1. Introduction
In the United States, stroke is one of the top 5 leading cause of death, in addition to being a leading cause of adult disability [2-4]. An estimated 140,000 people die annually in the US as a direct result of a stroke, leaving roughly 795,000 to suffer the consequences of disabilities, giving rise to considerable economic loss and social issues [1,2,4,5]. Research shows that 63% of patients who experience an acute stroke or transient ischemic attack manifest obstructive sleep apnea (OSA) having an Apnea-Hypopnea index (AHI) score greater than 10 [6]. Obstructive sleep apnea (OSA), a condition in which patients experience recurrent apnea and hypopnea episodes due to complete or partial collapse of the upper airway [7]. The repeated cessations of breathing (apneas) and slow or shallow breathing (hypopneas) during sleep that characterize OSA are accompanied by sleep disturbances, hemodynamic changes and heighten thrombotic potential. Mechanisms of pathology in OSA that are important to consider include sympathetic activation, intra-thoracic pressure changes and oxidative stress. Additionally, endothelial damage with subsequent platelet activation and increased systemic inflammation potentiating vasoconstriction are implicated in the atherosclerotic process and are important factors to consider in disease progression. Hypoxemia appears to drive these pathways [8]. It is for these reasons that OSA is a strong risk factor for hypertension (including resistant hypertension), coronary artery disease, renal disease, heart failure, arrhythmias and stroke [3,4,7,9-11].
An important particularly vulnerable sub-group within black populations with OSA are black patients with metabolic syndrome. Metabolic Syndrome (MetS) is a constellation of clinical and metabolic risk factors that include abdominal obesity, dyslipidemia, glucose intolerance, and hypertension. In general, blacks have lower prevalence of MetS when compared to whites, but suffer disproportionately from higher cardiovascular mortality and type two diabetes mellitus [12]. It is unclear whether OSA and metabolic syndrome work synergistically within the black population to place this vulnerable sub-group at an even greater risk of stroke. Studies have speculated, that OSA may create and/or intensify the pre-existing negative components of metabolic syndrome (MetS), suggesting OSA to play a vital role in the pathogenesis of metabolic dysfunction [13]. There is a surprising lack of research regarding the risk of OSA and stroke among blacks with MetS. Given the increased risk of morbidity and mortality associated with OSA, and the undeniable economic burden this places on the US healthcare system, this study sought to investigate blacks with MetS and their risk for OSA and stroke within the Metabolic Syndrome Outcome (MetSO) trial.
2. Method
Data were collected as part of the Metabolic Syndrome Outcome study (MetSO), an NHLBI funded registry of 1035 blacks with metabolic syndrome in a primary-care setting in four clinics associated with SUNY Downstate Medical Center in Brooklyn, NY. During the data collection period 875 patients were enrolled during the time of analysis. Validated questionnaires were administered in order to obtain data on sleep apnea risk, day time sleepiness, demographic, anthropometric data, and diseases associated with risk for sleep apnea (i.e. hypertension, diabetes, heart disease, and stroke) (Allscripts, Sunrise Enterprise).
Patients were diagnosed with metabolic syndrome using the National Heart, Lung and Blood Institute and the American Heart Association guidelines. According to these guidelines, metabolic syndrome is diagnosed when a patient has at least three of the following five conditions: 1) fasting glucose ≥ 100 mg/dl or receiving treatment for hyperglycemia, 2) blood pressure ≥ 130/ 85 mmHg or receiving drug therapy for hypertension, 3) triglycerides ≥ 150 mg/ dl or receiving drug treatment for hypertriglyceridemia, 4) HDLC< 40mg/dl in men or <50 mg/dl in women or receiving drug therapy for HDL-C and 5) a waist circumference ≥ 102 cm (40 in) in men or ≥ 88 cm (35 in) in women [14]. Physician-diagnosed conditions were obtained using an electronic medical record (EMR) system (Allscript, Sunrise Enterprise). We used the Apnea Risk Evaluation System (ARES) to identify individuals who were at OSA risk because of its accuracy in evaluating populations with a large pretest OSA probability. Data solicited included socio-demographics, diseases associated with OSA, the Epworth Sleepiness Scale (ESS), and frequency of breathing abnormalities. The ESS questionnaire has a sensitivity of 0.94, specificity of 0.79 (based on a clinical cut-off of AHI > 5), positive predictive value of 0.91 and negative predictive value of 0.86.
3. Statistical Analysis
Frequency and measures of central tendency were used to describe the sample. In preliminary analyses, Pearson and Spearman correlations were used to explore relationships between variables of interest. A multivariate-adjusted logistic regression modeling was also used. Covariates entered in the model include age, sex, obesity (defined as BMI > 30 kg/m2), history of diabetes, dyslipidemia, hypertension and a measured waist circumference. Data were processed by an experienced Biostatistician using SPSS 20.0 (Chicago, SPSS Inc.).
4. Results
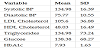
The study revealed 93% of the sample were diagnosed with hypertension; 61%, diabetes; 72%, dyslipidemia; 90% were overweight/ obese; 33% had a history of heart disease and 10% had a stroke. ARES data indicated that 48% were at high OSA risk. Logistic regression analysis, adjusting for age and gender, showed that patients at risk for high OSA had a nearly three-fold increase in odds of having a stroke (OR = 2.79, 95% CI: 1.64-4.73).
5. Discussion
Results from this study revealed blacks with MetS had a 48 percent increased risk of OSA that accompanied a nearly three-fold increase in odds of having a stroke. In an observational cohort study, OSA was associated with stroke and death (hazard ratio, 1.97; 95 percent confidence interval, 1.12 to 3.48) [13,15-18]. Similar, findings were noted in the Vitoria Sleep Project, where it was determined that elderly patients with OSA were at a higher risk for stroke (hazard ratio [HR] =2.52, 95 % CI, 1.04-6.01, P = 0.04) [13]. OSA seemingly increases the intensity of “The Perfect Storm”, vascular comorbidities such as hypertension; atrial fibrillation and atherosclerosis have been proven to contribute the increase risk of stroke [13].
In patients with no medical history of OSA a 10%-15% nocturnal drop of blood pressure is usually experienced, however in patients with OSA the protective effect of nocturnal blood pressure dipping is lost [18]. As a result, during an apneic episode, hypoxia can induce vasodilatation or a reflex cerebral vasoconstriction, a mechanism that can lead to a stroke [13].
Although OSA plays a role in the progression of many diseases, it is uniquely important within the context of stroke. The prevalence of sleep apnea in stroke patients has been shown to be as high as 50-70% [16]. OSA is a predictor of both poor functional outcomes after a stroke and post-stroke mortality [19]. It is thought that poor cerebral blood flow from changes in blood pressure and oxygen saturation during apneic episodes affect the neurological recovery after cerebrovascular events. A greater than 50% reduction in middle cerebral artery blood flow velocity has been demonstrated by transcranial doppler studies during obstructive apneas and hypopneas [8]. A 2018 study showed that patients with more severe OSA as defined by the apnea-hypopnea index (AHI) demonstrated significantly increased levels of calcified carotid arterial plaques (CCAP) on panoramic imaging compared to patients with lower AHI scores, an important validated risk factor for future adverse cerebrovascular and cardiovascular events (OR = 1.035; CI, 1.008-1.062; P = .010). The same study also found almost a third of patients with OSA were found to have CCAP panoramic imaging [20].
Studies have shown that blacks that are obese are more prone to develop OSA [13,15]. Additionally, obesity has been proven to be a top contributor to the development of MetS in blacks [21]. During an apneic hypopneic episode, sleep duration is altered, sleeping <6 hrs or >8 hrs; researchers have propositioned the idea of prolong sleep occurring as an attempt to compensate for fragmented sleep [13,16]. In addition, short and long sleep perpetuated by OSA has been linked to increase in stroke mortality and cardiovascular diseases [22,23]. Furthermore, blacks with MetS experience an increase in endothelial and microvascular damage [24].
Research has suggested the role of endothelial inflammation and damage to play a violent role regarding the pathophysiology of a stroke; resulting in thrombosis, due to increase D-dimers, fibrinogens, inflammatory markers and endothelial progenitor cells. Chu et al 2008, set out to investigate the microvascular environment of endothelial progenitor cells (EPC) in 75 patients with acute stroke, 45 patients with chronic stroke and 40 patients deemed healthy with no history of stroke [24]. It was found that endothelial progenitor cells (EPC) was demonstrated in 71% of patients with acute stroke, 22% with chronic stroke and 10% of those healthy, concluding that endothelial cell injury and dysfunctions are predictors of increased risk of a vascular event [6,24]. Research has shown that both MetS and OSA can alter the microvascular environment [24-26] . A turbulent endothelial environment to increase the risk of stroke [27], furthermore the MetSO trial, the largest clinical trial to date of this kind, has provided unique insight of how blacks with MetS are 1) at increased risk for OSA and 2) the combination of both OSA and MetS may contribute significantly to increase risk of stroke in the black population.
6. Conclusions
As research continues to increase patient and physician awareness of OSA, a deeper appreciation of the detrimental long-term consequences of diagnosing and treating OSA have increased in popularity. As it stands, the most predominate risk factor for MetS is obesity, which is also a dominate risk factor for OSA. Both MetS and OSA contribute to the destruction of the microvascular environment increasing the risk of stroke. Prevention and control is of the utmost importance, modification of risk factors such as obesity is an important public health concern.
Competing Interests
The authors have read the journal’s policy and have the following potential conflicts: All authors declare that they have no proprietary, financial, professional, nor any other personal interest of any nature or kind in any product or services and/or company that could be construed or considered to be a potential conflict of interest that might have influenced the views expressed in this manuscript.
Contributors
All authors intellectually contributed to the design, analysis, and interpretation of the results and to drafting the critical review of manuscript. All authors reviewed and approved the final version of the manuscript.
Acknowledgments
This research was supported by funding from the National Institutes of Health: R25HL105444, R01HL095799, RO1MD004113, and U54NS081765. The funding source had no role in the design, conduct, or analysis of the study, or in the decision to submit the manuscript for publication.
Abbreviations