department. Our study protocol was reviewed and approved by our Institutional Review Board (IRB) with a waiver of informed consent as the study was deemed a performance improvement intervention.
2.2 Patients
All adult patients who presented to the emergency department from September 2018 through June 2019, were screened for this project. Patients with severe sepsis or septic shock at the time of presentation as defined by Center for Medicare and Medicaid service, were identified through the use of a written screening guide (Figure 1).
2.3 Sepsis intervention protocol
ED physicians, nurses, CNA, pharmacists and lab technician were educated regarding implementation of time sensitive measures of sepsis bundles through lectures and monthly nursing orientation at the end of September through October of 2018 (Figure 2). Sepsis posters highlighting time sensitive measures were posted throughout the emergency department. Time sensitive measures in the 3-hour bundle include obtaining timely initial lactate level, administration of IV fluids at a rate of 30 ml/kg of body weight within 2 hours, and timely blood cultures draw prior to administration of antibiotics. In the 6-hour bundle, time sensitive measures include obtaining repeat lactate within 4 hours if initial lactate >2, assessing patient responsiveness to fluid resuscitation and prompt administration of vasopressors within 4 hours if patient is not responsive to fluid resuscitation.
An ED sepsis kit which included two liters of crystalloids, and a timer as reminder for timely re-measurement of lactate was created. Patients presenting to the ED who demonstrated clinical deterioration and met two or more criteria on the sepsis screening guide (thereby demonstrating that they were likely to have severe sepsis or septic shock) were intended to trigger a sepsis code (SIP=sepsis intervention protocol). Sepsis resuscitation and management bundle elements were implemented using a sepsis checklist to capture the above time sensitive measures to be completed by nurses and physicians (Figure 3). Checklist review process by Quality Assurance and Performance Improvement department along with ED leadership allowed for real time feedback.
3. Results
We analyzed data of cases of patients with severe sepsis and septic shock in our emergency department which were reported to the New York State Department of Health (NYSDOH) from 2017 Q2 to 2018 Q2 (April 2017 - June 2018), the period prior to implementation of SIP. We compared the results to data from 2018 Q3 to 2019 Q2 (July 2018 to June 2019) the period after implementation of SIP. A total of 512 cases of patient with severe sepsis and septic shock was reported, of which there were a total of 180 deaths during the time under review for this project.
A demographic analysis of hospital data pre and post implementation of SIP showed a higher proportion of patient aged 70 to 79 years (about 24 to 26% of total number of cases) constituting the majority of patients with severe sepsis or septic shock. Of note, 88.4 to 88.6 % of total number of cases in our hospital were African Americans compared to statewide averages of which only 15.9 to 16.3% were African Americans. A mild gender difference was also noted with female patient constituting a slightly higher majority (of 50.2 to 53.6%) compared to (46.4 to 49.8%) of male cases in our hospital. The reverse situation was noted when comparing statewide data which showed a slightly higher male to female percentages (Table 1a & 1b).
As show in the trend percentages in figure 4, prior to 2018 Q3 our hospital percentages of timely lactate level, timely blood culture prior to antibiotic administration and timely re-measurement of lactate level in sepsis cases, were below statewide percentages. Consequently, 3-hour and 6-hour bundle adherence percentages were also below statewide averages (Figure 4e & 4f). Of note however, timely broadspectrum antibiotic administration was similar or above statewide percentages.
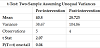
The implementation of SIP in 2018 Q3, resulted in improved adherence and performance of the sepsis bundle (Figure 4). Consequently, a clinically significant reduction of the mean preintervention hospital percent mortality of 40.3% to a mean postintervention hospital percent mortality of 28.7% was observed (Figure 5). Furthermore, as shown in Table 2, a two-sample t-test analysis of the mean hospital percent mortality before and after implementation of SIP demonstrated a reduction in mortality outcome that was statistically significant (p<0.05).
4. Discussion
This quality improvement project demonstrates that an evidencebased protocol for the early recognition and treatment of patients with severe sepsis and septic shock is an effective tool for increasing compliance with sepsis resuscitation and management bundle elements as its primary outcome. The use of a sepsis checklist by health care providers after the implementation of SIP in October 2018 significantly improved performance bundle elements. The most remarkable finding in this project was the statistically significant reduction in mortality outcomes of patient with severe sepsis and septic shock since implementation of the SIP.
We did not perform a statistical analysis of each bundle elements to assess if the improved trended percent performance of these elements upon implementation of SIP were statistically significant. Furthermore, we noted that timely broad spectrum antibiotic administration were also above or similar to statewide percentages before and after implementation of SIP. The timeliness of antibiotic administration has been proven to decrease mortality. Thus, reducing antimicrobial burden by early antibiotic administration not only decreases mortality in septic shock, but also decreases pressor/ inotrope free days, and ventilator days [7-11]. However, the findings of this quality improvement project demonstrates that improved performance of bundle elements in addition to prompt antibiotics administration results in decrease mortality outcomes.
For example, elevated lactate results from hypoperfusion of tissues. Decreased perfusion to tissue affects mitochondrial oxidative phosphorylation thereby shifting energy metabolism to anaerobic glycolysis and the production of serum lactic acid [6]. Animal models have shown that a delay in antibiotic administration following the onset of hypotension and hypoperfusion of tissues is associated with an increase in inflammatory mediators [12]. Therefore, timely measurement of lactate levels may alert providers to perfusion abnormalities that may prompt therapeutic changes such as prompt intravenous fluid and broad spectrum antibiotic administration.
5. Conclusion
In conclusion, early intervention protocols for medical emergencies with an extremely high mortality rate such as Code STEMI for patients with ST-segment elevation myocardial infarctions have demonstrated an improved rate of survival with early recognition and implementation of appropriate therapy. Severe sepsis and septic shock are medical emergencies with an extremely high mortality rate. A sepsis intervention protocol (SIP) as demonstrated in this project can be useful in severe sepsis and septic shock as it increases completion of time-sensitive measures via the use of a sepsis checklist, compliance with bundle elements and improves mortality outcomes. The SIP was easy to implement, essentially without cost, improved compliance with sepsis bundle and mortality outcomes, making it an attractive tool for institutions to consider when meeting the goals of early goal-directed therapy for severe sepsis and septic shock.
Competing Interests
The authors declare that they have no competing interests.
Acknowledgments
This work is supported, in part, by the efforts of Dr. Moro O. Salifu M.D., M.P.H., M.B.A., M.A.C.P., Professor and Chairman of Medicine through NIH Grant number S21MD012474.